Introduction
Bleomycin is a chemotherapeutic antibiotic. Its mode
of action is to block DNA uptake of thymidine in the S-phase of the
cell cycle. Since it was first developed in Japan in 1966 (1), it has been used most commonly in the
treatment of Hodgkin’s lymphoma, certain germ cell tumors (GCT) and
for the sclerosis of recurrent pleural effusions (2). Bleomycin is inactivated in the
majority of tissues by an enzyme, bleomycin hydrolase, which
cleaves the ammonia group from bleomycin. This enzyme is active in
all tissues, with the exception of skin and lung tissue, which may
account for these being the most common sites of toxicity.
Reported dermatologic adverse effects of bleomycin
include Raynaud’s phenomenon, hyperkeratosis, nail-bed changes and
palmoplantar desquamation. Flagellate erythema is an unusual rash
that appears as ‘whip-like’ linear streaks and occurs specifically
during bleomycin use. Bleomycin-associated flagellate erythema has
been reported since 1970 (3–5);
however, with the declining use of bleomycin, this adverse reaction
has become much less common in practice. In the present study, we
report a case of bleomycin-associated flagellate erythema with a
review of the associated literature.
Case report
In April 2013, a 42-year-old male was diagnosed with
stage IIIB testicular cancer in accordance with the American Joint
Committee on Cancer Staing Classification (6) at the Kangwon National University
Hospital (Chuncheon, Korea). The histology revealed
non-seminomatous germ cell tumor (NSGCT) comprising seminoma (60%),
yolk sac tumor (25%), embryonal carcinoma (10%) and teratoma (5%).
Following orchiectomy, serum α-fetoprotein (αFP) levels were 20
ng/ml and lactate dehydrogenase (LDH) levels were 298 U/l (normal,
<190 U/l). Computed tomography (CT) scanning showed pre- and
para-aortic lymphadenopathy ≤3.6 cm. There was no medical history
of note and, specifically, no history of dermatological disorders
or allergy. The pateint’s pulmonary function test results were
normal. The patient was commenced on bleomycin, etoposide and
cisplatin chemotherapy, intravenously from May 20, 2013 in the
outpatient clinic. Bleomycin (30 units) was scheduled to be
administered on days 2, 9 and 16, while etoposide (100
mg/m2) and cisplatin (20 mg/m2) were
administered for 5 days from day 1. Treatment was intended to be
repeated every three weeks. After 10 days from the start of
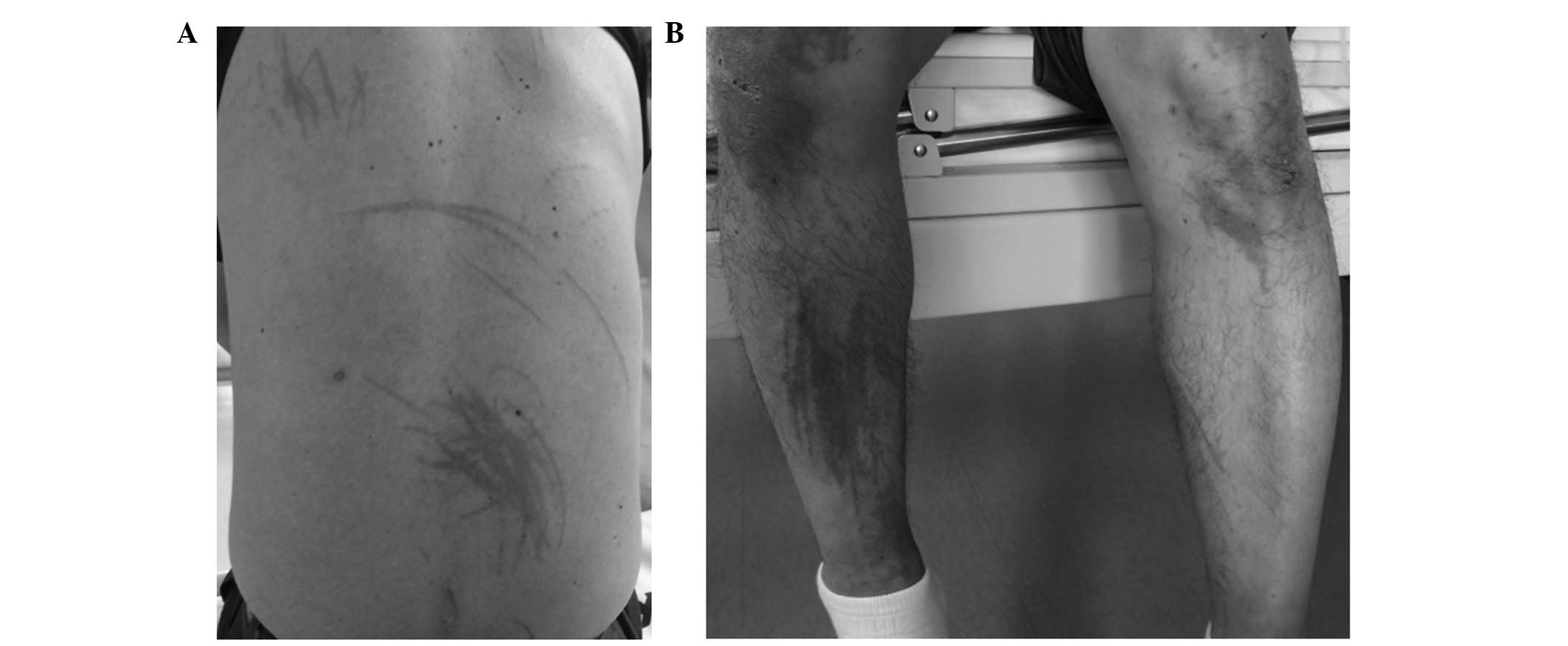
treatment, the patient subsequently developed a generalized
pruritus and erythematous linear rash that was most prominent on
the trunk and upper and lower extremities. The patient visited the
emergency room (ER) and was given antihistamine. The patient then
revisited the clinic for bleomycin treatment on day 16, and the
rash in which the patient appeared to have been whipped over
multiple body areas was observed. Physical examination showed the
appearance of an erythematous popular rash on the whole body, with
evidence of dermatographia (Fig.
1). There were no scales or lichenification, and the patient’s
vital signs were normal. Laboratory tests at ER showed a white
blood cell count of 3,800/mm3 (normal range,
3,800–10,000/mm3) (segmented neutrophils, 70%;
lymphocytes, 24%; and eosinophils, 3%), hemoglobin levels of 13.7
g/dl (normal range, 13.3–16.5 g/dl), a platelet count of
313,000/mm3 (normal range,
140,000–400,000/mm3), serum LDH levels of 208 U/l
(normal range, <190 U/l) and C-reactive protein levels of 5.35
mg/dl (normal range, <0.75 mg/dl). Prothrombin time and
activated prothrombin time were 11.5 (normal range, 12.1–14.5 sec)
and 36.7 sec (normal range, 31.0–43.7 sec), respectively.
A skin biopsy of a right forearm lesion was taken.
Bleomycin treatment on day 16 was cancelled. Pathological
examination of the skin biopsy showed endothelial swelling and
perivascular mononuclear cell infiltration present in the
superficial and deep dermis (Fig.
2). The findings were considered to be consistent with a
systemic hypersensitivity reaction. Given the patient’s clinical
history and the gross appearance of the lesions, the diagnosis was
most compatible with a severe bleomycin-induced flagellate erythema
reaction. The patient was commenced on a short course of oral
prednisolone, 20 mg daily, and antihistamine. The itching sensation
was improved, but mild hyperpigmentation remained.
Consequently, bleomycin was withheld from the
treatment regimen. As the patient’s NSGCT was intermediate-risk, we
recommended that the regimen should be changed to etoposide,
ifosfamide and cisplatin. However, the patient refused to add
ifosfamide following a discussion of the possible toxicities. Tumor
markers, such as αFP and LDH levels, were normalized within 3 weeks
of the first cycle of chemotherapy. Following a further three
cycles of etoposide 100( mg/m2, days 1–5) and cisplatin
(20 mg/m2, days 1–5), without bleomycin, every three
weeks, no remnant mass was visible in the abdomen on positron
emission tomography-CT.
Discussion
Diverse cutaneous reactions to bleomycin therapy are
common in the literature, and are reported as having an incidence
of 8 to 20% in patients receiving cumulative doses >100 units.
Bleomycin is associated with numerous dermatological toxicities,
such as alopecia, skin ulceration (predominantly plantar-palmar),
eczematous changes, erythematoid bulla, sclerodermoid lesions,
nail-bed changes and Raynaud’s phenomenon (7). Flagellate erythema is a less common
cutaneous toxicity of bleomycin, but is one with a strikingly
characteristic presentation.
The development of flagellate erythema appears to be
dose-independent, and flagellate erythema is considered to be a
reaction specific to bleomycin and is independent of the route of
administration or type of malignant disease being treated. The
lowest reported dose with systemic dermatologic complications is 15
units given intravenously (8).
Another report of low-dose bleomycin causing flagellate erythema
involved the intrapleural administration of 30 units of bleomycin
for the treatment of mesothelioma (9). Flagellate erythema may also occur at a
dose of <15 units intracutaneously (10).
Several hypotheses regarding the cause of
hyperpigmentation have been proposed. It has been proposed that the
linear lesions are induced by rubbing or scratching the skin, which
causes the drug to leak out of blood vessels. Alternatively, it has
been suggested that accumulation of bleomycin in the skin causes a
subsequent fixed drug eruption, due to the direct effects of
bleomycin on the keratinocytes. Histopathologically, the lesions
have shown a spectrum of morphological findings, including
urticarial hypersensitivity reaction (4), localized increase in melanogenesis
from hyperactive and enlarged melanocytes, inflammatory oncotaxis
(8) and lymphocytic vasculitis
(11).
The course of bleomycin-induced flagellate erythema
is varied. The majority of patients initially develop generalized
pruritus several hours to several weeks following the
administration of bleomycin. Erythematous linear streaks eventually
progress to the typical flagellate hyperpigmentation (8,9,12,13).
Onset of the characteristic lesions can occur anywhere from 1 day
to 9 weeks after bleomycin administration (14). There does not seem to be a
characteristic distribution as cases have shown involvement of the
face, trunk and extremities. Dermatographia is present to a limited
extent and the role of scratching in producing the linear shape of
the lesions has been debated (15).
However, studies have shown the clear appearance of linear streaks
in the absence of direct trauma (5). The majority of cases are reversible
following cessation of bleomycin; however, persistence of
hyperpigmented streaks for ≤1 year after treatment has been
reported (8,9,12).
There is no specific treatment for flagellate
erythema, which usually has a self-limited course of several weeks
to months, as long as bleomycin is subsequently avoided, although
permanent hyperpigmentation in affected areas is not unusual.
Occasionally, topical corticosteroids with or without oral
corticosteroids are required. Re-exposure to bleomycin may cause
further extension or recurrence of this rash and should be stopped
(16).
In summary, the present study describes a patient
with flagellate erythema following bleomycin administration.
Despite the declining use of bleomycin, clinicians should be aware
of this peculiar cutaneous manifestation. Therefore, we have
reported a characteristic feature of flagellate erythema with a
review of the associated literature.
Acknowledgements
This study was supported by a grant from the
National R&D Program for Cancer Control, Ministry for Health
and Welfare, Republic of Korea (grant no. 1020420).
References
|
1
|
Umezawa H: Bleomycin and other antitumor
antibiotics of high molecular weight. Antimicrob Agents chemother
(Bethesda). 5:1079–1085. 1965.
|
|
2
|
Chen J and Stubbe J: Bleomycin: towards
better therapeutics. Nat Rev Cancer. 5:102–112. 2005.
|
|
3
|
Simpson RC, Da Forno P, Nagarajan C and
Harman KE: A pruritic rash in a patient with Hodgkin lymphoma.
Bleomycin-induced flagellate dermatosis. Clin Exp Dermatol.
36:680–682. 2011.
|
|
4
|
Fyfe AJ and McKay P: Toxicities associated
with bleomycin. J R Coll Physicians Edinb. 40:213–215. 2010.
|
|
5
|
Chen YB, Rahemtullah A, Breeden E and
Hochberg EP: Bleomycin-induced flagellate erythema. J Clin Oncol.
25:898–900. 2007.
|
|
6
|
Edge S, Byrd DR, Compton CC, et al;
American Joint Committee on Cancer. AJCC cancer staging handbook.
7th edition. Springer-Verlag New York, Inc; New York, NY: pp.
539–546. 2010
|
|
7
|
Yamamoto T: Bleomycin and the skin. Br J
Dermatol. 155:869–875. 2006.
|
|
8
|
Cortina P, Garrdio JA, Tomas JF, Unamuno P
and Armijo M: ‘Flagellate’ erythema from bleomycin. With
histopathological findings suggestive of inflammatory oncotaxis.
Dermatologica. 180:106–109. 1990.
|
|
9
|
Fernandez-Obregon AC, Hogan KP and Bibro
MK: Flagellate pigmentation from intrapleural bleomycin. A light
microscopy and electron microscopy study. J Am Acad Dermatol.
13:464–468. 1985.
|
|
10
|
Abess A, Keel DM and Graham BS: Flagellate
hyperpigmentation following intralesional bleomycin treatment of
verruca plantaris. Arch Dermatol. 139:337–339. 2003.
|
|
11
|
Duhra P, Ilchyshyn A and Das RN:
Bleomycin-induced flagellate erythema. Clin Exp Dermatol.
16:216–217. 1991.
|
|
12
|
Templeton SF, Solomon AR and Swerlick RA:
Intradermal bleomycin injections into normal human skin. Arch
Dermatol. 113:577–583. 1994.
|
|
13
|
Watanabe T and Tsuchida T: ‘Flagellate’
erythema in dermatomyositis. Dermatology. 190:230–231. 1995.
|
|
14
|
Rubeiz NG, Salem Z, Dibbs R and Kibbi AG:
Bleomycin-induced urticarial flagellate drug hypersensitivy
reaction. Int J Dermatol. 38:140–141. 1999.
|
|
15
|
Lindae ML, Hu CH and Nickoloff BJ:
Pruritic erythematous linear plaques on the neck and
back‘Flagellate’ erythema secondary to bleomycin therapy. Arch
Dermatol. 123:395–398. 1987.
|
|
16
|
Mowad CM, Nguyen TV, Elenitsas R and
Leyden JJ: Bleomycin-induced flagellate dermatitis: a clinical and
histopathological review. Br J Dermatol. 131:700–702. 1994.
|