Introduction
Colorectal cancer (CRC) is the second most common
type of cancer in females and the third in males, worldwide
(1). It is also the second most
common cause of cancer-related mortality in the United States
(2). Approximately one third of
patients who develop CRC succumb to the disease (2). CRC is diagnosed in the majority of
patients following the onset of symptoms which include rectal
bleeding, a change in bowel habits, bowel obstruction and weight
loss, or following the identification of occult bleeding (3,4).
However, the implementation of CRC screening guidelines has
improved the detection of pre-malignant polyps and early-stage
asymptomatic CRC, and thus has improved disease outcomes (3,4). The
most prevalent sites of metastasis are the regional lymph nodes,
liver, lung, bone and brain (5). In
the present study, an extremely rare case of colon adenocarcinoma
with extensive metastasis to multiple mediastinal lymph nodes
without any other organ involvement is presented. The patient
provided written informed consent for the publication of this
study.
Case report
Patient presentation
This study presents the case of a 44 year-old
Caucasian male with a one-year history of waxing and waning
right-sided abdominal pain associated with a change in bowel
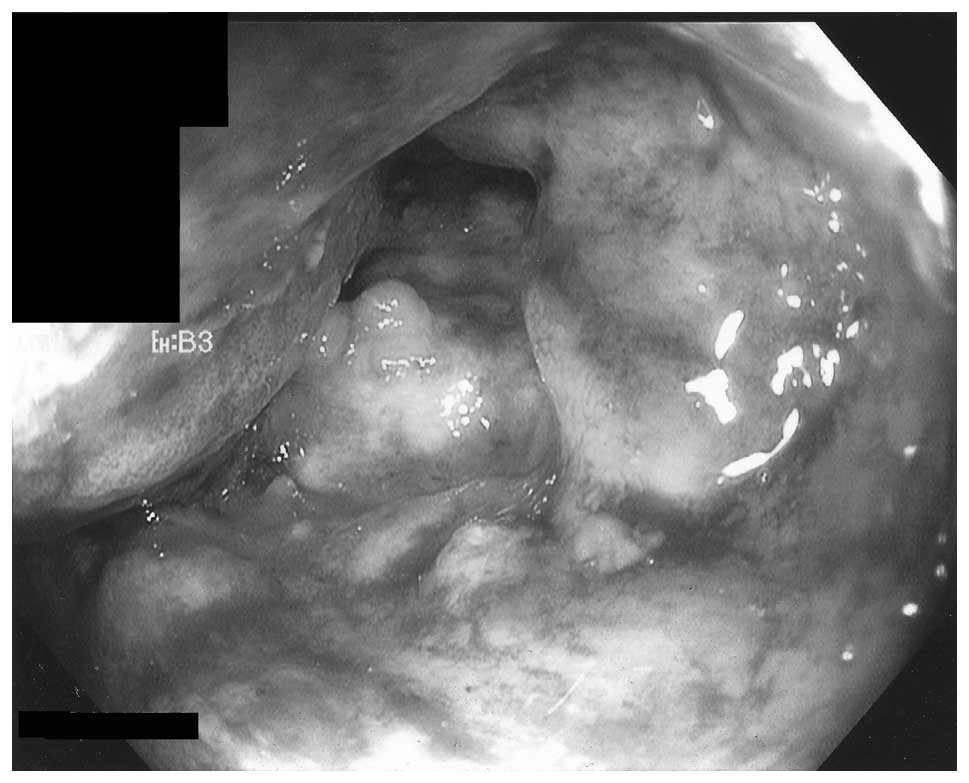
habits, melena and a weight loss of ~9 kg. Therefore, colonoscopy
was performed, which revealed a large, friable, ulcerated,
circumferential mass in the ascending colon, which was almost
completely obstructing the ascending colon and was unable to be
safely traversed with the colonoscope (Fig. 1). Biopsies were consistent with the
diagnosis of invasive moderately differentiated adenocarcinoma. The
level of carcinoembryonic antigen (CEA) in the patient’s blood was
found to be 3.0 ng/ml (normal range, <2.5 ng/ml).
Cancer staging
Computed tomography (CT) scans of the chest, abdomen
and pelvis were performed as part of the staging process of colon
cancer. Abdominal images revealed a large concentric mass involving
the ascending colon that extended ~7 cm in length with marked
narrowing of the colon, without causing complete obstruction
(Fig. 2). Retroperitoneal and
mesenteric lymphadenopathy were also observed. No liver pathology
was identified by CT. The CT scan of the chest revealed multiple
pathologically enlarged mediastinal lymph nodes with the largest
sizes exhibited by the pre-aortic lymph node (3.0×2.9 cm), a
precarinal lymph node (3.6×4.9 cm), a subcarinal lymph node
(5.2×3.5 cm) and a right hilar lymph node (3.3×5.2 cm), in addition
to bilateral smaller hilar lymph nodes (Fig. 3). No metastasis or other pathologies
was identified inside the lungs by CT.
Mediastinal lymph node involvement
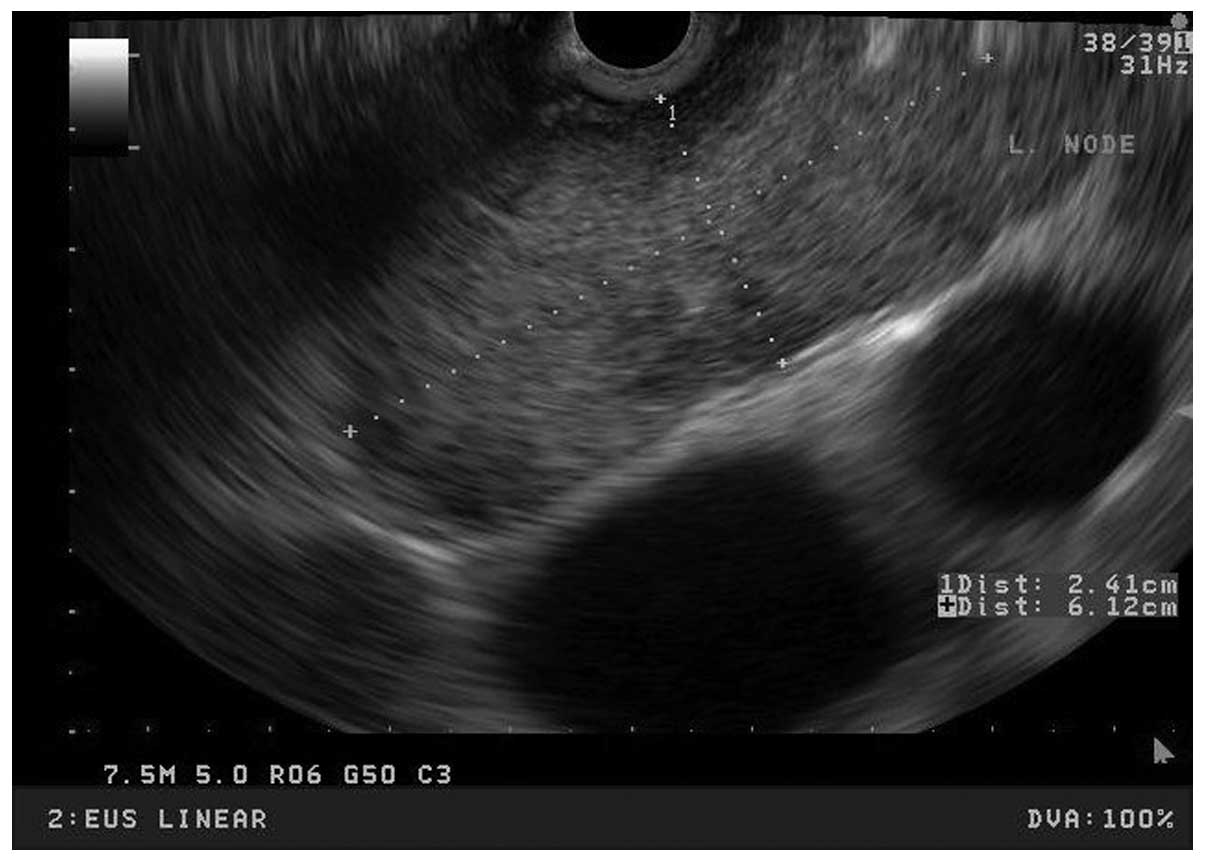
Endoscopic ultrasound (EUS) with fine-needle
aspiration was performed to exclude lymphoma. EUS did not reveal
any celiac lymphadenopathy; however, multiple enlarged mediastinal
lymph nodes were identified and the largest was located in the
subcarinal region (2.41×6.12 cm) (Fig.
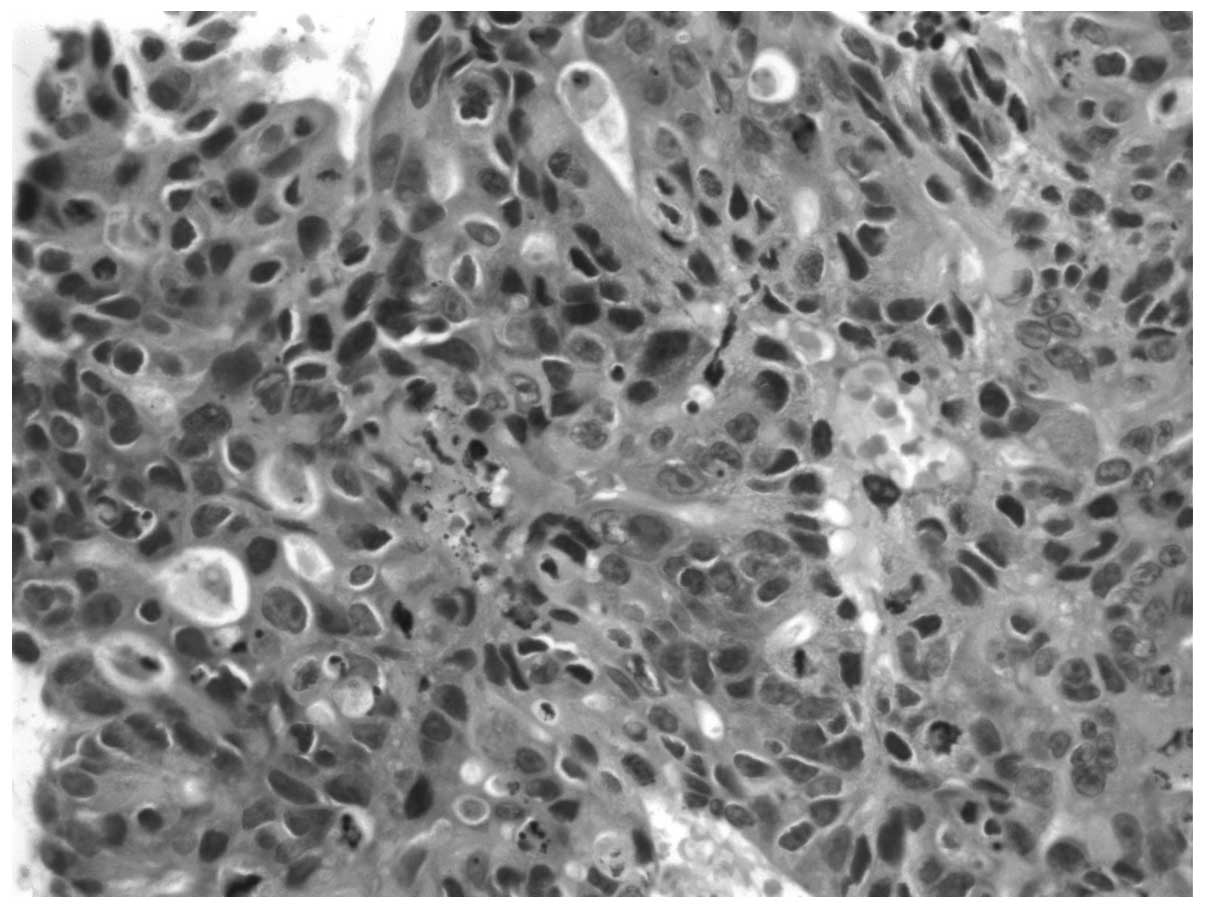
4). The pathology was again consistent with the diagnosis of
metastatic adenocarcinoma (Fig. 5)
and immunohistochemical staining of the core biopsy samples
revealed a cytokeratin 7 (CK7)-negative/CK20-positive pattern,
which is typical of colorectal primary carcinoma. Prior to
receiving the pathology results of the mediastinal lymph node
biopsies, the patient developed symptoms of colonic obstruction.
The patient was managed conservatively with bowel rest, and
continuous suctioning of the gastric contents via a nasogastric
tube. Obstructive symptoms were resolved after two days.
Colon resection
Following the pathological examination of the lymph
nodes the patient underwent right colon resection from the terminal
ileum proximally to the mid transverse colon distally. Pathology
results revealed moderately differentiated adenocarcinoma of the
right colon (largest tumor dimension, 7 cm), demonstrating invasion
of the muscularis propria with extensive infiltration of pericolic
fat and discontinuous extramural extension, prominent and extensive
lymph-vascular invasion, and metastatic involvement of 33 out of 52
regional lymph nodes. The circumferential (radial) resection margin
was positive and the proximal and distal margins were negative.
Chemotherapy and follow-up
The patient began chemotherapy treatment, and was
treated with eight cycles of folinic acid, fluorouracil and
oxaliplatin plus Avastin prior to developing peripheral neuropathy.
Therefore, the patient was administered infusional fluorouracil and
Avastin. The patient is alive one year following hemicolectomy.
Initial follow-up CT scans of the chest revealed a positive
response to chemotherapy with certain shrinkage of the mediastinal
lymph nodes after a small number of cycles. Nine months following
the diagnosis of CRC, CT scans revealed a stable disease and CEA
levels were observed to be 3.7 ng/ml.
Discussion
In summary, the patient exhibited a proximal colon
adenocarcinoma with extensive regional (retroperitoneal and
mesenteric) lymphadenopathy and distal metastasis to the
mediastinal lymph nodes without liver, lung or any other organ
involvement. This case demonstrated an extremely rare pattern of
colon cancer metastasis (5). It is
hypothesized that mediastinal involvement is usually a
re-metastasis from a previously metastasized site, such as the lung
or liver. The re-metastasis of colon cancer to the mediastinal
lymph nodes from lung metastasis is rare; however, it has been
reported in a small number of studies (6). Re-metastasis from the liver to lymph
nodes draining the liver is even rarer, but has also been reported
in the literature (7). Rashidi
et al (8) demonstrated,
using an orthotopic mouse model, that re-metastasis from the liver
to all of its draining lymphatic systems, including the portal,
celiac and mediastinal lymph nodes, is possible (8). However, re-metastasis from the liver
to the mediastinal lymph nodes in humans is extremely rare and has
been reported in only four cases in the literature (7,9–11).
Ovarian re-metastasis to the mediastinal lymph nodes also appears
to be possible; however, only a single case report exists that
describes this (12). Re-metastasis
to the mediastinal lymph nodes has also been reported in a single
patient with brain metastasis (13). However, direct colon metastasis to
the mediastinal lymph nodes without liver, lung or any other organ
involvement has been reported in a single case report by Musallam
et al (14), who
demonstrated solitary mediastinal lymph node involvement, in which
only one lymph node was involved. However, to the best of our
knowledge, the present study is the first to identify extensive
metastasis of colorectal adenocarcinoma to multiple mediastinal
lymph nodes without any other organ or site involvement. The exact
route of this metastasis is unclear. However, we hypothesize that
involvement of the mediastinal lymph nodes was via the para-aortic
lymphatic drainage route, or via ‘skip’ metastasis, as the patient
exhibited retroperitoneal peri-aortic lymph node involvement.
The optimal treatment option for metastatic colon
cancer to mediastinal lymph nodes is unclear, given the scarcity of
cases reported in the literature. Previous studies have reported
surgical resection of a solitary mediastinal lymph node with
positive outcomes (11), and
systemic treatment with chemotherapy with favorable outcomes
(14). However, in the present
case, due to multiple lymph node involvement being observed, the
lymph nodes were not surgically resected and chemotherapy was
administered instead. At present, the response appears favorable,
as the patient is alive one year following diagnosis. In
conclusion, physicians, in particular radiologists, must consider
the mediastinum during the first evaluation and further follow-up
of patients with colorectal carcinoma even in the absence of
metastasis.
References
|
1
|
Jemal A, Bray F, Center MM, Ferlay J, Ward
E and Forman D: Global cancer statistics. CA Cancer J Clin.
61:69–90. 2011.
|
|
2
|
Siegel R, Ma J, Zou Z and Jemal A: Cancer
statistics, 2014. CA Cancer J Clin. 64:9–29. 2014.
|
|
3
|
Levin B, Lieberman DA, McFarland B, et al:
American Cancer Society Colorectal Cancer Advisory Group; US
Multi-Society Task Force; American College of Radiology Colon
Cancer Committee: Screening and surveillance for the early
detection of colorectal cancer and adenomatous polyps, 2008: a
joint guideline from the American Cancer Society, the US
Multi-Society Task Force on Colorectal Cancer, and the American
College of Radiology. CA Cancer J Clin. 58:130–160. 2008.
|
|
4
|
U.S. Preventive Services Task Force.
Screening for colorectal cancer: U.S. Preventive Services Task
Force recommendation statement. Ann Intern Med. 149:627–637.
2008.
|
|
5
|
Hess KR, Varadhachary GR, Taylor SH, Wei
W, Raber MN, Lenzi R and Abbruzzese JL: Metastatic patterns in
adenocarcinoma. Cancer. 106:1624–1633. 2006.
|
|
6
|
Szöke T, Kortner A, Neu R, Grosser C,
Szilklavari Z, Wiebe K and Hofmann HS: Is the mediastinal
lymphadenectomy during pulmonary metastasectomy of colorectal
cancer necessary? Interact Cardiovasc Thorac Surg. 10:694–698.
2010.
|
|
7
|
August DA, Sugarbaker PH and Schneider PD:
Lymphatic dissemination of hepatic metastases. Implications for the
follow-up and treatment of patients with colorectal cancer. Cancer.
55:1490–1494. 1985.
|
|
8
|
Rashidi B, Gamagami R, Sasson A, Sun FX,
Geller J, Moosa AR and Hoffman RM: An orthotopic mouse model of
remetastasis of human colon cancer liver metastasis. Clin Cancer
Res. 6:2556–2561. 2000.
|
|
9
|
Vetto JT and Cohen AM: Isolated spread of
hepatic metastatic disease to a mediastinal lymph node. Report of a
case and review of pertinent anatomy and literature. Dis Colon
Rectum. 34:1128–1130. 1991.
|
|
10
|
Sano A, Murakawa T, Morota T and Nakajima
J: Resection of a posterior mediastinal metastasis of colon cancer.
Ann Thorac Surg. 92:353–354. 2011.
|
|
11
|
Iwata T, Chung K, Hanada S, Toda M, Nakata
K, Kato T and Miura T: Solitary bulky mediastinal lymph node
metastasis from colon cancer. Ann Thorac Cardiovasc Surg.
19:313–315. 2013.
|
|
12
|
Kuba H, Sato N, Uchiyama A, Nakafusa Y,
Mibu R, Yoshida K, Kuroiwa K and Tanaka M: Mediastinal lymph node
metastasis of colon cancer: report of a case. Surg Today.
29:375–377. 1999.
|
|
13
|
Tsubaki M, Nemoto K, Yoda N, et al:
Sigmoid colon cancer with mediastinal lymph node metastases. Int
Surg. 92:209–213. 2007.
|
|
14
|
Musallam KM, Taher AT, Tawil AN,
Chakhachiro ZI, Habbal MZ and Shamseddine AI: Solitary mediastinal
lymph node metastasis in rectosigmoid carcinoma: a case report.
Cases J. 1:692008.
|