Introduction
The worldwide incidence of renal cell carcinoma
(RCC), a predominantly male (2:1 ratio) disease, is ~271,000 new
cases and 116,000 fatalities per year (1). There are several known risk factors for
RCC, such as obesity, hypertension and decreased fruit and
vegetable consumption. A subset of patients with this cancer has
local or systemic symptoms, including flank pain, hematuria, a
palpable abdominal mass, fever and wasting syndromes (2). However, in recent years, approximately
half of the RCC patients have had no clinical symptoms; the disease
was identified by abdominal imaging during a health check-up. The
traditional method for clinical diagnosis is abdominal imaging.
Computed tomography can be used to stage the primary tumor and
determine the lymphadenopathy and metastasis (3), and Doppler sonography can better detect
the tumor extension in equivocal cases (4). However, despite its sensitivity, imaging
is relatively non-specific; therefore, the disease must be
confirmed using renal biopsy. Although urine cytology, a
reproducible and noninvasive approach, may be valuable for
differentiating urothelial cell carcinoma from RCC (5), it lacks sensitivity. Currently, there is
no adequate sensitive, reproducible, specific and noninvasive
biomarker that can reliably be used to detect RCC.
In recent years, an increasing number of researchers
have focused on volatile organic compound (VOC) profiling, a novel
and robust procedure, because it is convenient and inexpensive.
Altomare et al (6) confirmed
that the pattern of breath VOCs in patients with colorectal cancer
was different from healthy controls. Ikeda et al (7) proposed serum VOC profiling as a novel
diagnostic approach for gastrointestinal cancer. Wu et al
(8) demonstrated that hepatocellular
carcinoma patients had a unique urinary VOC profile. Filipiak et
al (9) demonstrated that lung
cancer-derived cells exhibited specific volatile compounds. These
studies indicate that different cancers may produce different VOCs
profiles. Numerous metabolic profiling studies have focused on the
urinary levels of nucleosides as biomarkers of cancers, including
leukemia (10), breast cancer
(11), colorectal cancer (12) and hepatocellular carcinoma (13), which are detected independent of
patient age or gender. Metabolomics can also be used to elucidate
biomarkers. Ganti and Weiss (14)
obtained the urinary non-volatile metabolic profiles of RCC.
Notably, Jobu et al (15)
proposed that urinary VOC metabolites in human bladder cancer were
significantly more sensitive compared to urine cytology. However,
whether VOC profiling can be used to identify RCC remains to be
elucidated.
In the current study, gas chromatography/mass
spectrometry (GC/MS) and multivariate data analysis were used to
compare the VOCs in urine samples from RCC patients (preoperative
and postoperative) and healthy subjects to identify potential
volatile biomarkers of RCC in VOCs.
Materials and methods
Patients
All the experimental protocols were approved by the
Ethics Committee of the First Affiliated Hospital of Harbin Medical
University (Harbin, Heilongjiang, China; no. 201314), and the
informed consent was obtained from the parents of the patients
prior to study enrollment. A total of 22 patients who were admitted
to the Department of Urology (The First Affiliated Hospital of
Harbin Medical University) between May 2011 and October 2012 were
selected for the study (the cancer group). These 22 patients were
diagnosed with RCC. In addition to the cancer group, 25 healthy
volunteers were also included in the study.
Of the 22 patients with RCC, 15 were males and 7
were females. The mean age of the patients was 57.65±10.92 years.
Among them, 18 patients (12 males and 6 females) were involved in
the preoperative and postoperative collection. The mean age was
58.22±11.29 years. The normal control group of 25 included 12 males
and 8 females. The mean age of individuals in the normal control
group was 57.92±10.81 years.
Urine sample collection
Urine samples (2 ml) were immediately transferred to
evacuated 20 ml heparinized glass vials (Supelco, Inc., Bellefonte,
CA, USA) before surgery and 1 day after surgery. All the samples
were analyzed within 2 h of collection.
Solid-phase microextraction
(SPME)
For SPME, 75-µm carboxen/polydimethylsiloxane fibers
(Supelco, Inc.) were used. The SPME fiber was inserted into the
vial and exposed to the gaseous sample for 40 min at 40°C.
Subsequently, the volatile compounds were de-absorbed in a hot GC
injector at 200°C for 2 min.
GC/MS analysis
Analysis was performed using a GC/MS (Shimadzu GC-MS
QP 2010; Shimadzu, Kyoto, Japan) equipped with a DB-5MS (30 m ×
0.250 mm × 0.25 µm) (Agilent Technologies, Inc., Santa Clara, CA,
USA) plot column. Injections were conducted in the splitless mode.
The temperature of the injector was 200°C. The flow rate of the
helium (99.999%) carrier gas was maintained constantly at 2 ml
min−1. The column temperature was maintained at 40°C for
2 min to concentrate the hydrocarbons at the head of the column.
Subsequently, the column temperature was increased 7°C
min−1 to 200°C for 1 min and following this, was ramped
20°C min−1 to 230°C for 3 min. The MS analyses were
performed in full-scan mode using a scan range of 35–200 amu. The
ion source was maintained at 230°C, and an ionization energy of 70
eV was used for each measurement.
Extraction and pretreatment of the
GC/MS raw data
Raw GC/MS data were converted into CDF format
(NetCDF) files using Shimadzu GC/MS Postrun Analysis software and
processed using the XCMS toolbox (http://metlin.scripps.edu/xcms/).
Statistical analyses
Total area normalization was performed prior to the
statistical analysis. Normalized data were subsequently exported to
SIMCA-p 11.5 (Umetrics, Malmo, Sweden) for principal component
analysis (PCA) and a partial least-squares discriminant analysis
(PLSDA) was performed. To guard against overfitting, the default
seven-round cross-validation in the SIMCA-p software was applied,
and permutation tests with 100 iterations were also carried out to
further validate the supervised model. In addition, the two-sided
Welch two sample t-test was performed to determine the significance
of each metabolite. Based on the variable importance in the
projection (VIP values) from the PLSDA model and P-values from
t-tests with thresholds of 1.2 and 0.05, potential metabolic
biomarkers were selected. P<0.05 was considered to indicate a
statistically significant difference.
Results
VOCs in RCC
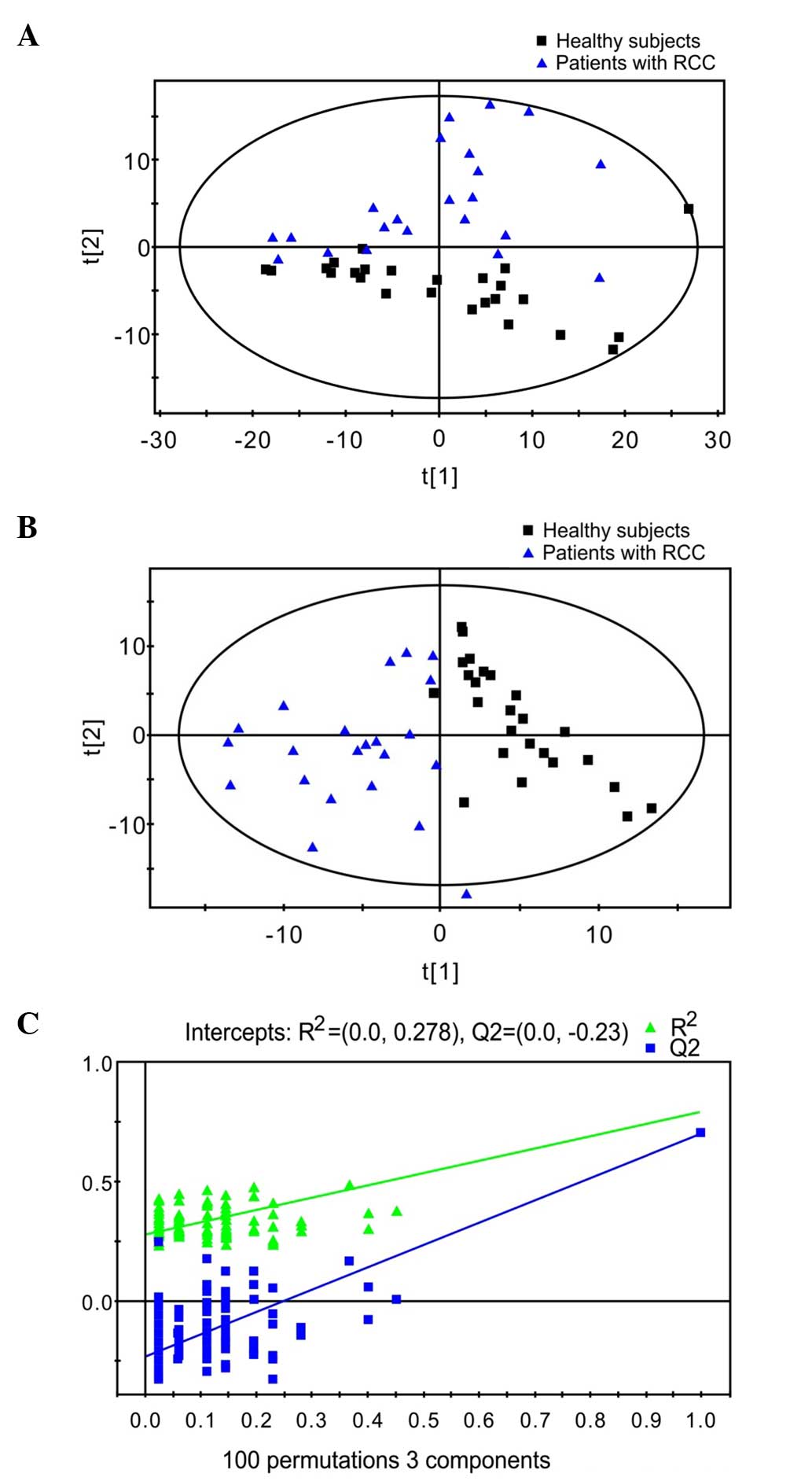
The VOCs in the urine samples of the 22 patients
with RCC and 25 healthy subjects were analyzed by GC/MS. Between
the patients with RCC and the healthy subjects, a two-dimensional
PCA score plot was obtained using 207 parameters, which showed a
good separation tendency (Fig. 1A). A
PLSDA score plot was subsequently used to separate these two groups
with three components (R2X=0.763, R2Y=0.791,
and Q2=0.702) (Fig. 1B). A
validation plot obtained from 100 permutation tests showed all of
the R2 and Q2 values calculated from the
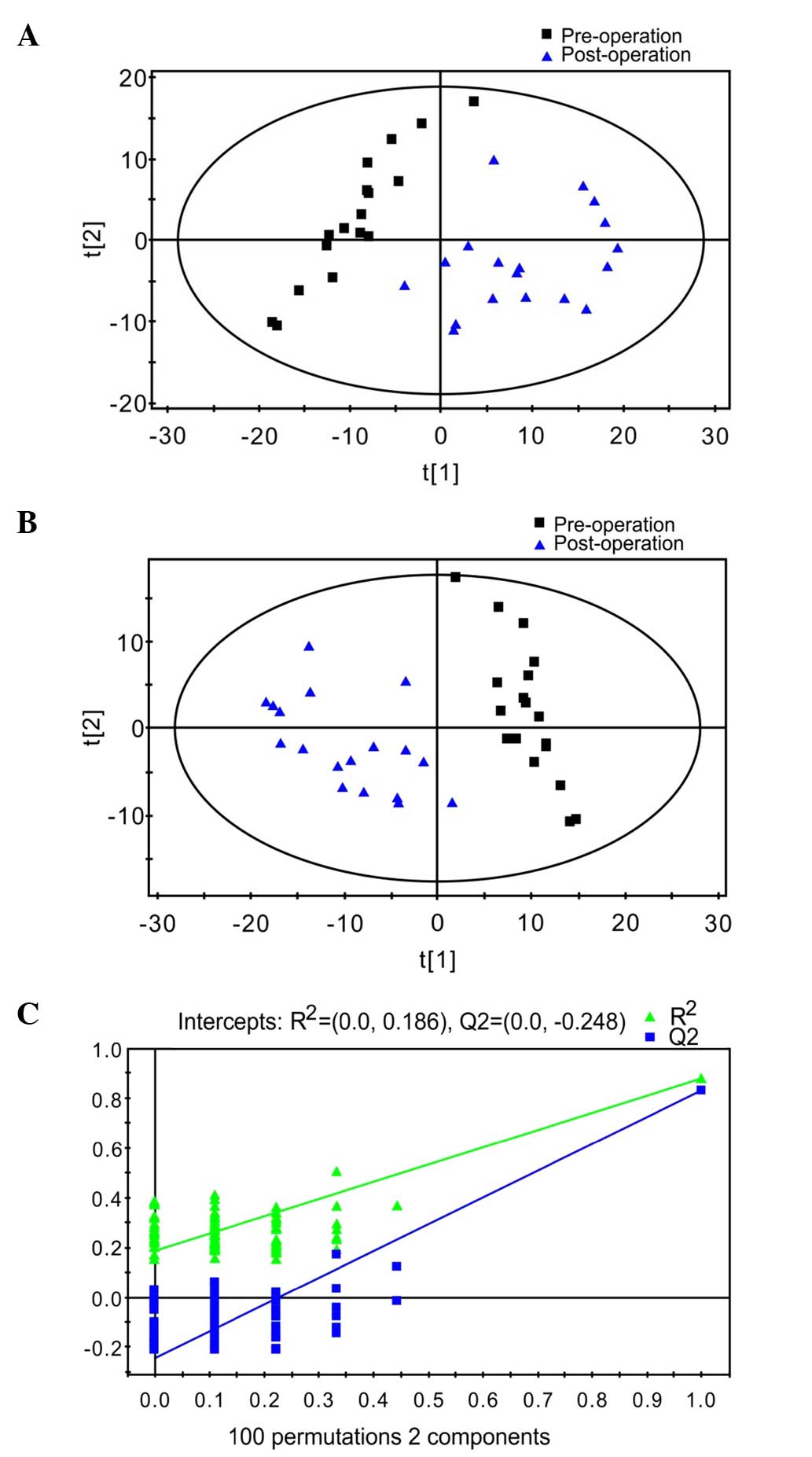
permutated data were lower than the original values (Fig. 1C). Between preoperative and
postoperative patients with RCC, we obtained 524 variables and
another PCA score plot (Fig. 2A),
PLSDA score plot (Fig. 2B) and a
validation plot (Fig. 2C) were created
by repeating the above steps. The results of these plots
demonstrated a good PCA separation tendency. The PLSDA separated
the patients with two components (R2X=0.614,
R2Y=0.879, and Q2=0.833). All of the VIP
values of the examined factors in the PLSDA model were calculated.
The distinct metabolic biomarkers were selected based on the
standard of a VIP value >1.2 using the NIST 11 database with a
similarity threshold of 75% (Tables I
and II).
 | Table I.Specific volatile organic compound
biomarkers identified at abnormal levels in the urine between
patients of RCC and healthy subjects. |
Table I.
Specific volatile organic compound
biomarkers identified at abnormal levels in the urine between
patients of RCC and healthy subjects.
| Potential
biomarker | RT, min | VIP | P-value | FC |
|---|
| Styrene |
6.069096 | 1.9154 |
1.87×10−07 | −12.09 |
| Phenol |
8.157637 | 1.9006 |
3.11×10−05 | 2.7 |
| Decanal | 13.2248 | 1.7131 |
2.14×10−05 | 3.04 |
|
1,6-Dioxacyclododecane-7,12-dione | 19.72507 | 1.6994 |
1.35×10−05 | 3.83 |
|
1-bromo-1-(3-methyl-1-pentenylidene)-2,2,3,3-tetramethyl-cyclopropane | 18.9668 | 1.45 |
5.36×10−05 | 0.57 |
|
Isolongifolene-5-ol | 18.39984 | 1.4163 |
1.21×10−03 | 1.17 |
| Nonanal | 11.02492 | 1.3884 |
2.67×10−03 | 2.99 |
|
2,5-Cyclohexadiene-1,4-dione,
2,6-bis(1,1-dimethylethyl)- | 18.3866 | 1.3356 |
1.79×10−03 | 1.36 |
| 4-Heptanone |
5.650597 | 1.3052 |
8.09×10−04 | −2.23 |
| Tetradecane | 18.3769 | 1.2991 |
3.65×10−03 | 1.09 |
|
3-Ethyl-3-methylheptane |
9.890793 | 1.2973 |
2.19×10−03 | 4.66 |
|
Dimethyl-silanediol |
3.061324 | 1.2879 |
1.59×10−03 | −6.31 |
| Aniline |
8.10944 | 1.2527 |
2.54×10−02 | 0.69 |
|
2,6,10,14-Tetramethyl-pentadecane | 22.31222 | 1.2163 |
3.79×10−03 | 1.45 |
 | Table II.Specific volatile organic compound
biomarkers identified at abnormal levels in the urine between
preoperative and postoperative patients of RCC. |
Table II.
Specific volatile organic compound
biomarkers identified at abnormal levels in the urine between
preoperative and postoperative patients of RCC.
| Potential
biomarker | RT, min | VIP | P-value | FC |
|---|
|
2-Ethyl-1-hexanol |
9.260928 | 1.4498 |
4.01×10−09 |
7.44 |
|
6-t-Butyl-2,2,9,9-tetramethyl-3,5-decadien-7-yne | 18.96002 | 1.2408 |
2.70×10−07 | −1.03 |
| Cyclohexanone |
6.147346 | 1.2383 |
5.12×10−06 |
9.75 |
Discussion
Currently, the relatively common VOC samples include
breath, blood and urine. Studies have confirmed specific and
distinct combinations of VOCs from patients with a variety of
cancers (including lung, breast and colorectal cancer) (16–19). Urinary
VOC metabolites are more useful biomarkers compared to the VOCs
identified in breath and blood for assessing VOC exposure, as
urinary metabolites have longer physiological half-lives and
sampling is non-invasive (6). The
micromolecular metabolites of RCC cells are freely filtered into
the urine (15). Urine sampling may
avoid the interference of uncertain primary or secondary
metabolites compared with breath or blood. The present study
acquired the expected VOC profiles from the urine of RCC
patients.
Compared to the healthy subjects, patients with RCC
showed increased levels of VOC biomarkers, including phenol;
decanal; 1,6-dioxacyclododecane-7,12-dione;
1-bromo-1-(3-methyl-1-pentenylidene)-2,2,3,3-tetramethyl-cyclopropane;
nonanal; 3-ethyl-3-methylheptane; isolongifolene-5-ol;
2,5-cyclohexadiene-1,4-dione, 2,6-bis(1,1-dimethylethyl);
tetradecane; aniline; and 2,6,10,14-tetramethyl-pentadecane. Three
components were decreased, which were styrene; 4-heptanone; and
dimethyl silanediol.
The results showed that 11 biomarkers were increased
in RCC patients. These biomarkers were mostly aldehydes, ketones,
alkenes, alkanes and substituted benzene compounds, which are
produced in response to oxidative stress (20), although the mechanisms by which these
compounds were produced remain to be elucidated.
2,6,10,14-Tetramethyl-pentadecane, a strong oxidant, was identified
among these compounds, suggesting that oxidative stress may be
involved. Decanal is a linear aldehyde that is formed from the
oxidation of the majority of the unsaturated fatty acids found in
human skin lipids (21). Pentadecane
is possibly derived from local oxidative stress in cancer cells, as
tumor cells are connected with the lipid peroxidation of cell
membranes (22). Additionally, an
increase in the aniline levels in the urine of the patients with
RCC was observed, which was consistent with the results of Gao
et al (22), who found
increased aniline levels in the blood of the patients with RCC. The
accumulation of another substituted benzene compound, phenol, may
accelerate the progress of RCC, as RCC is more commonly found in
patients with end-stage renal failure (23).
Humans regulate the balance of water and
electrolytes, and eliminate metabolic waste through urine. Ketones
were reported to be fairly abundant in human urine (24). Therefore, any impairment of kidney
function may significantly affect the excretion of ketones. Urinary
4-heptanone, a type of ketone, was consistently decreased in the
patients with RCC. The metabolic pathways of 4-heptanone is known.
In hemodialysis patients, di(2-ethylhexyl) phthalate, a
plasticizer, is rapidly metabolized to 2-ethylhexanol, which is
subsequently oxidized to 2-ethylhexanoic acid and finally to
4-heptanone (25). Halliwell et
al (26) reported that 4-heptanone
levels are increased in the blood and breath of end-stage renal
disease patients. The decrease in 4-heptanone levels found in the
urine of the RCC patients suggests that it is difficult for RCC
patients to excrete 4-heptanone though the urine; therefore,
4-heptanone remains in other tissues, leading to increased levels
in the blood and breath. However, the mechanism of this phenomenon
remains to be elucidated. Another decreased biomarker, styrene, is
a known carcinogenic environmental toxin. Styrene can attack
tissues by leaking into the cytoplasm and causing oxidative damage
to proteins (27). Decreased excretion
of this carcinogen in the urine can cause accumulation in the
kidneys, which leads to an increased risk of cancer.
Between the preoperative and postoperative patients
with RCC, three different biomarkers were obtained:
2-Ethyl-1-hexanol, cyclohexanone and
6-t-butyl-2,2,9,9-tetramethyl-3,5-decadien-7-yne. Cyclohexanone is
a uremic toxin (9) and levels have
been found increased in the blood of patients with end-stage renal
disease (26). Cyclohexanone levels
were increased in preoperative patients with RCC. Filipiak et
al (9) determined that certain
compounds, such as butyl acetate and 2-methylpropanal, are consumed
when tumor cells proliferate. We speculated that
6-t-butyl-2,2,9,9-tetramethyl-3,5-decadien-7-yne could also be
overly used by tumor consumption mechanisms. This increased
consumption may also account for the decreased levels of
6-t-butyl-2,2,9,9-tetramethyl-3,5-decadien-7-yne in preoperative
patients with RCC.
In conclusion, compared with the healthy subjects,
RCC has a unique VOC profile, suggesting that this profile may be
useful as a diagnostic assay for RCC.
Acknowledgements
Financial support included grants from the National
Natural Science Foundation of China (no. 81402462), China
Postdoctoral Science Foundation (no. 2013M531069), Foundation of
Heilongjiang Educational Committee (no. 12531245) and the Doctoral
Fund of the First Affiliated Hospital of Harbin Medical University
(no. 2012B006), which are gratefully acknowledged.
Glossary
Abbreviations
Abbreviations:
|
RCC
|
renal cell carcinoma
|
|
VOC
|
volatile organic compound
|
|
GC/MS
|
gas chromatography/mass
spectrometry
|
|
SPME
|
solid-phase microextraction
|
|
PCA
|
principal component analysis
|
|
PLSDA
|
partial least-squares discriminant
analysis
|
|
VIP
|
variable importance in the
projection
|
References
|
1
|
Ferlay J, Shin HR, Bray F, Forman D,
Mathers C and Parkin DM: Estimates of worldwide burden of cancer in
2008: GLOBOCAN 2008. Int J Cancer. 127:2893–2917. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Rini BI, Campbell SC and Escudier B: Renal
cell carcinoma. Lancet. 373:1119–1132. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Guo HF, Song Y and Na YQ: Value of
abdominal ultrasound scan, CT and MRI for diagnosing inferior vena
cava tumour thrombus in renal cell carcinoma. Chin Med J (Engl).
122:2299–2302. 2009.PubMed/NCBI
|
|
4
|
Khan AR, Anwar K, Fatima N and Khan SF:
Comparison of CT scan and colour flow Doppler ultrasound in
detecting venous tumour thrombous in renal cell carcinoma. J Ayub
Med Coll Abbottabad. 20:47–50. 2008.PubMed/NCBI
|
|
5
|
Rendon RA, Kapoor A, Breau R, Leveridge M,
Feifer A, Black PC and So A: Surgical management of renal cell
carcinoma: Canadian Kidney Cancer Forum Consensus. Can Urol Assoc
J. 8:E398–E412. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Altomare DF, Di Lena M, Porcelli F, Trizio
L, Travaglio E, Tutino M, Dragonieri S, Memeo V and de Gennaro G:
Exhaled volatile organic compounds identify patients with
colorectal cancer. Br J Surg. 100:144–150. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Ikeda A, Nishiumi S, Shinohara M, Yoshie
T, Hatano N, Okuno T, Bamba T, Fukusaki E, Takenawa T, Azuma T, et
al: Serum metabolomics as a novel diagnostic approach for
gastrointestinal cancer. Biomed Chromatogr. 26:548–558. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Wu H, Xue R, Dong L, Liu T, Deng C, Zeng H
and Shen X: Metabolomic profiling of human urine in hepatocellular
carcinoma patients using gas chromatography/mass spectrometry. Anal
Chim Acta. 648:98–104. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Filipiak W, Sponring A, Mikoviny T, Ager
C, Schubert J, Miekisch W, Amann A and Troppmair J: Release of
volatile organic compounds (VOCs) from the lung cancer cell line
CALU-1 in vitro. Cancer Cell Int. 8:172008. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Zambonin CG, Aresta A, Palmisano F,
Specchia G and Liso V: Liquid chromatographic determination of
urinary 5-methyl-2′-deoxycytidine and pseudouridine as potential
biological markers for leukaemia. J Pharm Biomed Anal.
21:1045–1051. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Sasco AJ, Rey F, Reynaud C, Bobin JY,
Clavel M and Niveleau A: Breast cancer prognostic significance of
some modified urinary nucleosides. Cancer Lett. 108:157–162. 1996.
View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Zheng YF, Yang J, Zhao XJ, Feng B, Kong
HW, Chen YJ, Lv S, Zheng MH and Xu GW: Urinary nucleosides as
biological markers for patients with colorectal cancer. World J
Gastroenterol. 11:3871–3876. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Yang J, Xu G, Zheng Y, Kong H, Pang T, Lv
S and Yang Q: Diagnosis of liver cancer using HPLC-based
metabonomics avoiding false-positive result from hepatitis and
hepatocirrhosis diseases. J Chromatogr B Analyt Technol Biomed Life
Sci. 813:59–65. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Ganti S and Weiss RH: Urine metabolomics
for kidney cancer detection and biomarker discovery. Urol Oncol.
29:551–557. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Jobu K, Sun C, Yoshioka S, Yokota J,
Onogawa M, Kawada C, Inoue K, Shuin T, Sendo T and Miyamura M:
Metabolomics study on the biochemical profiles of odor elements in
urine of human with bladder cancer. Biol Pharm Bull. 35:639–642.
2012. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Phillips M, Cataneo RN, Cummin AR,
Gagliardi AJ, Gleeson K, Greenberg J, Maxfield RA and Rom WN:
Detection of lung cancer with volatile markers in the breath.
Chest. 123:2115–2123. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Hietanen E, Bartsch H, Béréziat JC, Camus
AM, McClinton S, Eremin O, Davidson L and Boyle P: Diet and
oxidative stress in breast, colon and prostate cancer patients: A
case-control study. Eur J Clin Nutr. 48:575–586. 1994.PubMed/NCBI
|
|
18
|
Wang C, Li P, Lian A, Sun B, Wang X, Guo
L, Chi C, Liu S, Zhao W, Luo S, et al: Blood volatile compounds as
biomarkers for colorectal cancer. Cancer Biol Ther. 15:200–206.
2014. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Alwis KU, Blount BC, Britt AS, Patel D and
Ashley DL: Simultaneous analysis of 28 urinary VOC metabolites
using ultra high performance liquid chromatography coupled with
electrospray ionization tandem mass spectrometry (UPLC-ESI/MSMS).
Anal Chim Acta. 750:152–160. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Nicolaides N: Skin lipids: Their
biochemical uniqueness. Science. 186:19–26. 1974. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Broza YY, Kremer R, Tisch U, Gevorkyan A,
Shiban A, Best LA and Haick H: A nanomaterial-based breath test for
short-term follow-up after lung tumor resection. Nanomedicine.
9:15–21. 2013.PubMed/NCBI
|
|
22
|
Gao H, Dong B, Liu X, Xuan H, Huang Y and
Lin D: Metabonomic profiling of renal cell carcinoma:
High-resolution proton nuclear magnetic resonance spectroscopy of
human serum with multivariate data analysis. Anal Chim Acta.
624:269–277. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Mochalski P, Krapf K, Ager C, Wiesenhofer
H, Agapiou A, Statheropoulos M, Fuchs D, Ellmerer E, Buszewski B
and Amann A: Temporal profiling of human urine VOCs and its
potential role under the ruins of collapsed buildings. Toxicol Mech
Methods. 22:502–511. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Wahl HG, Hong Q, Hildenbrand S, Risler T,
Luft D and Liebich H: 4-Heptanone is a metabolite of the
plasticizer di(2-ethylhexyl) phthalate (DEHP) in haemodialysis
patients. Nephrol Dial Transplant. 19:2576–2583. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Mochalski P, King J, Haas M, Unterkofler
K, Amann A and Mayer G: Blood and breath profiles of volatile
organic compounds in patients with end-stage renal disease. BMC
Nephrol. 15:432014. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Halliwell B, Gutteridge JM and Cross CE:
Free radicals, antioxidants, and human disease: Where are we now? J
Lab Clin Med. 119:598–620. 1992.PubMed/NCBI
|
|
27
|
Thompson-Torgerson CS, Champion HC,
Santhanam L, Harris ZL and Shoukas AA: Cyclohexanone contamination
from extracorporeal circuits impairs cardiovascular function. Am J
Physiol Heart Circ Physiol. 296:H1926–H1932. 2009. View Article : Google Scholar : PubMed/NCBI
|