Introduction
Bladder exstrophy is typically associated with a
specific set of conditions, including epispadias, hernia and pelvic
malformation. This spectrum of abnormalities is known as the
exstrophy-epispadias complex (EEC) (1). It is estimated that EEC occurs in
~1/35,000 live births (2), and the
risk of bladder carcinoma in the EEC population is 700-times higher
compared with that of the age-matched general population (3). Ideally the management of EEC is
initiated in the neonatal period, as malignant potential increases
with age if the condition remains untreated (4). As the majority of patients with EEC are
treated when they are infants, adult cases of EEC are rarely
reported.
Case report
A 32-year-old man with bladder exstrophy was
referred to the Second Xiangya Hospital of Central South University
(Changsha, China) in February 2013, having received no previous
surgical intervention. The patient complained of intermittent
bladder pain and bleeding, and complete incontinence that required
the continual use of diapers. Since adolescence, the patients penis
had exhibited a limited degree of development; however, it was able
to enlarge and eject seminal fluid in response to sexual
stimulation.
A physical examination revealed that the umbilicus
was absent, replaced by a scarlet-colored bladder plate of 5×6 cm,
which was partially thickened and exhibited mucosal erosion. The
ureters opened at each side of the lower part of the bladder plate,
and clear urine was release intermittently from each ureter. A 2-cm
long epispadias penis with a splayed glans was present beneath the
bladder plate. The left testicle was impalpable and the right was
normal. A number of painless enlarged lymph nodes were identified
in the left inguinal area. The perineum was shortened as the anus
was located immediately behind the scrotum. Numerous reddish
broad-based neoplasms were identified on the bladder plate
(Fig. 1).
Laboratory analysis, including routine blood tests,
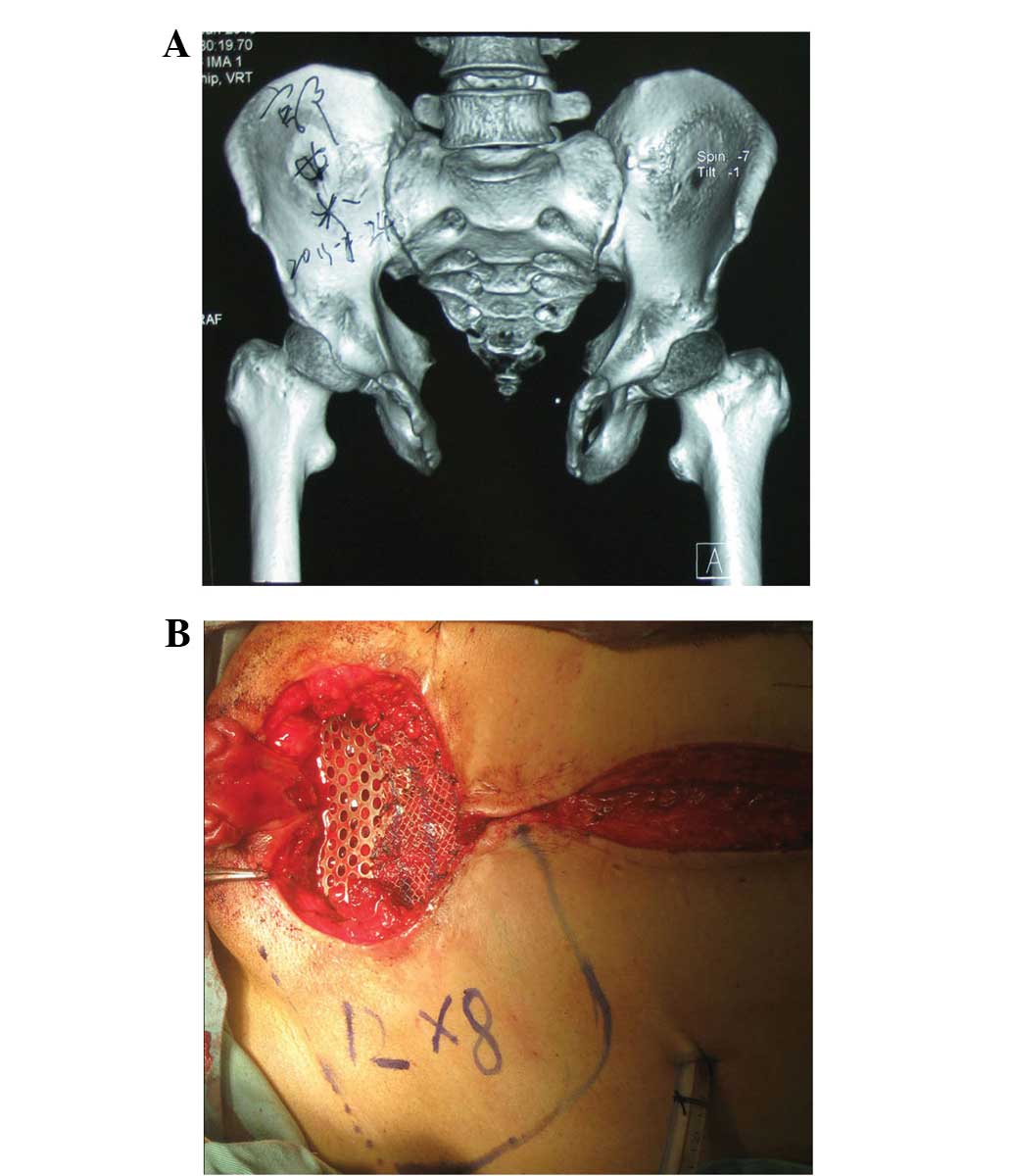
indicated no abnormalities in renal or liver function. X-ray
examination showed a separation of the symphysis pubis of ≤102 mm
(Fig. 2). Computed tomography
scanning revealed that the bladder cavity was absent and the
bladder plate was thickened and protruded, and a hernia protruding
into the left scrotum chamber was confirmed. Magnetic resonance
imaging showed no enhancement of the bladder plate and the signal
of the prostate was homogenous, indicating no abnormality. No
enlarged lymph nodes were observed in the pelvic cavity.
Ultrasonography indicated normal bilateral kidneys and adrenal
glands. A biopsy of the bladder plate neoplasms revealed severe
atypical hyperplasia with well-differentiated adenocarcinoma. No
other abnormalities or tumor sites were detected.
The patient underwent radical cystectomy and urinary
diversion with a ileal conduit, and an expanded local
lymphadenectomy was performed. Subsequently, a 10×8-cm gap was
present in the lower abdomen. Osteotomy was not performed; instead
a customized titanium mesh was applied to bridge the gap. The mesh
was fixed to the pubic and ischial ramus, and an onlay mesh repair
was performed to correct the hernia (Fig. 2).
A 12×8-cm lower abdominal island skin flap was
specifically designed, the pedicle of which was located in the left
inguinal region. The flap was rotated ~45° to cover the skin of the
defective area.
The reconstruction of the penis was not conducted,
but postponed until following the successful completion of the
current surgery.
Postoperative pathological examination revealed that
the bladder tumor was a well-differentiated adenocarcinoma. No
cancer tissue was detected in the resected prostate or lymph nodes.
Following surgery, no adjuvant therapy was applied. At a 1-year
follow-up examination, the patient was recovering well, claiming to
experience a much better quality of life. The patient expressed no
intention to undergo reconstruction of the penis (Fig. 3). This study was approved by the
ethics committee of the Second Xiangya Hospital of Central South
University. Informed consent was obtained from the patient prior to
their contribution to this study.
Discussion
In cases of EEC in adult patients, careful screening
for malignant lesions in the affected areas is necessary. Notably,
the majority of untreated cases of EEC with bladder cancer have
been identified as adenocarcinoma or squamous cell carcinoma, which
are rare histological types of primary bladder cancer (5,6,7). The usual primary sites of these types
include the gastrointestinal system, breasts, prostate and ovaries
(5).
As in numerous other complicated conditions, it is
necessary for the treatment for adult EEC to be designed according
to the circumstances of the individual patient. In the present
case, the aims of the surgery included: i) Controlling the
malignant lesions; ii) improving the quality of life of the
patient; and iii) improving the patients cosmetic appearance.
Therefore, a radical cystectomy plus expanded local
lymphadenectomy was performed. In addition, an ileal conduit was
applied as the patient had no normal urethra.
The performance of an osteotomy in exstrophy
reconstruction is controversial. Proponents of the use of osteotomy
maintain that it facilitates easier approximation of the soft
tissues; the opponents are primarily concerned about the risk of
inadvertently causing future incontinence (8). To the best of our knowledge, the
present patient had the widest separation of the symphysis pubis
reported in the literature to date. Considering the width of the
gap and the rigidity of the pelvic bone, there was risk of an
osteotomy reducing the stability of the patients pelvis. Therefore,
an osteotomy was not performed. Instead, a metallic mesh was used
to restore the integrity of the pelvis and to help reconstruct the
lower abdomen wall. On the basis of multiple follow-up
examinations, the mesh appeared to function well for the patient.
At a 1-year follow-up examination, neither mesh distortion nor
other complications were detected.
Acknowledgements
The authors thank the anesthesiologists, nurses,
care-givers and hospital workers who facilitated the surgery.
References
|
1
|
Gearhart JP: The bladder
exstrophy-epispadias-cloacal exstrophy complex. Pediatric Urology.
Gearhart JP, Rink RC and Mouriquand PDE: (Philadelphia). Saunders.
511–546. 2001.
|
|
2
|
Grossfeld GD and Carroll PR: Evaluation of
asymptomatic microscopic hematuria. Urol Clin North Am. 25:661–676.
1998. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Smeulders N and Woodhouse CR: Neoplasia in
adult exstrophy patients. BJU Int. 87:623–628. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Gulati P, Yadav SP and Sharma U:
Management of bladder exstrophy in adulthood: Report of 2 cases. J
Urol. 157:947–948. 1997. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Di Lauro G, Iacono F, Ruffo A, Romis L,
Mordente S, Pane U, Illiano E, Romeo G, Prezioso D and Amato B:
Presenting a case of a mucinous adenocarcinoma of an exstrophic
bladder in an adult patient and a review of literature. BMC Surg.
13(Suppl 2): S362013. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Rieder JM, Parsons JK, Gearhart JP and
Schoenberg M: Primary squamous cell carcinoma in unreconstructed
exstrophic bladder. Urology. 67:1992006. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Paulhac P, Maisonnette F, Bourg S, Dumas
JP and Colombeau P: Adenocarcinoma in the exstrophic bladder.
Urology. 54:7441999. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Borer JG: Are osteotomies necessary for
bladder exstrophy closure? J Urol. 191:13–14. 2014. View Article : Google Scholar : PubMed/NCBI
|