Introduction
A dural arteriovenous fistula (DAVF) refers to an
abnormal direct blood connection between an intracranial artery and
the dural venous sinus, and accounts for 10–15% of all intracranial
vascular malformations (1). It is
known that there are congenital and acquired causes of DAVF. The
majority of cases of DAVF are congenital and caused by dural
vascular abnormalities. However, certain cases of DAVF are acquired
and may be caused by brain trauma, venous sinus inflammation,
venous sinus thrombosis formation, brain surgery, hypercoagulable
states and others. DAVFs most commonly occur in the cavernous
sinus, transverse sinus, sigmoid sinus and superior sagittal sinus.
The main treatment for DAVF is endovascular embolization (2). The principle of DAVF treatment is the
‘permanent and complete occlusion of the fistula’. However, in
certain cases (including cortical venous reflux disease DAVF and
wide DAVF) the DAVF cannot be completely cured, so the goal of
treatment changes to reduce the rate of bleeding and relieve
clinical symptoms. Treatments for DAVF include endovascular
embolization, vascular compression, surgery and stereotactic
treatment. With the development of modern materials and devices,
endovascular treatment has become the main method for DAVF
treatment (2). Endovascular
interventional embolization treatment includes transartery
embolization, transvenous embolization and the united arteriovenous
approach. The main clinical manifestations of DAVF depend on the
position of the venous drainage, drainage direction, velocity and
the position of the fistula. DAVF manifestations of ophthalmic vein
drainage are headaches, exophthalmos and conjunctival congestion;
cortical venous drainage in patients is usually manifested as local
neurological dysfunction and brain hemorrhage (3). A previous study observed that lesions
in the craniocervical junction region, frequently to the brain stem
vein, and cervical spinal perimedullary venous drainage revealed
subarachnoid hemorrhage (4). DAVFs
have various clinical manifestations, but rarely present as
parkinsonism and dementia. Therefore, DAVFs are easily
misdiagnosed. The present study reports the case of a DAVF
manifesting as parkinsonism and dementia, and reviews the relevant
literature.
Case report
Written informed consent was obtained from the
patient’s family for inclusion in the present case report. A
62-year-old male was admitted to hospital after presenting with
progressive limb stiffness and weakness for five months, as well as
memory loss and unstable walking for two weeks. Five months prior
to admission, the patient developed limb stiffness and weakness
with no incentive, particularly when going downhill. In addition,
the patient exhibited slow movements, which sequentially involved
the upper limbs, but without an evident tremor. No treatment was
administered during this period. At two weeks prior to admission,
the patient presented with aggravated limb stiffness and weakness,
walking instability (rushing forward and difficulty stopping when
walking), memory loss (the performance of forgetting commonly used
figures and short-term memory loss), apathy and urinary
incontinence. The patient had been hospitalized at a local hospital
and was diagnosed with cerebral infarction and Parkinson’s disease;
however, no treatment was administered after improving the
circulation and anti-Parkinson therapy. Thereafter, the patient was
transferred to the Tianjin Fifth Central Hospital (Tianjin, China)
for further diagnosis and treatment.
The patient had a history of hypertension for 10
years, coronary heart disease and atrial fibrillation for five
years, and had undergone coronary stenting, but had no history of
encephalitis, traumatic brain injury or poisoning. On examination,
the patient exhibited a blood pressure of 150/80 mmHg, an irregular
heartbeat, clear consciousness, apathy, slurred speech,
disorientation, memory loss and decreased comprehension and
calculation abilities. The patient scored 11 points on the
mini-mental state examination. Muscle strength in four limbs was
slightly lower than normal with limb hypermyotonia, particularly in
the lower limbs. Babinski’s sign (−) was observed on both feet. The
patient walked forward with fewer movements and postural
instability, and was classified with Hoehn-Yahr stage III of
Parkinson’s disease. Cranial magnetic resonance imaging (MRI)
revealed long T1 and T2 signals in the bilateral frontal lobes, a
high FLAIR signal, an enlarged vascular shadow at the meninges of
the left temporal lobe and mild cerebral atrophy (Fig. 1A and B). Computed tomography
angiography (CTA) revealed multiple vermiform enlarged vessels on
the left cerebral hemisphere and the right frontal and parietal
brain surface, considered to be a left temporal DAVF (Fig. 1C and D). Furthermore, an
electroencephalography revealed frontotemporal slow waves, and a
lumbar puncture examination showed normal pressure in the
cerebrospinal fluid, which was l40 mm H2O, while the
cerebrospinal fluid cellular and biochemical tests were normal.
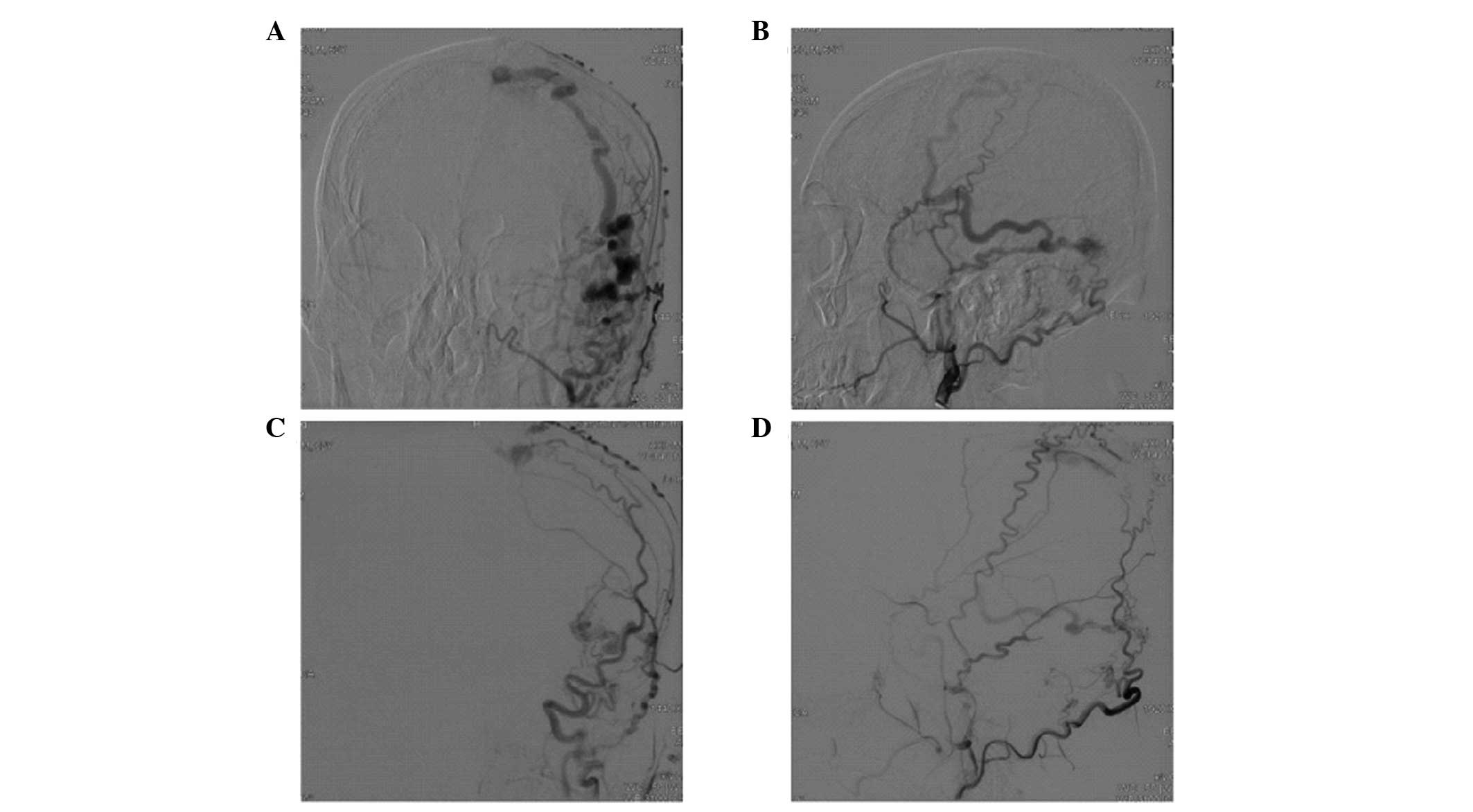
The patient was initially diagnosed with
parkinsonism, vascular dementia and a DAVF. Digital subtraction
angiography (DSA) revealed a DAVF in the left temporal region, fed
by the bilateral middle meningeal arteries and meningeal branches
of the vertebral artery, which were enlarged abnormally, with poor
venous reflux to the superior sagittal sinus (Fig. 2A and B). The patient was treated
with transarterial embolization therapy. Following general
anesthesia, a Malathon microcatheter was inserted into the left
branch of the middle meningeal artery, guided by a Mirage 0.008
microwire, and the tip of the microcatheter was close to the
fistula. Thereafter, Onyx-l8 glue (~1.5 ml), was slowly injected
for embolization. Intraoperative angiography showed almost complete
embolization of the DAVF, and the venous reflux was slower than
before (Fig. 2C and D). At day 3
following surgery, the condition of the patient improved. In
comparison with the preoperative conditions, the muscle tension of
the bilateral limbs was significantly decreased, movement during
walking was improved, the walking start and leg speed were faster
and turn-back and cognitive function had improved. In addition, at
two weeks post-surgery, the memory ability of the patient had
recovered to the level prior to onset, and the gait was stable.
Scores of the mini-mental state examination were up to 25 points,
and the Hoehn-Yahr level was stage I. At discharge, the patient was
diagnosed with a left temporal DAVF.
Discussion
DAVFs can be developed at all ages, but are most
common in individuals aged between 60 and 70 years. The ratio of
females to males with a DAVF is 1:1.65 (5). DAVFs are mainly fed by the external
carotid artery; however, the internal carotid and meningeal
branches of the vertebral artery can be involved. In the present
case, the branches of the external carotid artery and meningeal
branches of the vertebral artery fed the DAVF. Venous sinus
hypertension is considered to be the leading cause of an acquired
DAVF (6). A physiological
arteriovenous access exists between the network of dural arteries
and the dural sinus. Under venous hypertension, the physiological
arteriovenous channels around the venous sinus remain open, and a
pathological arteriovenous shunt forms and attracts a large number
of middle meningeal arteries involved in the blood supply through
enriched tiny arteries from the dural wall, forming a DAVF
(7,8). Poor reflux of the superior sagittal
sinus in the present case may be the initiating factor of the
temporal DAVF.
DAVFs are often involved in the transverse sinus and
sigmoid sinus, followed by the cavernous sinus and superior
sagittal sinus, but are rarely found in the straight sinus, with
complex and diverse clinical manifestations, but no significant
specificity. In the present case, the symptoms of the DAVF were
progressive parkinsonism and dementia, which is rare and has been
rarely reported (9,10). The initial symptoms were
progressive limb stiffness and weakness with symmetrical onset;
however, there was no significant limb tremor, abnormal posture and
difficulty in starting to walk. Soon afterwards, the patient
presented with progressive memory loss, behavioral abnormalities
and a decline in activities of daily living, which were more in
line with the clinical diagnosis of Parkinson’s disease and
dementia. A number of pathophysiological mechanisms were considered
to cause the present case of DAVF, which resulted in parkinsonism
and dementia. Firstly, the direct connection between the arterial
fistula and the superior sagittal sinus caused a partial arterial
steal phenomenon that led to frontal, temporal lobe and basal
ganglia ischemia, among which, frontal white matter and basal
ganglia damage triggered parkinsonism (11), while dementia was generated from
the involvement of the frontal and temporal lobe. Secondly,
localized venous hypertension, venous congestion and decreased
cerebral perfusion due to abnormal venous return caused local
ischemia and hypoxia, which resulted in the release of vascular
endothelial growth factor and induced angiogenesis. Finally,
parkinsonism and dementia may have been the result of cerebral
compression by dilated veins in the frontotemporal area.
Due to varying nonspecific clinical manifestations,
the diagnosis of a DAVF is often based on imaging studies (12). Diagnosis is difficult using cranial
CT; however, this imaging technique can reveal certain secondary
changes caused by a DAVF, including venous sinus thrombosis, acute
and sub-acute subarachnoid hemorrhage and subdural or cerebral
hemorrhage. However, cranial MRI is better compared with CT for the
detection of DAVF-induced secondary changes, and is useful to show
the extensive flow void phenomenon (Fig. 1A). In addition, with a serious
condition, MRI can display tortuously enlarged cortical veins
(Fig. 1B). In the present case,
the patient was misdiagnosed prior to admission to the Tianjin
Fifth Central Hospital. An abnormal flow void area was identified
in the left temporal lobe from the cranial MRI films, and
subsequently CTA and DSA were essential for the final diagnosis.
CTA and MRI show abnormal enlarged feeding arteries, dilated veins
and dural sinuses, but are unable to reveal the situation of the
fistula or the existence of potential anastomosis and small feeding
arteries. DSA is better for demonstrating the characteristics of a
DAVF, including the site of the fistula, feeding features and
venous return, and even can indirectly demonstrate the degree of
fistula blood flow and intracranial hemodynamic characteristics
(13).
The treatment methods for DAVFs include
embolization, vascular compression, surgery and stereotactic
treatment. In addition, with the invention of novel materials and
devices, endovascular therapy has become the primary method for
DAVF treatment. The treatment principle is to occlude the dural
venous fistula. Theoretically, it is better to directly embolize
the fistula by transvenous embolization, as this is easier to
achieve an anatomic cure. The arterial approach is a substitute for
the intravenous approach, and is used for patients without venous
sinus drainage, with sinus stenosis or if the fistula is simply fed
by the branches of the external carotid artery or the non-tortuous
enlarged feeding artery (14).
Onyx glue is often selected as the embolic material since it
exhibits excellent dispersibility, is not easily broken up or
adheres to a microcatheter and is easy to control. The maximum
degree of embolization can be obtained with curative outcomes
(15). In the present case, a
microcatheter was inserted into the fistula of the middle meningeal
artery and Onyx-l8 glue was slowly injected, ultimately achieving
embolization. Following surgery, the symptoms of parkinsonism and
dementia were significantly reduced, and the neurological function
and scores on the dementia scale showed a substantial increase over
the preoperative evaluation. After one month, the patient was able
to take care of himself completely, and after three months, a
stereotactic treatment was performed for the residual fistula. At
the one year follow-up, neurological examination revealed that the
patient was recovering normally.
In conclusion, a DAVF presenting as parkinsonism and
dementia is easily misdiagnosed. However, a timely diagnosis is
crucial for improved therapeutic outcomes. In cases of rapidly
progressive parkinsonism or dementia, accompanied by an abnormal
flow void shadow on cranial MRI films, the possibility of a DAVF
should be considered. Subsequently, the DAVF should be treated with
appropriate and timely selective endovascular treatment, with DSA
recommended as soon as possible.
Acknowledgements
The study was supported by grants from the
Health-System Science Foundation of Binhai New Area in Tianjin (no.
2012BWKL001) and the Science-Technology Developmental Foundation of
Binhai New Area in Tianjin (no. 2012MS05-04).
References
|
1
|
Jahan R, Gobin YP, Glenn B, Duckwiler GR
and Viñuela F: Transvenous embolization of a dural arteriovenous
fistula of the cavernous sinus through the contralateral pterygoid
plexus. Neuroradiology. 40:189–193. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Cha KC, Yeon JY, Kim GH, Jeon P, Kim JS
and Hong SC: Clinical and angiographic results of patients with
dural arteriovenous fistula. J Clin Neurosci. 20:536–542. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Kuwayama N, Kubo M, Tsumura K, Yamamoto H
and Endo S: Hemodynamic status and treatment of aggressive dural
arteriovenous fistulas. Acta Neurochir Suppl. 94:123–126. 2005.
View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Kai Y, Hamada J, Morioka M, et al:
Arteriovenous fistulas at the cervicomedullary junction presenting
with subarachoid hemorrhage: six case reports with special
Reference to the angiographic pattern of venous drainage. AJNR Am J
Neuroradiol. 26:1949–1954. 2005.PubMed/NCBI
|
|
5
|
He HW, Jiang CH, Wu ZX, Li YX and Wang ZC:
Transvenous embolization of cavernous dural arteriovenous fistula:
report of 28 cases. Clin Med J (Engl). 120:2229–2232. 2007.
|
|
6
|
Chen L, Mao Y and Zhou LF: Local chronic
hypoperfusion secondary to sinus high pressure seems to be mainly
responsible for the formation of intracranial dural arteriovenous
fistula. Neurosurgery. 64:973–983. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Tsai LK, Jeng JS, Liu HM, Wang HJ and Yip
PK: Intracranial dural arteriovenous fistulas with or without
cerebral sinus thrombosis: analysis of 69 patients. J Neurol
Neurosurg Psychiatry. 75:1639–1641. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Xavier J, Cruz R, Stocker A, et al: Dural
fistulas of the anterior cranial fossa. Acta Med Port. 14:71–75.
2001.(In Portuguese). PubMed/NCBI
|
|
9
|
Kajitani M, Yagura H, Kawahara M, et al:
Treatable fluctuating Parkinsonism and dementia in a patient with a
dural arteriovenous fistula. Mov Disord. 22:437–439. 2007.
View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Matsumura A, Oda M, Hozuki T, Imai T and
Shimohama S: Dural arteriovenous fistula in a case of dementia with
bithalamic MR lesions. Neurology. 7l:l5532008.
|
|
11
|
Yamanouchi H and Nagura H: Neurological
signs and frontal white matter lesions in vascular Parkinsonism. A
clinicopathological study. Stroke. 28:965–969. 1997. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Gandhi D, Chen J, Pearl M, et al:
Intracranial dural arteriovenous fistulas: classification, imaging
findings, and treatment. AJNR Am J Neuroradiol. 33:1007–1013. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Ming Y, Zhong L, Ze Y, et al: Comparison
among CT, MRI and DSA features of dural ateriovenous fistula.
Zhongguo Linchuang Shenjing Waike Zazhi. 11:201–203. 2006.(In
Chinese).
|
|
14
|
Pelz DM, Lownie SP, Fox AJ and Rosso D:
Intracranial dural arteriovenous fistulae with pial venous
drainage: combined endovascular-neurosurgical therapy. Can J Neurol
Sci. 24:210–218. 1997.PubMed/NCBI
|
|
15
|
Jiang C, Lv X, Li Y, Zhang J and Wu Z:
Endovascular treatment of high-risk tentorial dural arteriovenous
fistulas: clinical outcomes. Neuroradiology. 51:103–111. 2009.
View Article : Google Scholar
|