Introduction
Aneurysmal bone cyst (ABC) was first reported by
Jaffe and Lichtenstein in 1942 (1).
The term was used to describe the ‘blow out’ radiographic
appearance and blood filled contents of the cystic spaces (2). In pathology, ABCs are destructive,
expansile bone lesions characterized by a reactive proliferation of
connective tissue containing multiple blood-filled cavities.
Presumably due to the local hemodynamic disturbances, the process
arises de novo in bone or is engrafted on pre-existing bone lesions
histologically identifiable in 30% of cases (3). ABC occurs predominantly in children
and young adults, mainly involving the long bones and the vertebrae
(4). The rib is a rare location for
ABC. The size of the majority of cases that have been reported in
the literature is <10 cm. The present study describes the case
of a huge ABC of the rib presenting in a 17-year-old male, which
was successfully treated by surgical resection. Written informed
consent was obtained from the patient.
Case report
A 17-year-old male was admitted to the Chinese
People’s Liberation Army (PLA) General Hospital (Beijing, China)
with a chief complaint of progressive right-sided chest pain and
chest distress for two months. There was no history of trauma,
fever or respiratory embarrassment accompanying the pain and mass.
On physical examination, the right posterior chest wall in the
region of the seventh rib bulged to a minimal degree, but it was
not tender to palpation. The respiratory sounds were slightly
decreased on the right side.
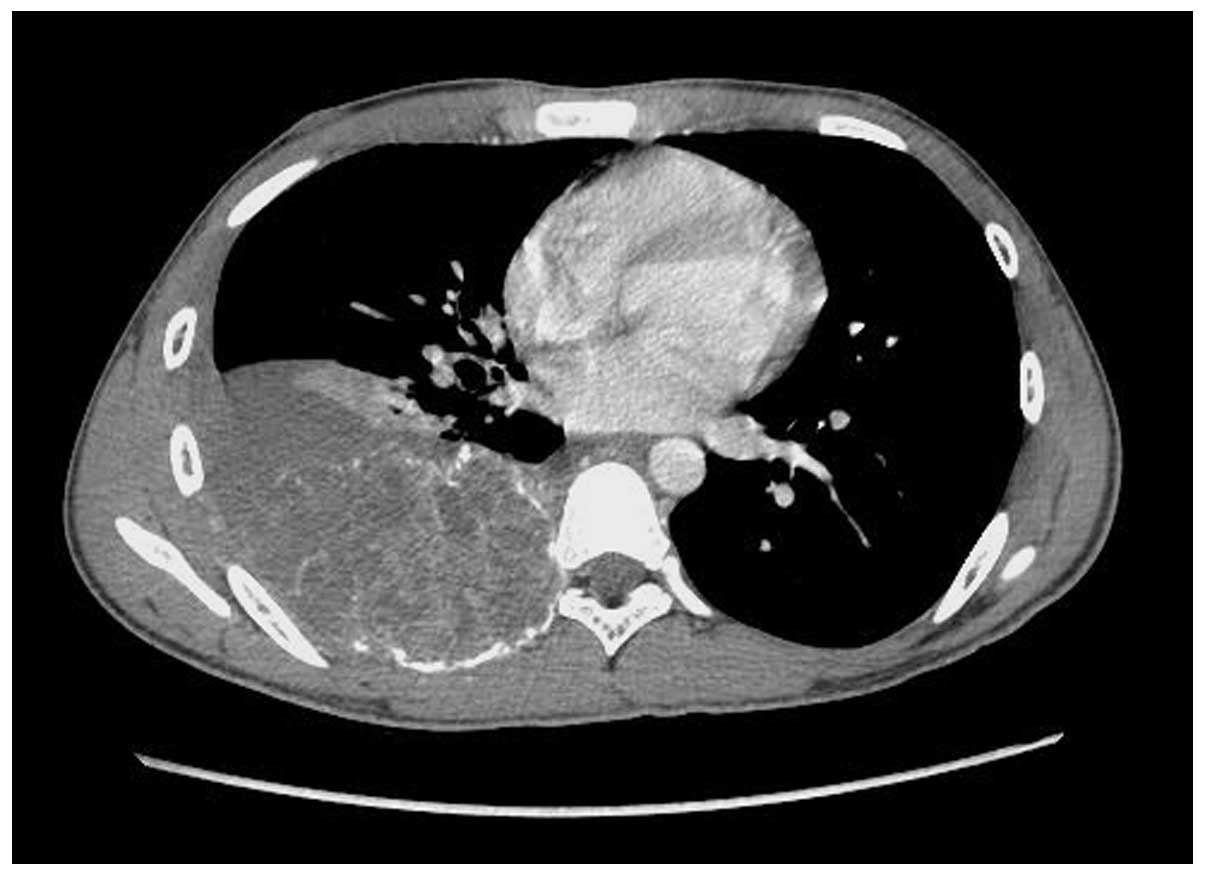
Plain and lateral chest radiographs revealed a
posterior chest mass on the right side. Computed tomography (CT) of
the chest revealed an irregular-shaped 12×10×10-cm tumor beside the
7th thoracic vertebra, which occupied almost half of the chest
cavity. A mottled calcification was observed in the core of tumor.
The tumor was mildly enhanced in the contrasted scan. The mass had
expanded and destroyed the posterior part of 7th rib. Atelectasis
of the right lower lobe and pleural effusion were also observed in
the CT (Fig. 1).
CT-guided aspiration biopsy pre-operatively
demonstrated that a neoplasm of spindle cell, solitary fibrous
tumor of the pleura was possible. As the CT findings suggested the
possibility of a malignant lesion, including sarcoma, surgery was
performed on June 3, 2011.
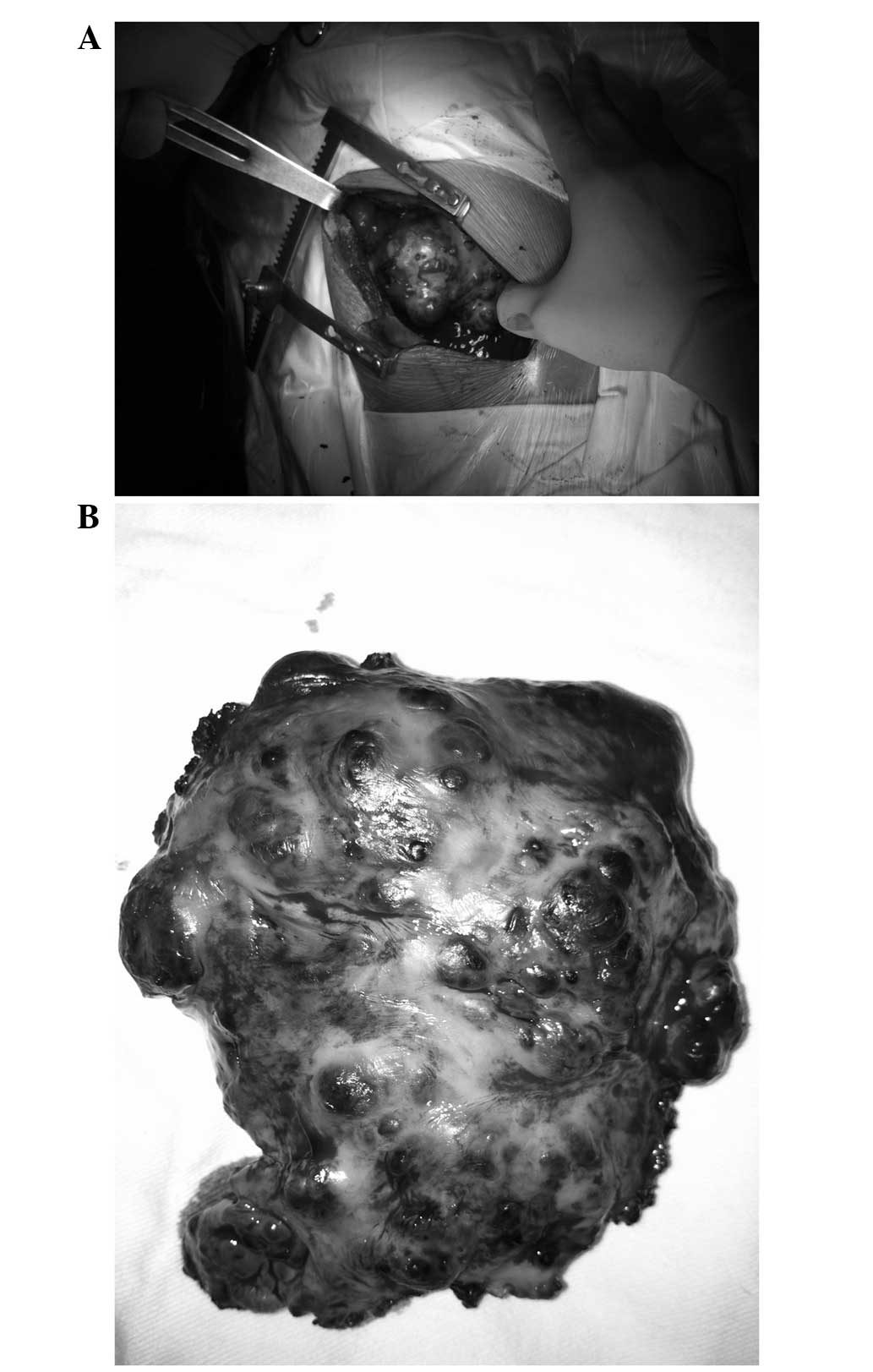
A right-sided thoracotomy revealed a 12×10-cm mass
that originated from the posterior half of the 7th rib, which was
medium-hard in texture. Numerous blood-filled cysts protruded from
the surface of the mass, and an abundant blood supply was observed
in the margin of the tumor (Fig.
2). The main vessels leading into the mass were sutured. Due to
a broad-base pedicle and poor exposure, the mass was excised
totally en bloc with the affected part of the 7th rib first. Other
adjacent parts of the rib, including the periosteum and adjacent
intercostal muscles, were subsequently resected.
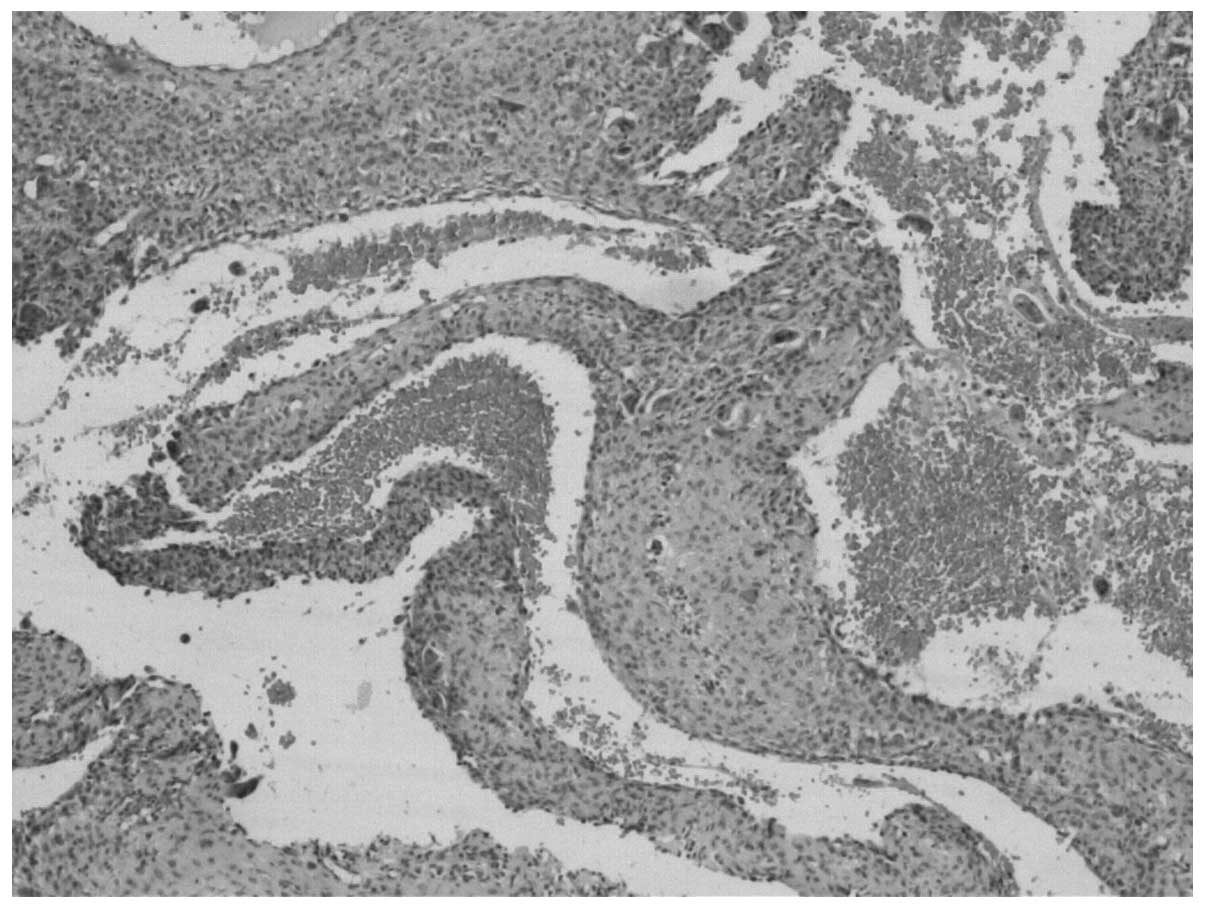
The microscopic examination demonstrated multiple
blood-filled cavernous spaces that were separated by fibrous
connective tissue, with hemosiderin pigment-laden macrophages,
multinucleated osteoclastic giant cells and well-developed vascular
spaces with hemorrhages in the septa lining the cystic spaces.
There were focal areas of calcification and osteoid. The surgical
margin was free. All these pathological findings were consistent
with those of an ABC (Fig. 3).
The patient was discharged following an uneventful
12-day postoperative period, and has been followed up for two years
with no evidence of recurrence.
Discussion
Primary rib neoplasms comprise 5–7% of all primary
bone tumors (5). ABC was first
described by Jaffe and Liechtenstein in 1942 (1), and accounts for only 1.3% of all bone
tumors. Therefore, ABC originating from the rib is particularly
rare. An ABC may occur in every rib with the exception of the lower
three (6). Although ABC
predominantly occurs in people aged <30 years old and equally
between genders, ABC of the rib is observed at an average age of
22.8 years and is marginally more frequent in females.
The etiology of ABC is unclear. Certain studies have
considered the condition to be secondary to an increased
circulatory venous pressure or trauma, causing bone absorption and
blood-filled cyst formation, thus explaining the expansile nature
of ABC (3). Alternatively, it is
proposed that ABC may be secondary to other pre-existing bone
diseases, including fibrous dysplasia, giant cell tumor and
non-ossifying fibroma, and is called ‘secondary ABC’ (7). Approximately one-third of all cases
are the secondary type.
The most common symptoms in a patient with ABC of
the rib are chest pain, swelling of the chest wall, dyspnea,
paraplegia and pathological fractures (6). Some patients with ABC of the rib have
an asymptomatic clinical course. These patients may be diagnosed
incidentally by chest X ray or CT. Infants with ABC of the rib may
also present with respiratory distress.
Although the radiological appearance of ABC of the
rib is not sufficiently specific to establish a definitive
diagnosis, a CT scan is of great value to demonstrate the
characteristic findings of the disease. CT may aid in showing a
destructive pattern of rib lesions with a ‘soap bubble’ or
‘honeycomb’ appearance (2,8). The differential diagnosis of ABC may
include Ewing sarcoma and eosinophilic granuloma, among others
(9). Core needle biopsy specimens
have been used to confirm the diagnosis, and their careful
performance is recommended as they may increase the risk of
bleeding due to the abundant blood cysts inside the ABC (10).
Grossly, the lesion is a cavity separated by septa.
The spaces usually contain blood or serum. The macroscopic
pathological findings tend to show a paper-thin cortex that is
usually intact unless there has been a complicated pathological
fracture. Under this shell, the bone is completely destroyed and
replaced by various sizes of cysts containing blood or serum. In
the present study, the cysts were separated by septa composed of
loosely arranged spindle cells and benign giant cells. Cuboidal
appearing cells line the cysts, and beneath this layer, osteoid
tissue with osteoblasts are observed. Focal calcifications may also
be evident (3,11).
Regarding the treatment of ABC, various methods have
been described, including surgery, radiotherapy, embolization,
cryotherapy, sclerotherapy and a wait-and-see strategy. To date,
the ideal treatment option is total excision, as it has the lowest
risk of local recurrence (12). An
incomplete removal may result in the persistence and growth of the
lesion. In addition, it is often difficult to obtain a precise
pre-operative diagnosis. Therefore, surgical treatment is
recommended, and complete local excision should be performed if
possible. Curettage of the lesion often results in recurrence
(11,13).
Radiotherapy should be considered only for
inoperable cases. Extreme care should be taken with regard to the
use of irradiation, as there is the possibility of a late
development of sarcoma (14).
Selective arterial embolization (SAE) has been reported as an
effective treatment for ABC and may be considered in lesions whose
site (spine or pelvis) or size make other types of treatment
difficult or hazardous. Certain studies have suggested that
embolization should be the first option for ABC treatment, as it
has the best cost-to-benefit ratio (12,15,16).
However, due to the lack of large feeding arteries to be embolized
in the ABC reported in the present case and the requirement for
repeated procedures as the sole therapy, embolization ought not to
be the standard therapy or a sole therapy. Pre-operative
embolization aids in controlling bleeding and minimizing the extent
of surgery that is required (17).
If pre-operative embolization had been performed in this case, the
procedure would have been smoother with less blood loss. SAE may be
a significant choice of treatment for certain ABCs and is a less
invasive, lower cost and simpler procedure that is easily
repeatable.
Dubois et al recommended sclerotherapy for
ABCs to avoid surgical risk and prolonged hospitalization, when the
clinical presentation and radiological appearances are typical
(18). The advantage of
sclerotherapy is that it is a minimally invasive, safer procedure.
Repetitive sclerotherapy using polidocanol or ethibloc injection
makes a considerable contribution to the therapeutic solution in
certain cases in which operative treatment is extremely hazardous
(19,20).
ABC arising from the rib is a rare, benign entity,
which should be considered in the differential diagnosis of chest
wall tumors. Complete surgical excision offers the best choice of
treatment for curing ABC.
Acknowledgements
The authors would like to thank Dr Zhigang Song,
Department of Pathology, Chinese PLA General Hospital, for
assistance and advice on the histopathological diagnosis.
References
|
1
|
Jaffe HL and Lichtenstein L: Solitary
unicameral bone cyst with emphasis on the roentgen picture, the
pathologic appearance and the pathogenesis. Arch Surg.
44:1004–1025. 1942. View Article : Google Scholar
|
|
2
|
Hughes EK, James SL, Butt S, Davies AM and
Saifuddin A: Benign primary tumours of the ribs. Clin Radiol.
61:314–322. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Martinez V and Sissons HA: Aneurysmal bone
cyst. A review of 123 cases including primary lesions and those
secondary to other bone pathology. Cancer. 61:2291–2304. 1988.
View Article : Google Scholar
|
|
4
|
Freidman B, Yellin A, Huszar M, Blankstein
A and Lotan G: Aneurysmal bone cyst of rib: a review and report of
two cases. Br J Dis Chest. 82:179–185. 1988. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Cappana R, Albisinni U, Picci P, Calderoni
P, Campanacci M and Springfield S: Aneurysmal bone cyst of the
spine. J Bone Joint Surg Am. 67:527–531. 1985.
|
|
6
|
Sabanathan S, Chen K, Robertson C and
Salama F: Aneurysmal bone cyst of rib. Thorax. 39:125–130. 1984.
View Article : Google Scholar
|
|
7
|
Kransdorf MJ and Sweet DE: Aneurysmal bone
cyst: concept, controversy, clinical presentation, and imaging. AJR
Am J Roentgenol. 164:573–580. 1995. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Soyer T, Karnak I, Talim B and Tanyel FC:
Aneurysmal bone cyst of the rib in a child: report of a case. Surg
Today. 35:886–889. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Andiran F, Ciftci AO, Senocak ME, Akcören
Z and Göğüs S: Chest wall hamartoma: an alarming chest lesion with
benign course. J Pediatr Surg. 33:727–729. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Cheng C, Yeung SC, Zhong FT, Xiong Y, Luo
HH, Ji S and Pan J: Aneurysmal bone cyst in the first rib. Ann
Thorac Surg. 85:2118–2120. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Ruiter DJ, van Rijssel TG and van der
Velde EA: Aneurysmal bone cysts: a clinicopathological study of 105
cases. Cancer. 39:2231–2239. 1977. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Cottalorda J and Bourelle S: Modern
concepts of primary aneurismal bone cyst. Arch Orthop Trauma Surg.
127:105–114. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Sadighi A, Tuccimei U and Annessi P:
Aneurysmal bone cyst of the rib: a case report. Chir Ital.
58:403–406. 2006.PubMed/NCBI
|
|
14
|
Tillman BP, Dahlin DC, Lipscomb PR and
Stewart JR: Aneurysmal bone cyst: an analysis of ninety-five cases.
Mayo Clin Proc. 43:478–495. 1968.PubMed/NCBI
|
|
15
|
Amendola L, Simonetti L, Simoes CE,
Bandiera S, De Iure F and Boriani S: Aneurysmal bone cyst of the
mobile spine: the therapeutic role of embolization. Eur Spine J.
22:533–541. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Rossi G, Rimondi E, Bartalena T, et al:
Selective arterial embolization of 36 aneurysmal bone cysts of the
skeleton with N-2-butyl cyanoacrylate. Skeletal Radiol. 39:161–167.
2010. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
An SY: Aneurysmal bone cyst of the
mandible managed by conservative surgical therapy with preoperative
embolization. Imaging Sci Dent. 42:35–39. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Dubois J, Chigot V, Grimard G, Isler M and
Garel L: Sclerotherapy in aneurysmal bone cysts in children: a
review of 17 cases. Pediatr Radiol. 33:365–372. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Rastogi S, Varshney MK, Trikha V, Khan SA,
Choudhury B and Safaya R: Treatment of aneurysmal bone cysts with
percutaneous sclerotherapy using polidocanol. A review of 72 cases
with long-term follow-up. J Bone Joint Surg Br. 88:1212–1216. 2006.
View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Lambot-Juhan K, Pannier S, Grévent D,
Péjin Z, Breton S, Berteloot L, Emond-Gonsard S, Boddaert N,
Glorion C and Brunelle F: Primary aneurysmal bone cysts in
children: percutaneous sclerotherapy with absolute alcohol and
proposal of a vascular classification. Pediatr Radiol. 42:599–605.
2012. View Article : Google Scholar
|