Introduction
Acute coronary syndrome (ACS), one of the most
common severe cardiovascular diseases, is a type of severe coronary
heart disease that is associated with high rates of mortality and
disability (1). ACS is classified
as either acute myocardial infarction (AMI) or unstable angina
pectoris (UAP), and the classification is based on vulnerable
plaque rupture accompanied by complete or incomplete artery
occlusion (2). Evaluation of the
characteristics of coronary atherosclerotic plaques and the extent
of coronary artery lesions can enable early diagnosis of ACS. At
present, intracoronary ultrasound and coronary angiography can be
used for the detection of coronary atherosclerotic plaques.
However, these two methods are not widely applied in the clinic as
they are expensive and invasive, and require improvements (3).
Estrogen, a female hormone, not only promotes growth
and development, but also has a role in various systems of the
human body (4). High-sensitivity
C-reactive protein (hs-CRP) is produced by hepatocytes and is
involved in inflammation. Clinical studies have demonstrated that
hs-CRP levels can be used as predictors of cardiovascular disease
(5). Matrix metalloproteinase 9
(MMP-9, also known as gelatinase B), which has numerous substrates,
is involved in a wide range of physiological functions, including
regulation of protease and cytokine activity (6). In addition, MMP-9 plays a role in
elastin degradation, which promotes breakdown of the thin, fibrous
caps of plaques (7). The aim of
the present study was to explore an economic, convenient and
non-invasive method to evaluate the extent of coronary artery
lesions and to analyze the correlation between estrogen, hs-CRP and
MMP-9 levels and the severity of coronary artery lesions.
Subjects and methods
Subjects
From March 2011 to March 2012, 65 patients with ACS
diagnosed by coronary angiography, including 30 patients with AMI
and 35 patients with UAP, were randomly enrolled from the First
Affiliated Hospital of Xinxiang Medical University (Weihui, China).
A total of 33 patients with stable angina pectoris (SAP) and 36
healthy individuals were also included. Exclusion criteria included
hepatic or renal dysfunction, thyroid disease, cancer, autoimmune
disease, chronic bronchitis and asthma. The mean age of the
patients with AMI (16 male, 14 female) was 61.46±9.37 years, with a
range of 51–73 years. The mean age of the patients with UAP (19
male, 16 female) was 60.92±10.79 years, with a range of 49–74
years. The mean age of the patients with SAP (16 male, 17 female)
was 61.13±11.05 years, with a range of 50–72 years. The mean age of
the healthy subjects (19 male, 17 female) was 61.71±11.88 years,
with a range of 49–74 years. There were no significant differences
in age and gender among the four groups (P>0.05). This study was
conducted in accordance with the Declaration of Helsinki, and
approval was obtained from the Ethics Committee of the First
Affiliated Hospital of Xinxiang Medical University. Written
informed consent was obtained from all subjects
Methods
Venous blood samples (4 ml) were obtained from all
subjects following an overnight fast. The blood samples were
centrifuged at 5,000 × g for 10 min and the supernatants were
stored at -30°C. ELISA was used to detect serum levels of estrogen,
hs-CRP and MMP-9 (8–10). Coronary angiography was performed
in all patients, including healthy subjects, according to the
Judkins technique (11). Two
experienced interventional cardiologists assessed the extent of
coronary artery lesions and the number of stenosed coronary
vessels. To assess the extent of coronary artery lesions, the
diameter of the proximal coronary artery was measured. Patients
were classified as having mild (50–70% lesion), moderate (71–90%
lesion), severe (91–99% lesion) or total occlusion (100% lesion).
Coronary artery stenosis was defined as ≥50% narrowing of vessels
Left main coronary artery stenosis was calculated as two-vessel
coronary artery stenosis.
Statistical analysis
Version 17.0 of the SPSS statistical software
package (SPSS, Inc., Chicago, IL, USA) was used for all statistical
analysis. Multiple groups were compared using analysis of variance.
Correlations were analyzed using linear correlation analysis and
Spearman’s rank correlation analysis. P<0.05 was considered to
indicate a statistically significant difference.
Results
Comparison of serum levels of estrogen,
hs-CRP and MMP-9
Serum estrogen levels were significantly lower in
patients with AMI (52.31±8.94 ng/l), UAP (58.72±8.21 ng/l) and SAP
(61.93±8.69 ng/l) compared with the control group (82.16±9.85 ng/l;
P<0.05). Estrogen levels were also significantly different among
the AMI, UAP and SAP groups (P<0.05). Compared with the control
group (2.31±1.54 mg/l), the AMI (7.16±2.82 mg/l), UAP (5.77±2.33
mg/l) and SAP groups (3.38±1.72 mg/l) had significantly higher
serum hs-CRP levels (P<0.05). Serum hs-CRP levels were also
significantly different among the AMI, UAP and SAP groups
(P<0.05). Serum MMP-9 levels were significantly higher in
patients with AMI (347.86±22.58 ng/ml), UAP (283.95±19.51 ng/ml)
and SAP (195.32±18.46 ng/ml) compared with the control group
(123.89±18.08 ng/ml; P<0.05). MMP-9 levels were also
significantly different among the AMI, UAP and SAP groups
(P<0.05) (Table I).
 | Table ISerum levels of estrogen, hs-CRP and
MMP-9 in the AMI, UAP, SAP and control groups. |
Table I
Serum levels of estrogen, hs-CRP and
MMP-9 in the AMI, UAP, SAP and control groups.
| Groups | Estrogen (ng/l) | hs-CRP (mg/l) | MMP-9 (ng/ml) |
|---|
| AMI (n=30) | 52.31±8.94a–c | 7.16±2.82a–c | 347.86±22.58a–c |
| UAP (n=35) | 58.72±8.21a,b | 5.77±2.33a,b | 283.95±19.51a,b |
| SAP (n=33) | 61.93±8.69a | 3.38±1.72a | 195.32±18.46a |
| Control (n=36) | 82.16±9.85 | 2.31±1.54 | 123.89±18.08 |
Correlation analysis between serum levels
of estrogen, hs-CRP and MMP-9
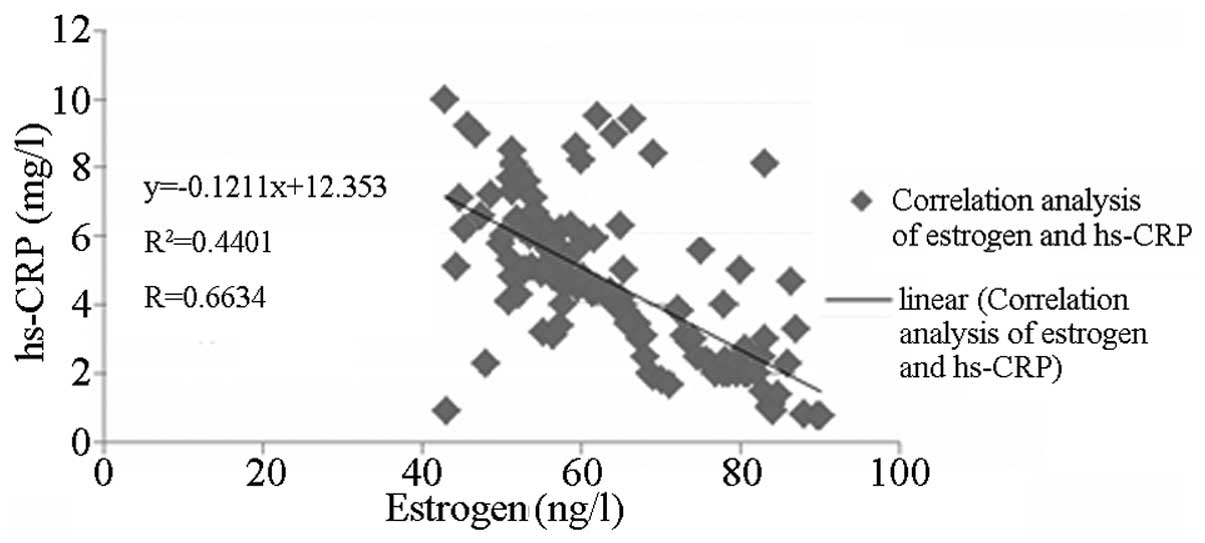
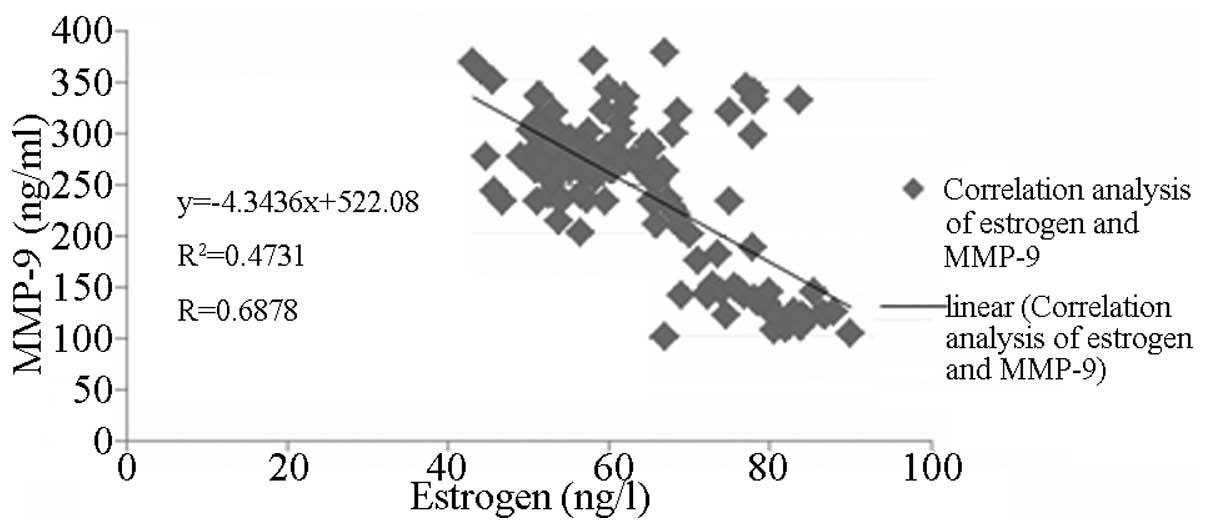
As shown in Figs. 1
and 2, serum estrogen levels were
negatively correlated with hs-CRP and MMP-9 levels (r=−0.6634 and
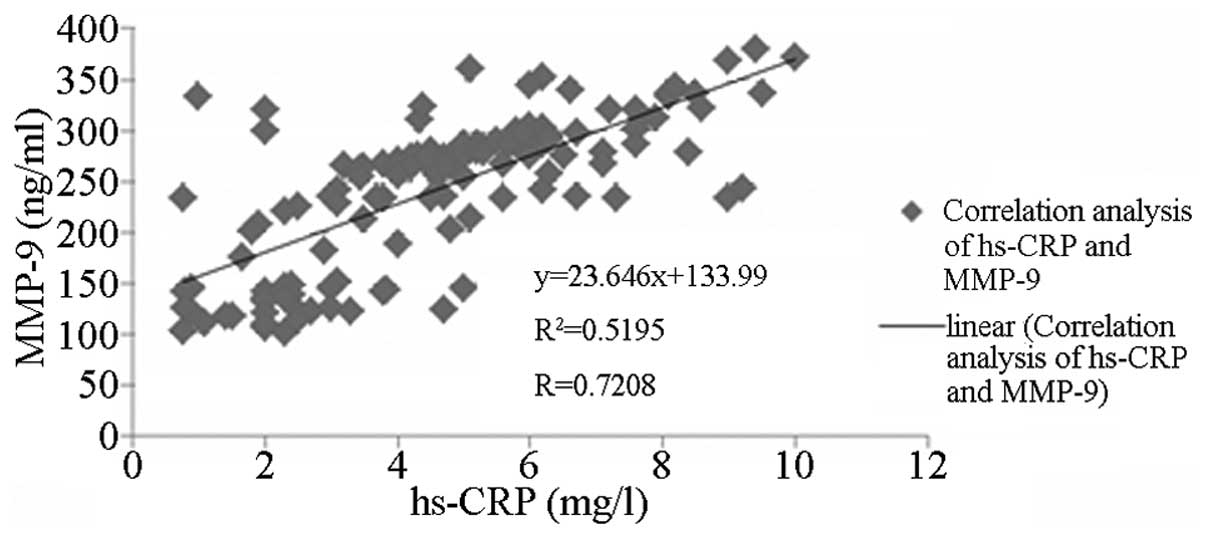
−0.6878, respectively; both P<0.05). As shown in Fig. 3, hs-CRP and MMP-9 levels correlated
positively (r=0.7208, P<0.05).
Correlation analysis between the number
of stenosed coronary vessels and serum levels of estrogen, hs-CRP
and MMP-9
Estrogen levels were significantly different among
patients with one-, two- and three-vessel disease. The number of
stenosed coronary vessels correlated negatively with estrogen
levels (r=-0.6467, P<0.05) and positively with hs-CRP and MMP-9
levels (r=0.6519 and 0.6835, respectively; both P<0.05)
(Table II).
 | Table IISerum levels of estrogen, hs-CRP and
MMP-9 in patients with one-, two- and three-vessel disease. |
Table II
Serum levels of estrogen, hs-CRP and
MMP-9 in patients with one-, two- and three-vessel disease.
| Disease type | Estrogen (ng/l) | hs-CRP (mg/l) | MMP-9 (ng/ml) |
|---|
| One-vessel
(n=12) | 56.04±8.80 | 3.63±1.54 | 236.24±19.50 |
| Two-vessel
(n=29) | 53.72±9.56a | 5.84±1.79a | 268.54±19.31a |
| Three-vessel
(n=24) | 49.87±9.06a,b | 7.47±2.36a,b | 302.73±20.62a,b |
Discussion
ACS describes a spectrum of clinical symptoms that
result from acute myocardial ischemia, including AMI and UAP
(12). It has been indicated that
instability of coronary atherosclerotic plaques plays an important
role in the pathogenesis of ACS. Erosion or rupture of coronary
plaques, leading to partial or complete obstruction of the coronary
artery, results in AMI or angina pectoris (13,14).
In clinical practice, early diagnosis of the stability of plaques
and the severity of coronary artery lesions is important for
patients with ACS. As current diagnostic approaches for ACS are
invasive and expensive, non-invasive and cost-efficient methods for
the diagnosis of ACS are being widely explored. At present, few
studies have investigated the correlation between severity of
coronary artery lesions and serum levels of estrogen, hs-CRP and
MMP-9. This study investigated the correlation between the severity
of coronary artery lesions and serum levels of estrogen, hs-CRP and
MMP-9 in patients with ACS.
Estrogen, an important hormone, possesses a wide
spectrum of biological activities. In addition to its role in
reproduction, estrogen affects the endocrine, cardiovascular and
metabolic systems. It has been observed that the incidence of
coronary heart disease in pre-menopausal females is significantly
lower than that in post-menopausal females and males (15). In the present study, serum estrogen
levels in patients with coronary artery disease were significantly
lower than those in healthy subjects. Serum estrogen levels
progressively increased across the AMI, UAP and SAP groups,
respectively, while a progressive decrease occurred across the
one-, two- and three-vessel disease subgroups, respectively.
hs-CRP, an indicator of inflammatory states, is involved in the
pathogenesis of atherosclerosis. Levels of hs-CRP change with
coronary artery plaque characteristics, and hs-CRP is also a
predictor of coronary artery disease-associated mortality (16). MMP-9, an important member of the
matrix metalloproteinase family, is involved in the invasion and
metastasis of cancer cells, inflammation and angiogenesis, as well
as the initiation and development of atherosclerosis (17). Park et al (18) demonstrated that MMP-9 levels were
significantly higher in patients with vulnerable atherosclerotic
plaques than in patients without vulnerable atherosclerotic
plaques, indicating that MMP-9 levels were closely associated with
vulnerable atherosclerotic plaques. In the present study, highest
levels of hs-CRP and MMP-9 were observed in patients with AMI,
followed by those with UAP and SAP, respectively. Levels of hs-CRP
and MMP-9 progressively increased across the one-, two- and
three-vessel disease groups. Correlation analyses demonstrated that
levels of estrogen, hs-CRP and MMP-9 were significantly correlated
with the number of stenosed coronary vessels, and there was also a
correlation between levels of estrogen, hs-CRP and MMP-9. These
results indicate that levels of estrogen, hs-CRP and MMP-9 are
associated with the severity of coronary artery lesions and the
stability of coronary artery plaques in patients with ACS, which is
consistent with previous studies (17–19).
Compared with patients with SAP, patients with ACS had a greater
number of vulnerable and unstable atherosclerotic plaques in which
inflammation was more active.
In conclusion, there is a significant correlation
between levels of estrogen, hs-CRP and MMP-9, which can be used as
biomarkers to evaluate the severity of coronary artery lesions and
to predict the stability of coronary artery plaques.
References
|
1
|
Harutyunyan M, Gøtze JP, Winkel P, et al:
Serum YKL-40 predicts long-term mortality in patients with stable
coronary disease: a prognostic study within the CLARICOR trial.
Immunobiology. 218:945–951. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Falcone C, Lucibello S, Mazzucchelli I, et
al: Galectin-3 plasma levels and coronary artery disease: a new
possible biomarker of acute coronary syndrome. Int J Immunopathol
Pharmacol. 24:905–913. 2011.PubMed/NCBI
|
|
3
|
Sakamoto Y, Muramatsu T, Tsukahara R, Ito
Y, Ishimori H, Hirano K and Nakano M: A case achieved successful
revascularization to severe ischemic coronary artery disease after
endovascular recanalization with infrarenal aortic occlusion.
Cardiovasc Interv Ther. 27:93–98. 2012. View Article : Google Scholar
|
|
4
|
Oh JE, Kim YW, Park SY and Kim JY:
Estrogen rather than progesterone cause constipation in both female
and male mice. Korean J Physiol Pharmacol. 17:423–426. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Seo SM, Baek SH, Jeon HK, et al:
Correlations between the level of high-sensitivity c-reactive
protein and cardiovascular risk factors in korean adults with
cardiovascular disease or diabetes mellitus: the CALLISTO study. J
Atheroscler Thromb. 20:616–622. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Yabluchanskiy A, Ma Y, Iyer RP, Hall ME
and Lindsey ML: Matrix metalloproteinase-9: Many shades of function
in cardiovascular disease. Physiology (Bethesda). 28:391–403.
2013.PubMed/NCBI
|
|
7
|
Duellman T, Warren CL, Peissig P, Wynn M
and Yang J: Matrix metalloproteinase-9 genotype as a potential
genetic marker for abdominal aortic aneurysm. Circ Cardiovasc
Genet. 5:529–537. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Miller VM, Petterson TM, Jeavons EN, et
al: Genetic polymorphisms associated with carotid artery
intima-media thickness and coronary artery calcification in women
of the Kronos Early Estrogen Prevention Study. Physiol Genomics.
45:79–88. 2013. View Article : Google Scholar
|
|
9
|
Rashidinejad H, Hosseini SM, Moazenzadeh
M, Azimzadeh BS, Mirzaeipour F, Fakhreddini K and Sheikhvatan M:
Relationship between serum level of high-sensitive C-reactive
protein and extension of myocardial involvement in patients with
acute myocardial infarction. Rom J Intern Med. 50:211–215.
2012.PubMed/NCBI
|
|
10
|
Golovkin AS, Matveeva VG, Grigor’ev EV,
Baĭrakova IuV, Shukevich DL, Velikanova EA and Barbarash OL:
Postoperative dynamic changes in matrix metalloproteinase levels in
patients with coronary artery bypass graft procedure complications.
Kardiologiia. 52:4–7. 2012.(In Russian).
|
|
11
|
Salama MM, Morad AR, Saleh MA, Sabri NA,
Zaki MM and ElSafady LA: Resistance to low-dose aspirin therapy
among patients with acute coronary syndrome in relation to
associated risk factors. J Clin Pharm Ther. 37:630–636. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Kehl DW, Iqbal N, Fard A, Kipper BA, De La
Parra Landa A and Maisel AS: Biomarkers in acute myocardial injury.
Transl Res. 159:252–264. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Cristell N, Cianflone D, Durante A, et al:
High-sensitivity C-reactive protein is within normal levels at the
very onset of first ST-segment elevation acute myocardial
infarction in 41% of cases: a multiethnic case-control study. J Am
Coll Cardiol. 58:2654–2661. 2011.PubMed/NCBI
|
|
14
|
Akhtar N, Adil MM, Ahmed W,
Habib-ur-Rehman and Shahs MA: The role of leukocyte counts in
patients with unstable angina pectoris or myocardial infarction;
prognostic significance and correlation with plasma brain
natriuretic peptide (BNP) levels. J Pak Med Assoc. 61:51–54.
2011.
|
|
15
|
Huang G, Wang D, Zeb I, et al:
Intra-thoracic fat, cardiometabolic risk factors, and subclinical
cardiovascular disease in healthy, recently menopausal women
screened for the Kronos Early Estrogen Prevention Study (KEEPS).
Atherosclerosis. 221:198–205. 2012. View Article : Google Scholar
|
|
16
|
Mirhosseini SJ, Forouzannia SK,
Ali-Hassan-Sayegh S, Ravan HV, Abdollahi MH and Mozayan MR:
Preoperative C-reactive protein can predict early clinical outcomes
following elective off-pump CABG surgery in patients with severe
left ventricle dysfunction. Saudi J Anaesth. 6:327–331. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Crăciunescu I, Serban M, Iancu M, et al:
Changes in plasma levels of MMP-9, MMP-7 and their inhibitors in
patients with coronary artery disease. Rom J Intern Med.
48:141–149. 2010.PubMed/NCBI
|
|
18
|
Park JP, Lee BK, Shim JM, Kim SH, Lee CW,
Kang DH and Hong MK: Relationship between multiple plasma
biomarkers and vulnerable plaque determined by virtual histology
intravascular ultrasound. Circ J. 74:332–336. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Datta S, Iqbal Z and Prasad KR: Comparison
between serum hsCRP and LDL cholesterol for search of a better
predictor for ischemic heart disease. Indian J Clin Biochem.
26:210–213. 2011. View Article : Google Scholar : PubMed/NCBI
|