Introduction
Hepatocellular carcinoma (HCC) is the most frequent
histological diagnosis of primary liver cancer, the fifth most
prevalent type of cancer and the second most common cause of
cancer-associated mortality in males worldwide. It is also the
seventh most commonly diagnosed cancer and sixth greatest cause of
cancer-associated mortality in females worldwide (1). Prognosis for terminal-stage HCC is
poor, and the majority of patients succumb to the disease within
six months (2). Spontaneous
regression of cancer is defined as a partial or complete
disappearance of malignant tumors in the absence of specific
treatment (3). Spontaneous
regression of HCC is a rare condition and the underlying mechanism
of this phenomenon is unclear. The present study reports a case of
multiple lung, adrenal gland and lymph node metastases of recurrent
HCC with spontaneous complete regression, as revealed by tumor
markers and imaging studies. The patient provided written informed
consent.
Case report
A 64-year-old male patient was admitted to the
Division of Hematology and Oncology, Department of Medicine,
Dankook University Hospital (Cheonan, Korea) for treatment of
progressive dyspnea and cough. The patient had undergone right
lobectomy of the liver due to HCC at Severance Hospital (Seoul,
Korea) on October 23, 2006. At that time, the surgical specimen was
confirmed to be HCC, Edmondson grade II. After 14 months, a chest
computed tomography (CT) scan revealed multiple lung metastases and
left adrenal gland metastasis. The level of serum protein induced
by vitamin K absence or antagonist II (PIVKA II) was elevated
abnormally (207 mAU/ml). Diagnosed with recurrent HCC with multiple
lung metastases and adrenal metastasis, the patient received
palliative chemotherapy with 5-fluorouracil, adriamycin and
carboplatin. Following two cycles of first-line chemotherapy, the
disease progressed. The patient was administered two more cycles of
second-line chemotherapy with 5-fluorouracil, etoposide and
carboplatin, and three cycles of third-line chemotherapy with oral
capecitabine. However, the disease demonstrated no objective
response and further progressed. The patient and physician agreed
to discontinue cytotoxic chemotherapy, and the patient was
transferred to Dankook University Hospital for paliative care on
February 19, 2009.
The patient was a chronic hepatitis B virus carrier
and an older brother had hepatitis B viral liver cirrhosis. Initial
laboratory data from our hospital was as follows: White blood cell
count, 4,970 cells/μl; hemoglobin level, 17.2 g/dl; platelet
count, 16.4×104 platelets/μl; aspartate aminotransferase
: alanine aminotransferase level, 32:41 IU/l; total bilirubin
level, 0.97 mg/dl; gamma guanosine triphosphate level, 17 IU/l;
alkaline phosphatase level, 89 IU/l; protein : albumin level,
8.4:4.3 g/dl; prothrombin time (international normalized ratio),
13.2 sec (1.14); α-fetoprotein (AFP) level, 16.55 ng/ml (normal
range, 0–15 ng/ml); and PIVKA II level, 12,900 mAU/ml (normal
range, 0–40 mAU/ml). Hepatitis B virus DNA polymerase chain
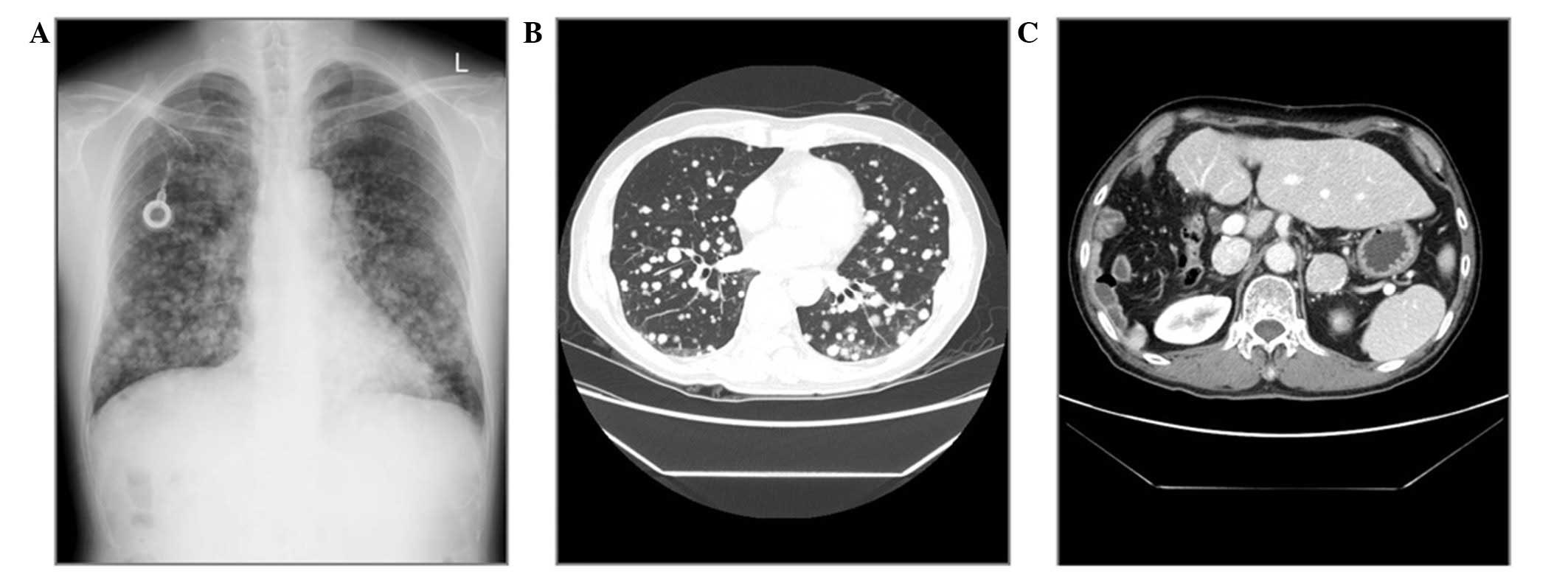
reaction test results were positive. At the time of admission, a
chest radiograph of the patient revealed miliary nodules in the
entirety of the lungs. CT scan of the chest and abdominopelvis
indicated miliary metastases throughout the lungs, bilateral
adrenal metastases and metastatic abdominal lymph nodes (Fig. 1). The patient was observed at
regular three-monthly follow-ups. After the first three months, the
patient continued to exhibit cough and dyspnea, and there was no
definitive interval change of the multiple lung metastases on the
chest radiograph. At the second visit on September 14, 2009, the
general condition of the patient had improved, and the cough and
dyspnea had stopped. A chest radiograph revealed that all
metastatic nodules had disappeared (Fig. 2). Serum AFP level had decreased to
1.5 ng/ml. Spontaneous tumor regression of HCC was observed, and
whole-body positron emission tomography-CT scan in December, 2009
revealed that all metastatic nodules in the lung, as well as the
metastatic lesions of the two adrenal glands and lymph nodes, had
disappeared. The patient had taken an alternative herbal medicine
for approximately one week, on the recommendation of his family.
The herbal medicine was Dendropanax morbifera Leveille,
which is a subtropical, broad-leaved evergreen tree belonging to
the family Araliaceae (4).
Follow-up CT scans revealed no recurrent lesions,
and follow-up chest radiograph also indicated no metastatic
lesions. Serum AFP and PIVKA II levels were within the normal range
(Fig. 3). The patient is alive
without any symptoms or signs as of May 2013.
Discussion
The present study reports a rare case of spontaneous
complete regression of hepatitis B virus-associated HCC. This
phenomenon is consistent with spontaneous regression of cancer as
defined by Everson and Cole (3).
Spontaneous regression has been described in numerous types of
tumors, particularly renal cell carcinoma, melanoma and
neuroblastoma. The incidence of spontaneous regression of cancer is
difficult to identify, but it has been estimated to occur in 1 in
60,000–100,000 cancer patients (5).
Epstein and Leung reported that spontaneous regression of HCC
appears to be more frequent than that of other types of cancers
(6), and Oquinena et al
reported that spontaneous regression is not an extraordinary event
among patients with HCC (7).
Nonetheless, spontaneous complete regression and long-term survival
in HCC is extremely rare. In a PubMed search, the present study
identified ≥60 reported cases of spontaneous regression of HCC
(7–11). Despite several reported cases of
spontaneous regression of metastatic HCC, to our knowledge, this is
the first case of spontaneous complete regression of a massive HCC
with multiple metastatic organs.
No exact mechanism for the spontaneous regression of
HCC is known. Several factors have been proposed, including
abstinence from alcohol, disruption of tumor blood supply from
subintimal vascular injury during angiographic procedures, use of
herbal medications, vitamin K, androgens, anti-estrogen therapy,
sepsis, fever and blood transfusion (3,45,12–18). Even following
detailed examination of all published cases of spontaneous
regressing HCC, precise conclusions concerning the mechanisms of
spontaneous regression remain unclear.
In the present report, no blood transfusion was
performed, and during the follow-up period there was no use of
hepatic angiography. There was no history of gastrointestinal
bleeding or infection in this patient. As the patient was a social
drinker, but had already stopped drinking alcohol at the initial
diagnosis of the disease, abstinence from alcohol was not
associated with the spontaneous regression.
The patient had taken an alternative herbal
medicine: The extracts from Dendropanax morbifera Leveille
(Korean name: Hwangchil tree), which is a subtropical, broad-leaved
evergreen tree belonging to the family Araliaceae. Previous studies
have demonstrated that Dendropanax morbifera Leveille has
anticomplement activity, antiatherogenic activity and antidiabetic
effects (19–21). Although the herbal medicine may be
associated with regression of HCC, it cannot be concluded that the
use of this particular herbal medicine affected the regression of
HCC in the present case, as there is no study on the antitumor
effects of Dendropanax morbifera Leveille, and the patient
had taken the herbal medication on only a few occasions during a
relatively short time period. The patient received no specific
antitumor treatment, nor had any known factors that effect HCC
regression. Therefore the regression of HCC presented in this
report can be described as truly spontaneous.
In conclusion, spontaneous tumor regression is an
interesting phenomenon, and spontaneous regression of HCC is rare
but not unknown. Although the mechanism of spontaneous regression
of HCC remains unclear and differs from patient to patient,
collation and further discussion of such cases will help to advance
the understanding of the phenomenon.
References
|
1
|
Jemal A, Bray F, Center MM, Ferlay J, Ward
E and Forman D: Global cancer statistics. CA Cancer J Clin.
61:69–90. 2011. View Article : Google Scholar
|
|
2
|
Llovet JM, Fuster J and Bruix J: Prognosis
of hepatocellular carcinoma. Hepatogastroenterology. 49:7–11.
2002.
|
|
3
|
Everson TC and Cole WH: Spontaneous
regression of cancer: preliminary report. Ann Surg. 144:366–380.
1956. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Kim SH, Jang YS, Han JG, Chung HG, Lee SW
and Cho KJ: Genetic variation and population structure of
Dendropanax morbifera Lev. (Araliaceae) in Korea. Silvae Genet.
55:7–12. 2006.
|
|
5
|
Cole WH: Efforts to explain spontaneous
regression of cancer. J Surg Oncol. 17:201–209. 1981. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Epstein RJ and Leung TW: Reversing
hepatocellular carcinoma progression by using networked biological
therapies. Clin Cancer Res. 13:11–17. 2007. View Article : Google Scholar
|
|
7
|
Oquiñena S, Guillen-Grima F, Iñarrairaegui
M, Zozaya JM and Sangro B: Spontaneous regression of hepatocellular
carcinoma: a systematic review. Eur J Gastroenterol Hepatol.
21:254–257. 2009.PubMed/NCBI
|
|
8
|
Meza-Junco J, Montano-Loza AJ,
Martinez-Benitez B and Cabrera-Aleksandrova T: Spontaneous partial
regression of hepatocellular carcinoma in a cirrhotic patient. Ann
Hepatol. 6:66–69. 2007.PubMed/NCBI
|
|
9
|
Arakawa Y, Mori H, Ikegami T, Hanaoka J,
Kanamoto M, Kanemura H, et al: Hepatocellular carcinoma with
spontaneous regression: report of the rare case.
Hepatogastroenterology. 55:1770–1772. 2008.PubMed/NCBI
|
|
10
|
Del Poggio P, Mattiello M, Gilardoni L,
Jamoletti C, Colombo S and Zabbialini G: The mysterious case of
spontaneous disappearance of hepatocellular carcinoma. Dig Liver
Dis. 41:e21–e25. 2009.PubMed/NCBI
|
|
11
|
Park HS, Jang KY, Kim YK, Cho BH and Moon
WS: Hepatocellular carcinoma with massive lymphoid infiltration: a
regressing phenomenon? Pathol Res Pract. 205:648–652. 2009.
View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Lam KC, Ho JC and Yeung RT: Spontaneous
regression of hepatocellular carcinoma: a case study. Cancer.
50:332–336. 1982. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Cole WH: Relationship of causative factors
in spontaneous regression of cancer to immunologic factors possibly
effective in cancer. J Surg Oncol. 8:391–411. 1976. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
O’Beirne JP and Harrison PM: The role of
the immune system in the control of hepatocellular carcinoma. Eur J
Gastroenterol Hepatol. 16:1257–1260. 2004.
|
|
15
|
Johnson FL, Lerner KG, Siegel M, et al:
Association of androgenic-anabolic steroid therapy with development
of hepatocellular carcinoma. Lancet. 2:1273–1276. 1972. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Markovic S, Ferlan-Marolt V and Hlebanja
Z: Spontaneous regression of hepatocellular carcinoma. Am J
Gastroenterol. 91:392–393. 1996.
|
|
17
|
Sato Y, Fujiwara K, Nakagawa S, et al: A
case of spontaneous regression of hepatocellular carcinoma with
bone metastasis. Cancer. 56:667–671. 1985. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Tocci G, Conte A, Guarascio P and Visco G:
Spontaneous remission of hepatocellular carcinoma after massive
gastrointestinal haemorrhage. BMJ. 300:641–642. 1990. View Article : Google Scholar
|
|
19
|
Chung IM, Song HK, Kim SJ and Moon HI:
Anticomplement activity of polyacetylenes from leaves of
Dendropanax morbifera Leveille. Phytother Res. 25:784–786.
2011.PubMed/NCBI
|
|
20
|
Chung IM, Kim MY, Park WH and Moon HI:
Antiatherogenic activity of Dendropanax morbifera essential
oil in rats. Pharmazie. 64:547–549. 2009.
|
|
21
|
Moon HI: Antidiabetic effects of
dendropanoxide from leaves of Dendropanax morbifera Leveille
in normal and streptozotocin-induced diabetic rats. Hum Exp
Toxicol. 30:870–875. 2011. View Article : Google Scholar : PubMed/NCBI
|