Introduction
Laparoscopic minimally invasive surgical techniques
are not routinely adopted for the excision of retroperitoneal
tumors, which are often located adjacent to vital organs and blood
vessels. Indeed, minimally invasive surgery is even more rarely
adopted for retroperitoneal tumors that are located between the
vena cava and the abdominal aorta (1).
A pheochromocytoma (PHEO) is a type of catecholamine
(CA)-producing neuroendocrine tumor, which originates in the
chromaffin cells of the paraganglia. Worldwide, the incidence of
PHEO ranges between 0.005 and 0.1%. In total 10% of PHEOs occur at
extra-adrenal sites. Extra-adrenal paraganglionic tumors are termed
paragangliomas or extra-adrenal PHEOs (2) and are primarily derived from the organ
of Zuckerkandl proximal to the aorta. Diagnosis and therapy remain
complicated and there are no histological criteria for
distinguishing between benign and malignant tumors. Complete
surgical resection is the first choice approach. Radioactive
isotope treatment with [131I]-MIBG, systemic
chemotherapeutic intervention and genetic analysis under
development (3,4). Recently, laparoscopic surgery has
become the standard treatment for benign and malignant PHEO.
However, despite recent advancements, laparoscopy is limited by the
degree of motion that can be achieved by instruments (4,5). In
the current study, a preliminary report of results from a
robot-assisted minimally invasive surgical procedure on an
extra-adrenal PHEO, which was located between the abdominal aorta
and the inferior vena cava is presented. Written informed consent
was obtained from the patient.
Case report
Patient information
The patient was a 56-year-old female with a
five-year history of hypertension. The patient’s preoperative blood
norepinephrine (NE) and epinephrine (E) levels were 9,866.9 pg/ml
(normal range, 19.0–121 pg/ml) and 188 pg/ml (normal range,
14.0–90.0 pg/ml), respectively, which were accompanied by a
headache, palpitations and sweating. The highest blood pressure
reading was 240/110 mmHg (normal range, 100–120/60–80 mmHg).
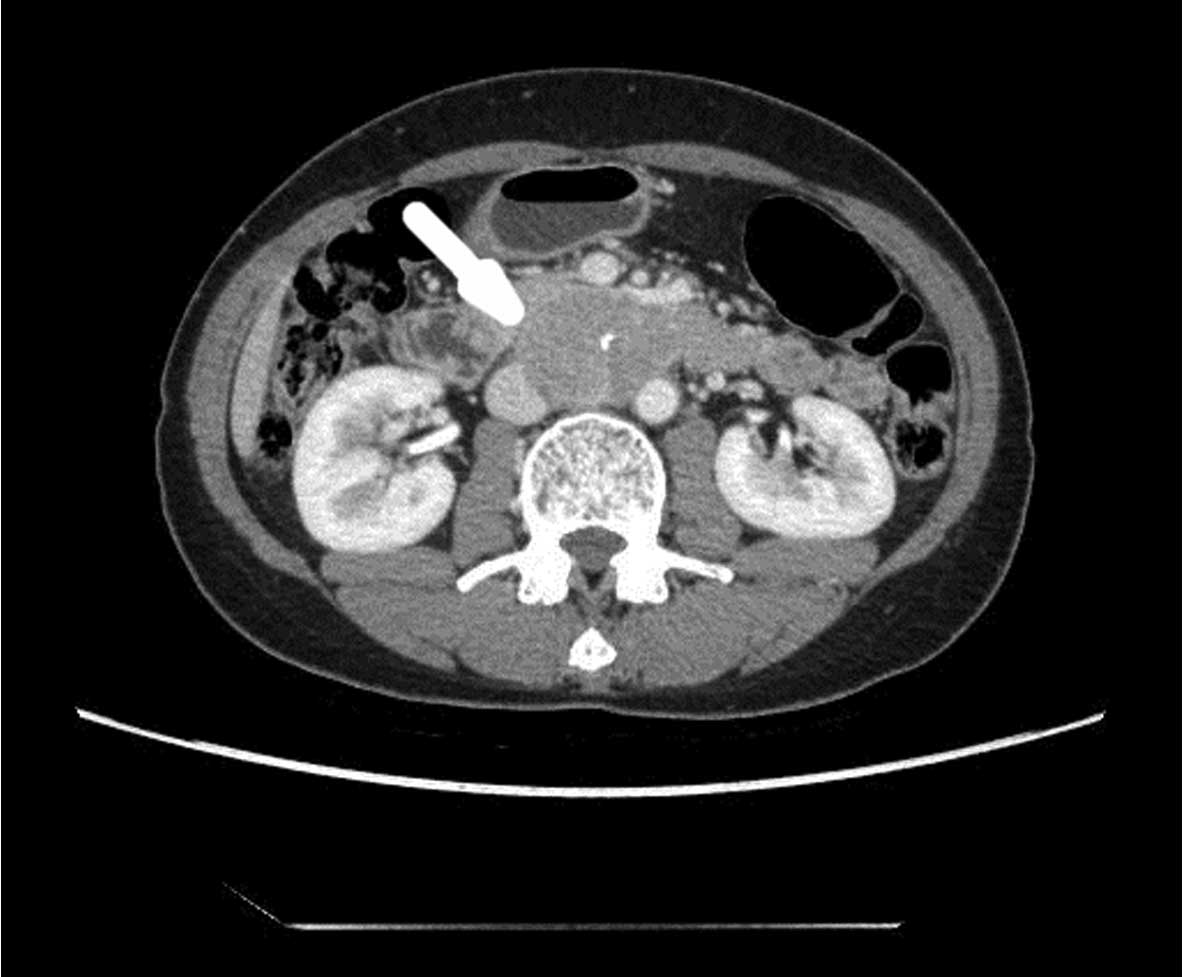
Preoperative positron emission tomography-computed tomography
(PET-CT), and CT angiography (CTA) revealed a round-shaped mass
that was ~6 cm in diameter and located anterior to the abdominal
aorta, proximal to the inferior vena cava at the level of the third
lumbar vertebra (termed L3). The tumor was in close proximity to,
and located between, the abdominal aorta and the inferior vena
cava; furthermore, the mass was posterior to the duodenum and the
uncinate process of the pancreas, as well as being tightly adhered
to the inferior vena cava. The tumor had a rich blood supply and no
obviously swollen retroperitoneal lymph nodes or distant metastases
were observed (Fig. 1).
Prior to surgery, the patient was suspected to have
an ectopic PHEO and was treated using orally administered Cardura
(doxazosin; Pfizer, Inc., New York, NY, USA; 4 mg, once a day for
seven days) to lower and control the elevated blood pressure to
120/80 mmHg. The preoperative assessment of the patient’s heart and
lung function indicated that she was able to tolerate the surgical
procedure. The patient had no previous history of upper abdominal
surgery, however, had previously undergone a cesarean section.
Preoperative preparation and
anesthesia
The preoperative preparations were similar to those
of laparotomic resections of ectopic adrenal PHEOs (7). The patient was placed in the left
lateral decubitus position (with the right side elevated ~70°)
under general anesthesia.
Installation of the da Vinci Robotic
Surgical System (Intuitive Surgical, Inc., Sunnyvale, CA, USA)
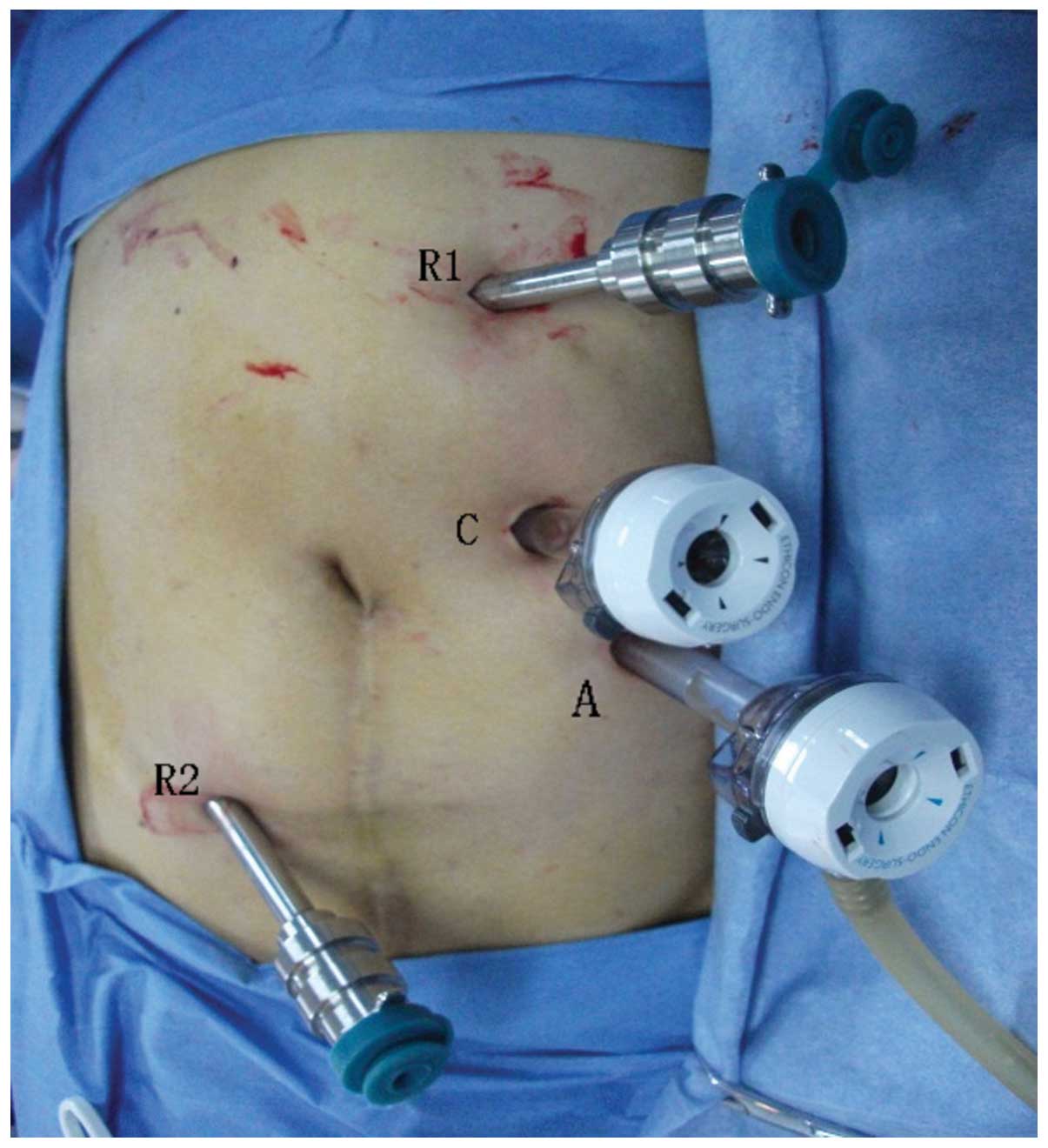
Based on the preoperative positioning and CT images,
the pneumoperitoneum was established by puncturing the point of
intersection of the left mid-clavicular line and the costal margin.
A trocar was inserted to establish the camera port, and a robotic
camera was inserted to determine whether tumor metastases were
present in the abdominal cavity and whether there were obvious
indications against performing the surgery. A four-port approach
was used to insert the remaining trocars (Fig. 2). The robotic arm tower was mounted
and the operating arms were installed. Subsequently, the accessory
port was positioned between robotic arm no. 1 and the camera
port.
Tumor resection
The lower abdominal adhesions were dissected, a
Kocher incision was made to mobilize the duodenum, and the
pancreatic head and the duodenum were shifted to the left. This was
to facilitate the investigation of the association between the
tumor and major blood vessels, such as the abdominal aorta and the
inferior vena cava.
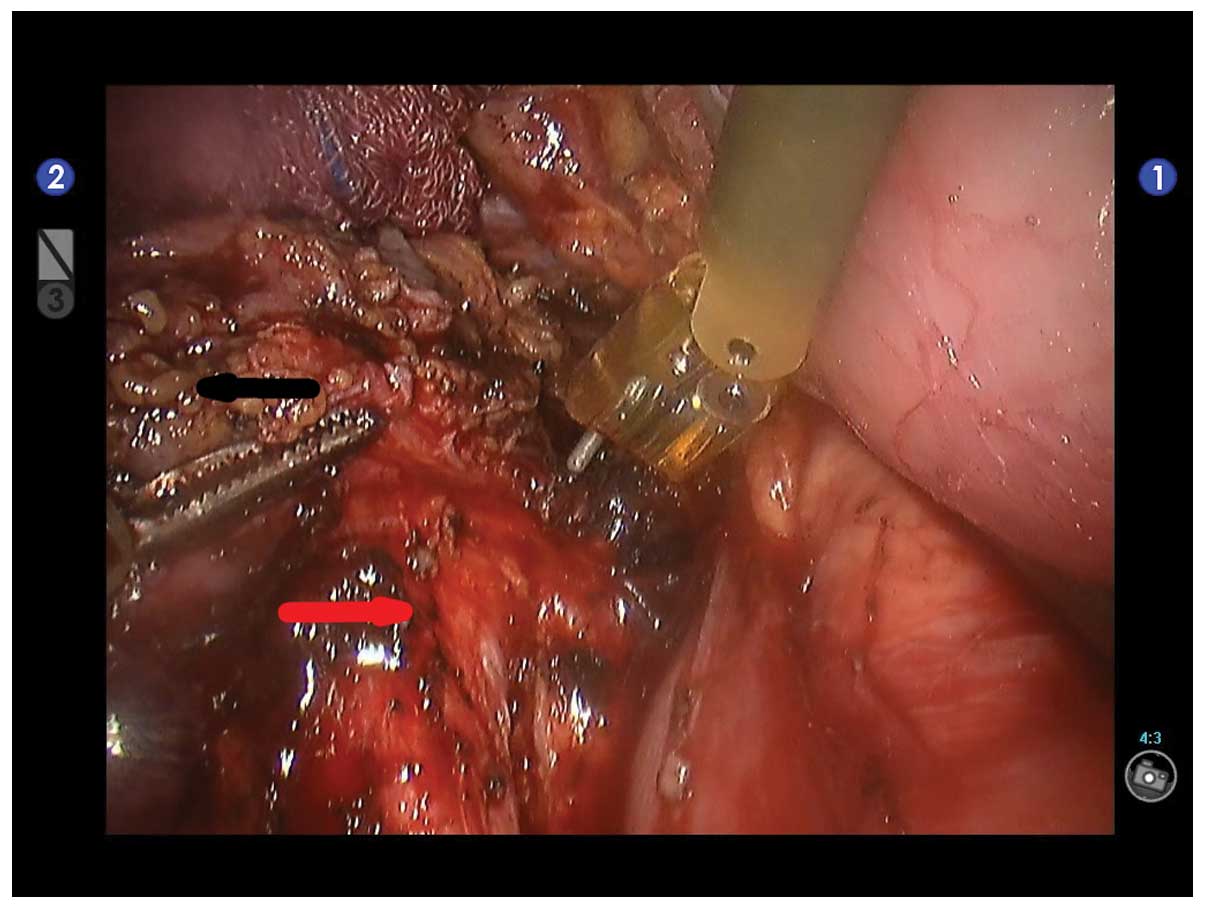
The tissue that was posterior to the tumor was
progressively freed from right to left and from bottom to top until
the level of the vena cava was reached. The abdominal aorta was
protected, using an electrical hook and bipolar coagulator to
seperate the tumor from the abdominal aorta and inferior vena cava,
while the tumor was dissected away from it (Fig. 3). The blood vessels that nourished
the tumor were ligated using an electric hook or titanium clips,
and the tumor was freed from the vena cava and the renal vein. The
tumor was observed to have densely infiltrated the inferior vena
cava; however, the intact tumor was completely dissected from the
inferior vena cava while the major blood vessels around the tumor
(such as the right gonadal vein) were carefully protected. Finally,
the adhesions between the tumor and the prevertebral tissue were
dissociated.
The tumor was placed in a specimen bag and a
separate incision was made to remove the specimen bag. The specimen
subsequently underwent pathological examination. In addition, the
wound surfaces were washed, examined and subjected to strict
hemostasis.
Drainage tube placement
A drainage tube was placed in the surgical area
between the abdominal aorta and the vena cava, and exited via the
trocar hole.
Results
There were no complications during surgery, the
intraoperative blood pressure was stable (without significant
fluctuation) and there was no requirement to convert to a
laparotomy. The patient’s drainage tube was removed after seven
days, and the patient was discharged 11 days following the surgery.
The postoperative pathological report obtained via analysis of a
tissue slice indicated a diagnosis of paraganglioma with visible
extracapsular vascular invasion (Fig
4).
The patient was followed up for three months and no
clear tumor recurrence was identified by CTA during the follow-up
examinations. The blood NE and E levels were restored to within
their normal ranges of 19.0–121 and 14.0–90.0 pg/ml,
respectively.
Discussion
The clinical manifestations of extra-adrenal PHEOs
are diverse, including paroxysmal symptoms (palpitations, headache,
sweating and pallor), hypertension, an adrenal or abdominal mass,
high blood sugar, lactic acidosis, weight loss and other symptoms
of the metabolic syndrome (8).
Extra-adrenal PHEOs commonly exhibit three typical symptoms, which
are headaches, palpitations and sweating. In addition, 80–100% of
patients have persistent or paroxysmal hypertension (9). The clinical manifestations depend on
the relative quantities of E, NE and dopamine that are secreted by
the tumor. The disease symptoms may exhibit a sudden onset that
generally persists for several minutes to 1 h and is precipitated
by hyperplasia, constipation, abdominal pressure, or a variety of
therapeutic agents (such as glucagon, contrast agents, tyramine,
metoclopramide and tricyclic antidepressants) (10). Therefore, intraoperative blood
pressure monitoring and the reduction of tumor stimulation present
as challenges for anesthesiologists and surgeons.
The emergence of laparoscopic techniques enables the
removal of adrenal tumors in a minimally invasive manner and the
laparoscopic resection of adrenal PHEOs has been used in clinical
practice for many years (11). An
investigation conducted outside of China by Gill (12) demonstrated that laparoscopic surgery
leads to milder stimulation of functional PHEOs when compared with
a laparotomy; furthermore, the CA hormone levels that are secreted
during surgery are lower. However, the difficulties and limitations
of laparoscopic resections of adrenal PHEOs arise when blood
vessels require handling during the surgical procedure, when the
tumor is located within anatomical structures that are located deep
in the abdominal cavity (particularly for retroperitoneal ectopic
PHEOs) and when the tumor is excessively large (11).
The da Vinci robot-assisted laparoscopic surgical
system is based on laparoscopic surgery and possesses various
advantages, such as clear three-dimensional images, the
EndoWristTM (Intuitive Surgical, Inc.) instrument (which
mimics the human wrist with seven degrees of freedom), hand-tremor
elimination, motion scaling and motion indexing (13). This system generates clear
three-dimensional images, and achieves an accurate
three-dimensional depth of field using a high resolution, thus
enabling the surgeon to acquire a visual field and an operating
position, which approximates open surgery. In particular, due to
the narrow retroperitoneal anatomical space that restricts the area
for conducting laparotomic surgery, the robot-assisted laparoscopic
surgical system provides natural advantages with regard to handling
the complex anatomical structures and the areas adjacent to any
important blood vessels (14).
Furthermore, this system overcomes certain issues associated with
the original laparoscopic techniques, for example, hand tremors and
a low degree of freedom when operating the instruments. Therefore,
the system achieves more precise separation and dissection of
tumors that are located within anatomical structures deep in the
abdominal cavity. Additionally, this method facilitates the
minimally invasive resection of tumors that are adjacent to major
blood vessels in the abdominal cavity (such as the abdominal aorta,
inferior vena cava, renal artery and the renal vein) and is
considered to be safer and more stable than traditional
laparoscopic surgical procedures. This novel technique fully
inherits the advantages of laparoscopic surgery, reduces the
stimulation of endocrine tumors, ligates and dissects the
tumor-feeding blood vessels in a timely manner and reduces the
incidence of intraoperative complications.
Currently there are a number of reports concerning
robot-assisted laparoscopic resection for adrenal tumors, such as
PHEO (15,16). As the occurrence of extra-adrenal
paraganglioma is rare, reports regarding this type of tumor are
also uncommon, to the best of our knowledge, only Lehrfeld et
al (14) have presented their
experience of conducting a robot-assisted excision of a
retroperitoneal mass in 2010.
In the present case, due to the specific anatomical
location of the tumor, which was proximal to the inferior vena cava
and abdominal aorta, the traditional laparoscopic instruments were
limited by the deep anatomical structures and the omental
mesenteric vascular occlusion. Generally, surgeons are unable to
avoid avulsing aspects of the mesenteric vessels, which may affect
the blood supply to regions of the intestines, cause ischemia,
delay postoperative functional recovery and potentially lead to
partial bowel resection. Whereas, robot-assisted laparoscopic
surgery systems are able to accurately dissect the tumor from the
surrounding tissue while the feeding vessels surrounding the tumor
(particularly those with an abundant blood supply) may be stanched
using an ultrasonic scalpel and electrocoagulation; however, during
traditional laparoscopic surgery, there is practically no ligation
or suturing. When flexible robotic arms are adopted for surgery,
the vessels surrounding the tumor may be smoothly manipulated to
achieve satisfactory hemostasis and a successful dissection.
As a result of our past experience (17–19),
the robot-assisted laparoscopic surgery system is considered to be
efficacious when adopted for the excision of benign and borderline
retroperitoneal tumors that have no significant adhesions with
surrounding tissues, such as fibrous tumors, teratoma and
particularly for tumors that are in close proximity to major
vessels. The biological behavior and pathological nature of
malignant tumors varies, however, if the capsule is complete, and
the radiological data and intraoperative findings demonstrate no
significant infiltration, minimally invasive surgery can also be
considered. The robot-assisted system may facilitate the reduction
of surgical trauma and the influence on the body’s immune system,
thus promoting postoperative recovery, enhancing the quality of
life of the patients and improving all possible outcomes.
In conclusion, retroperitoneal ectopic adrenal PHEOs
are particularly rare. This type of tumor is located deep within
the abdominal cavity, often in the deep retroperitoneal anatomical
structures. Consequently, PHEOs are complex to treat, even when
adopting the laparotomic surgical approach. The associated risk is
particularly significant for tumors that affect the endocrine
functions. The robot-assisted laparoscopic surgical system provides
a novel, minimally invasive solution for treating retroperitoneal
tumors. Furthermore, this technique reduces stimulation of the
tumor and prevents or minimizes complications. To the best of our
knowledge, the patient in the present study is currently the first
known patient in China that has successfully undergone a
robot-assisted resection of a retroperitoneal ectopic adrenal PHEO,
making this study particularly significant.
Acknowledgements
The present study was supported by a Shanghai
Science and Technology Commission project grant for 2010 (grant no.
10411955600).
References
|
1
|
Park JS, Lee KY, Kim JK and Yoon DS: The
first laparoscopic resection of extra-adrenal pheochromocytoma
using the da Vinci robotic system. J Laparoendosc Adv Surg Tech A.
19:63–65. 2009.
|
|
2
|
Whalen RK, Althausen AF and Daniels GH:
Extra-adrenal pheochromocytoma. J Urol. 147:1–10. 1992.
|
|
3
|
Barski D: Management and follow up of
extra-adrenal phaeochromocytoma. Cent European J Urol. 67:156–161.
2014.
|
|
4
|
Matro J, Giubellino A and Pacak K: Current
and future therapeutic approaches for metastatic pheochromocytoma
and paraganglioma: focus on SDHB tumors. Horm Metab Res.
45:147–153. 2013.
|
|
5
|
Lanfranco AR, Castellanos AE, Desai JP and
Meyers WC: Robotic surgery: a current perspective. Ann Surg.
239:14–21. 2004.
|
|
6
|
Dakin GF and Gagner M: Comparison of
laparoscopic skills performance between standard instruments and
two surgical robotic systems. Surg Endosc. 17:574–579. 2003.
|
|
7
|
Ng JM, Binsaleh S, Tisdale B, et al:
Laparoscopic excision of para-aortic ectopic pheochromocytoma. Can
J Urol. 13:3271–3274. 2006.
|
|
8
|
Martins R and Bugalho MJ:
Paragangliomas/Pheochromocytomas: clinically oriented genetic
testing. Int J Endocrinol. 2014:7941872014.
|
|
9
|
Joynt KE, Moslehi JJ and Baughman KL:
Paragangliomas: etiology, presentation, and management. Cardiol
Rev. 17:159–164. 2009.
|
|
10
|
Kebebew E and Duh QY: Benign and malignant
pheochromocytoma: diagnosis, treatment, and follow-up. Surg Oncol
Clin N Am. 7:765–789. 1998.
|
|
11
|
Faria EF, Andreoni C, Krebs RK, et al:
Advances in pheochromocytoma management in the era of laparoscopy.
J Endourol. 21:1303–1307. 2007.
|
|
12
|
Gill IS: The case for laparoscopic
adrenalectomy. J Urol. 166:429–436. 2001.
|
|
13
|
Sung GT and Gill IS: Robotic laparoscopic
surgery: a comparison of the DA Vinci and Zeus systems. Urology.
58:893–898. 2001.
|
|
14
|
Lehrfeld T, Natale R, Sharma S, et al:
Robot-assisted excision of a retroperitoneal mass between the left
renal artery and vein. JSLS. 14:447–449. 2010.
|
|
15
|
Dickson PV, Alex GC, Grubbs EG, et al:
Robotic-assisted retroperitoneoscopic adrenalectomy: making a good
procedure even better. Am Surg. 79:84–89. 2013.
|
|
16
|
Galvani C, Gorodner MV and Joseph Espat N:
Robotic-assisted resection of adrenal aldosteronoma. Ann Surg
Oncol. 18:479–481. 2011.
|
|
17
|
Zhan Q, Deng XX, Han B, et al:
Robotic-assisted pancreatic resection: a report of 47 cases. Int J
Med Robot. 9:44–51. 2013.
|
|
18
|
Peng CH, Shen BY, Deng XX, et al: Early
experience for the robotic duodenum-preserving pancreatic head
resection. World J Surg. 36:1136–1141. 2012.
|
|
19
|
Shen BY, Zhan Q, Deng XX, et al: Radical
resection of gallbladder cancer: could it be robotic? Surg Endosc.
26:3245–3250. 2012.
|