Introduction
Periosteal chondroma is a rare benign cartilaginous
tumor that occurs under or in the periosteum on the surface of
cortical bone. It was first described by Lichtenstein and Hall
(1) in a report of six cases.
Periosteal chondromas account for <2% of all chondromas and may
occur in adults or children (2),
however, the disease is predominantly identified in patients <30
years of age, with the highest frequency between the ages of 10 and
20 years (3). It is typically
observed in the metaphyses of long bones beneath the periosteal
membrane, particularly the proximal humerus and tubular bones of
the hands (2,4). A number of studies have also reported
erosion of the spine, clavicle and costal cartilage (2,7,8). The
diagnosis of periosteal chondromas is primarily based on
histological characteristics. Although the genetic mechanisms of
the disease remain unclear, genetic rearrangement in chromosome 12
has been reported to be associated with this disease (5). Treatment for periosteal chondroma
includes intralesional, marginal and en bloc resection and the
recurrence rate is 3.6% (2).
The current study reports a case of periosteal
chondroma located in the distal femur, and reviews the literature
with regard to clinical, radiological, histopathological and
treatment criteria, in addition to discussing the differential
diagnosis of this condition. Written informed consent was obtained
from the patient’s family.
Case report
A 14-year-old female presented to the Orthopedic
Department of the General Hospital of Jinan Military Commanding
Region (Jinan, China) with a two-month history of a
gradually increasing mass in the right lower thigh. No history of
trauma or episodes of pain similar to that observed in other bone
tumors, such as continuous pain or pain at night, were noted. Firm,
non-tender swelling in the distal thigh was observed upon physical
examination, with normal overlying skin and no neural deficit.
Radiographs revealed an overhanging edge and a radiolucent shadow
with stippled calcification (Fig.
1). Computed tomography (CT) imaging showed a solid tumor of
5×4 cm in diameter, with specks of calcification, which was
associated with the right distal femur bone (Fig. 2). Magnetic resonance imaging (MRI)
revealed a lobular heterogeneous mass arising from the femur, which
was hypointense on T1-weighted images and hyperintense on
T2-weighted images (Fig. 3). No
aggressive radiological appearance was observed, and chromosomal
analysis was unremarkable. Cytological examination of the excision
biopsy revealed cellular pleomorphism and binucleate cells.
Although cytological findings indicated a benign
tumor, a diagnosis of chondrosarcoma could not be excluded.
Therefore, an extended resection was performed; the tumor was
excised en bloc, including margins of normal bone, and ipsilateral
limb fibula transplantation was used to repair the cortical defect.
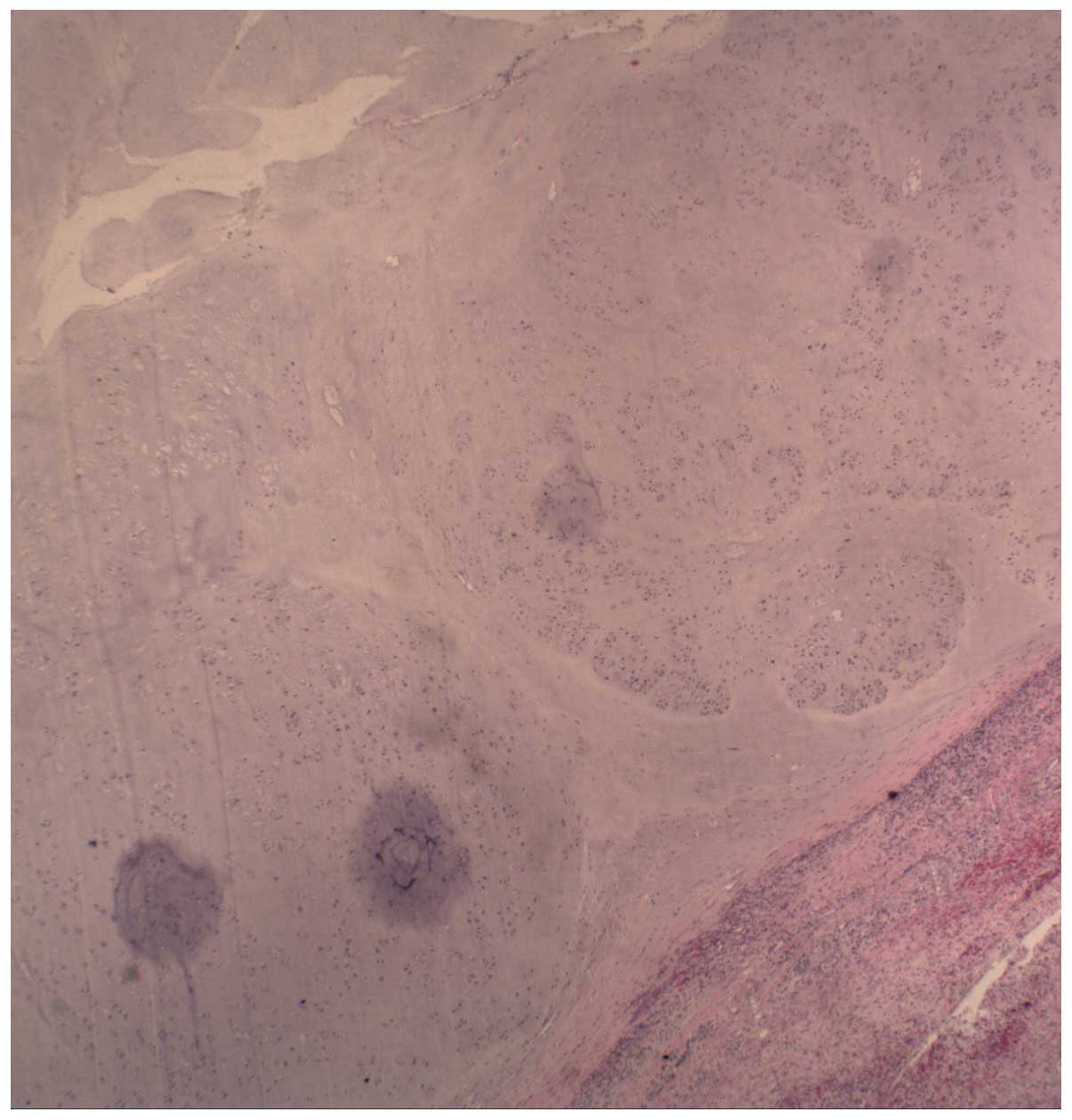
Microscopic examination revealed lobules of hyaline cartilage
composed of chondrocytes, with foci of endochondral ossification
and calcification (Fig. 4). The
lesion showed hypercellularity, however, cytological atypia was not
observed. Additionally, no penetration to the medullary cavity and
surrounding soft tissues was identified. A diagnosis of periosteal
chondroma was therefore determined.
The patient’s surgery was successful and six weeks
later, the patient walked with the aid of a brace. At follow-up,
radiographs revealed that healing had occurred following the bone
graft and no new tumor tissue was observed. No further treatment
was required.
Discussion
Periosteal chondroma is an uncommon benign tumor of
the hyaline cartilage (6). It is
slow-growing and frequently erodes the cortex. The lesion is
generally observed between the ages of 10 and 30 years with equal
gender distribution (2–4). The patient in the present study was
14-year-old female with a lesion in the right distal femur;
previous cases of periosteal chondroma occurring in the femur are
summarized in Table I (2,3,9,10).
 | Table IClinical characteristics of 10
patients with periosteal chondroma in the femur. |
Table I
Clinical characteristics of 10
patients with periosteal chondroma in the femur.
| Author
(reference) | Gender/age,
years | Site | Symptoms | Duration of symptoms,
months | Radiographic
pattern | Treatment | Follow-up, years |
|---|
| Boriani et al
(3) | M/11 | PF | Pain, mass | 24 | Overhanging
edges | Marginal
excision | 22 |
| M/26 | DF | Pain | 10 | Calcification of
matrix | Marginal
excision | 4 |
| M/6 | DF | Pain | 12 | Scalloping | Marginal
excision | 3 |
| M/18 | MF | Pain, mass | 10 | Calcification of
matrix | Incisional biopsy,
radiotherapy, hip disarticulation | 22 |
| Lewis et
al(2) | F/9 | PF | Pain | 5 | Sclerosis | Curettage | 3 |
| M/19 | DF | Pain, mass | 4 | No calcification of
matrix | Curettage | 3 |
| NP | DF | Pain | 5 | NP | Marginal
excision | 3 |
| Tillich et al
(9) | F/8 | PF | Pain | 1 | Sclerosis | Curettage | NP |
| Wheelhouse and
Griffin 10) | F/21 | DF | Mass | 108 | Sclerosis | En bloc
resection | 4.5 |
| Zheng (current) | F/14 | DF | Swelling | 2 | Overhanging
edges | En bloc
resection | 0.5 |
Of the 10 reviewed cases of periosteal chondroma of
the femur, five were males, four were females and one had no
reported gender data. The mean age at the beginning of treatment
was 14.67 years (range, 6–26 years), excluding one case in which no
accurate age was reported. With regard to the location of the
tumor, six cases involved the distal femur, three involved the
proximal femur, and one involved the middle femur.
Evaluation of the clinical course of periosteal
chondroma may aid in its diagnosis. Typically, the first symptom is
localised swelling, followed by moderate and prolonged pain (~6
months) (3). Of the reviewed cases,
five patients exhibited this pattern of symptoms for a long
duration (≥10 months) (mean, 18.1 months; range, 1–108 months). The
presence of pain is a significant clinical feature in the
evaluation of cartilaginous tumors; in adults with a histologically
low-grade cartilaginous tumor, we hypothesize that pain may
indicate aggressive biological behavior. However, in the reviewed
cases, the presence of pain was not associated with treatment
procedure or clinical effect.
Radiographic features of periosteal chondroma may
vary between cases. The mass typically arises from the surface of
bone, exhibiting scalloping of the cortex and a well-defined margin
between the tumor and bone (3).
Tumor sclerosis in this type of tumor is common and may include
overhanging edges and soft-tissue masses with a variable pattern of
calcification and ossification. Of the nine cases for which
radiographic pattern data was provided, one showed clear scalloping
of the cortex, two exhibited overhanging edges, three showed
sclerosis, two showed calcification or ossification of the
cartilaginous matrix and one patient exhibited no calcification or
ossification of the cartilaginous matrix. In the current case, CT
imaging revealed a soft tissue mass of iso and high density,
containing stippled calcifications and was associated with the
destruction of local regions of bone. MRI showed a sharply
delineated subperiosteal lobulated mass at the bone surface,
consisting of a matrix with a bright signal, a hypointense lining
on T2-weighted images and isointense signal relative to muscle on
T1-weighted images. The absence of CT and MRI data in the reviewed
cases prevents further speculation with regard to the use of these
imaging modalities for the diagnosis of this condition.
Histopathologically, periosteal chondromas exhibit a
prominent lobular arrangement of hyaline cartilage extending from
the periosteum into the adjacent cortical bone (4). They are typically hypocellular,
however, increased cellularity with nuclear pleomorphism,
binucleation, and multinucleation may be observed (2–4). The
presence of hypercellularity and nuclear atypia, which often
indicates malignancy, may lead to difficulties in the differential
diagnosis of such cases.
The differential diagnosis of periosteal chondroma
in this location includes chondrosarcoma, osteochondroma and
periosteal osteosarcoma. Compared with periosteal chondromas,
chondrosarcomas are generally greater in size and occur in older
patients (>50 years of age); extension into the soft tissue may
also be observed (3).
Osteochondromas are more commonly detected in the femurs of
adolescents, in contrast with periosteal chondromas, which
typically occur in young adults (11). Osteochondromas may also be
distinguished by the presence of a dense osteoid formation in the
cortex and medulla of the mass, and by the continuation with its
originating bone (12). Periosteal
chondrosarcoma shows popcorn calcifications on radiographs, which
present as a collection of scalloped radiolucencies, each with a
sclerotic margin, whereas periosteal osteosarcoma commonly exhibits
perpendicular spicules of calcification (13). Periosteal osteosarcomas are
slow-growing, and primarily arise beneath the periosteum in the
distal femur, inducing new bone formation. This is observed as a
radiolucent lesion on the bone surface with perpendicular striae
and a peripheral Codman’s triangle (14). Lace-like, malignant osteoids may be
detected, however, chondroid areas with high-grade anaplastic cells
dominate the histological appearance (14). Differentiating between these
conditions may necessitate an excision biopsy; however, it may also
be difficult to distinguish low-grade chondrosarcoma from chondroma
on the basis of histology (13).
A previous literature review revealed that, among
165 cases of periosteal chondroma, six reported local recurrence (a
recurrence rate of 3.6%) (2). Of
the cases of periosteal chondroma in the femur, no recurrence was
noted during postoperative follow-ups (range, 6 months to 22 years;
mean, 7.22 years). The treatments for periosteal chondroma of the
femur included marginal excision, en bloc resection and curettage.
In the cases reviewed in the current study, two patients were
treated by en bloc resection, four by marginal excision, three by
curettage and one by hip disarticulation following incisional
biopsy and radiotherapy. Marginal excision and curettage are
preferable options if the diagnosis is certain prior to surgery;
otherwise, en bloc resection may be a more beneficial treatment
strategy. Therefore, the results of this study may increase current
understanding with regard to the diagnosis of periosteal chondroma
in the femur and the selection of suitable treatments.
References
|
1
|
Lichtenstein L and Hall JE: Periosteal
chondroma; a distinctive benign cartilage tumor. J Bone Joint Surg
Am. 24-A-3:691–697. 1952.
|
|
2
|
Lewis MM, Kenan S, Yabut SM, Norman A and
Steiner G: Periosteal chondroma. A report of ten cases and review
of the literature. Clin Orthop Relat Res. 256:185–192.
1990.PubMed/NCBI
|
|
3
|
Boriani S, Bacchini P, Bertoni F and
Campanacci M: Periosteal chondroma. A review of twenty cases. J
Bone Joint Surg Am. 65:205–212. 1983.PubMed/NCBI
|
|
4
|
Bauer TW, Dorfman HD and Latham JT Jr:
Periosteal chondroma. A clinicopathologic study of 23 cases. Am J
Surg Pathol. 6:631–637. 1982. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Mandahl N, Willén H, Rydholm A, Heim S and
Mitelman F: Rearrangement of band q13 on both chromosomes 12 in a
periosteal chondroma. Genes Chromosomes Cancer. 6:121–123. 1993.
View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Brien EW, Mirra JM and Luck JV Jr: Benign
and malignant cartilage tumors of bone and joint: their anatomic
and theoretical basis with an emphasis on radiology, pathology and
clinical biology. II Juxtacortical cartilage tumors. Skeletal
Radiol. 28:1–20. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Peidro L, Suso S, Alcantara E and Ramon R:
Periosteal chondroma of the clavicle. Skeletal Radiol. 25:406–408.
1996. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Fahim DK, Johnson KK, Whitehead WE, Curry
DJ, Luerssen TG and Jea A: Periosteal chondroma of the pediatric
cervical spine. J Neurosurg Pediatr. 3:151–156. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Tillich M, Lindbichler F, Reittner P,
Weybora W, Linhart W and Fotter R: Childhood periosteal chondroma:
femoral neck thickening and remote hyperostosis as clues to plain
film diagnosis. Pediatr Radiol. 28:8991998. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Wheelhouse WW and Griffin PP: Periosteal
chondroma. South Med J. 75:1003–1006. 1982. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Singh AP, Singh AP and Mahajan S:
Periosteal chondroma of the sacrum. Can J Surg. 51:105–106.
2008.
|
|
12
|
Agrawal A, Dwivedi SP, Joshi R and Gangane
N: Osteochondroma of the sacrum with a correlative radiographic and
histological evaluation. Pediatr Neurosurg. 41:46–48. 2005.
View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Akansu B, Atık E, Altintaş S, Kalaci A and
Canda S: Periosteal chondroma of the ischium; an unusual location.
Turk Patoloji Derg. 28:172–174. 2012.PubMed/NCBI
|
|
14
|
Sulzbacher I, Puig S, Trieb K and Lang S:
Periosteal osteoblastoma: a case report and a review of the
literature. Pathol Int. 50:667–671. 2000. View Article : Google Scholar : PubMed/NCBI
|