Introduction
Although rare, metastatic choroid tumors are the
most common type of intraocular malignancy. The frequency of
intraocular metastasis in all patients dying of cancer was reported
to be approximately 12% (1). Lung
and breast cancers are two of the predominant tumors to metastasize
to the eye (2,3). Among the ocular metastases, the choroid
is the most commonly affected site (2). The prognosis for patients with ocular
metastases remains inadequate. For these patients life expectancy
is reported to be between 2–48 months (median 6–9 months)(4,5).
Radiotherapy remains the main type of therapy and allows the
majority of patients to maintain a good vision for as long as they
are alive (1). Recently, the
development of molecular targeted therapies, such as humanized
antivascular endothelial growth factor, bevacizumab and epidermal
growth factor receptor (EGFR)-tyrosine kinase inhibitors, has
improved the survival rate of patients with advanced non-small cell
lung cancer (NSCLC), without substantially increasing the toxicity
(6). The present study reports the
case of a patient with NSCLC and choroid metastasis who was
successfully treated with bevacizumab-containing chemotherapy,
following treatment failure with gefitinib.
Case report
A 69-year-old female that had been newly diagnosed
with a metastatic adenocarcinoma of the lung presented with a
one-month history of blurred vision in the left eye. The best
corrected visual activity (BCVA) in the left eye was 20/200. A
chest radiograph and computed tomography (CT) scan revealed a
pulmonary mass in the left upper lobe with ipsilateral mediastinal
lymph node swelling (Fig. 1). In
addition, pleural fluid was observed in the left lung, while
metastases were identified in both lungs, the paraaortic lymph
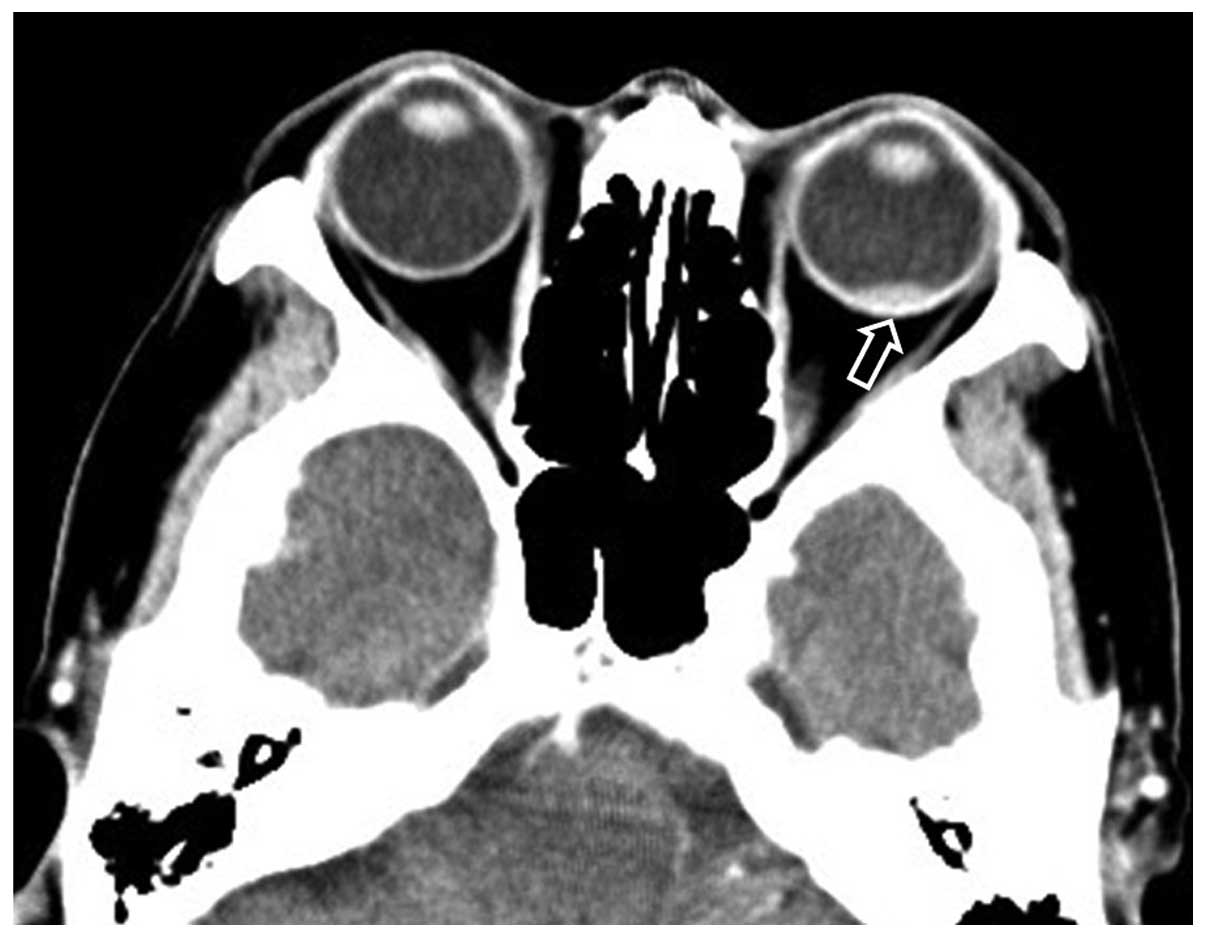
nodes of the abdomen and the right adrenal gland. A brain CT scan
revealed a choroidal tumor in the left eye that measured
10.4×6.4×2.6 mm in size (Fig. 2).
Pathological diagnosis of the lung mass, which was obtained via a
transbronchial biopsy, revealed an adenocarcinoma. Using the
specimen obtained from the primary lesion by bronchoscopy, an EGFR
mutation was evaluated using a PCR clamp method. The PCR clamp
method preferentially amplifies mutation sequences and detects
mutations. The method requires a peptide nucleic acid (PNA) clamp
primer and locked nucleic acid (LNA) probe. PNA clamp primers bind
to the wild type sequence and suppress their amplification, whereas
LNA probes are designed to specifically detect mutant sequences and
enhance their amplification in the presence of wild type sequences,
since PNA clamp primers competitively inhibit the ability of mutant
LNA probes to bind to wild type sequences. To detect mutations of
exons 18, 19, 20 and 21, a total of 12 probes were used. The PCR
clamp method was performed by Mitsubishi Kagaku Bio-Clinical
Laboratories, Inc. (Tokyo, Japan). As the patient had a mutation in
the EGFR gene (exon 21 L858R), treatment with gefitinib was
initiated. However, the BCVA of the left eye continued to
deteriorate to ‘mortus manus’ (finger movement) and the pleural
fluid in the left lung increased. Therefore, the response was
evaluated as a progressive disease. Subsequently, the patient
received chemotherapy with carboplatin (AUC 5, day 1, q28),
pemetrexed (500 mg/m2, day 1, q28) and bevacizumab (15
mg/mg, day 1, q28). A brain CT scan performed after two cycles of
the chemotherapy revealed the disappearance of the choroidal lesion
(Fig. 3). In addition, an
improvement in vision of up to 20/200 was observed. Subsequently,
the patient completed four cycles of the chemotherapy and attained
a partial response. The patient received additional maintenance
chemotherapy with pemetrexed (500 mg/m2, day 1, q28) and
bevacizumab (15 mg/mg, day 1, q28). The patient survived for 16
months after the diagnosis of lung adenocarcinoma, with no evidence
of deterioration of vision. Written informed patient consent was
obtained from the patient's family.
Discussion
Breast and lung cancers are the most common primary
tumors that metastasize to the eye and orbit (2,3,7), and the most commonly affected part of
the eye is the vascular uveal tract (7). Within the uvea, the choroid is the most
frequently affected site of metastasis (2). As observed in the patient in the
present study, the majority of patients have metastatic lesions
elsewhere at the time of diagnosis of ocular involvement (8). As a result of such metastasis, the
treatment for ocular metastasis may be palliative and the aims for
treatment are to maximize the quality of life and restore or
preserve vision.
Certain case reports have demonstrated that
chemotherapy is efficacious for choroid metastases from NSCLC
(9,10). To the best of our knowledge, there
have been seven case reports that precisely describe the outcome of
bevacizumab-containing chemotherapy for the treatment of choroid
metastasis (11–16). The characteristics of these studies
are outlined in Table I. In four
cases, the patient was diagnosed with adenocarcinoma. However, no
information was provided with regard to EGFR gene mutations in any
of the patients. In all the cases, improvement was observed in the
choroid metastasis, as well as functional improvement in visual
power. In four cases, including the present study, systemic
bevacizumab-containing chemotherapy was applied (one patient
received cisplatin-based therapy and three patients received
carboplatin-based chemotherapy) (11,14,16). Kim
et al reported successful treatment with oral erlotinib and
intravitreal therapy with bevacizumab (12). In the present case, gefitinib was not
effective for the intrathoracic and intraocular lesions, despite
the detection of a mutation in the EGFR gene. Lai et al
reported the successful treatment of a case with intravitreal
bevacizumab therapy, without administration of systemic
chemotherapy (15). Visual power in
this patient was shown to improve; however, the patient succumbed
four months after the diagnosis (15). By contrast, D'Antonio et al
presented a case who was successfully treated with systemic
bevacizumab-containing chemotherapy and survived for over 20 months
(14). In the present study, the
patient survived for 16 months following the diagnosis of lung
cancer. However, the prognosis of choroid metastasis from lung
cancer is very poor, with a mean life expectancy of 1.9 months
(4). This short survival time is not
due to the choroid metastasis itself, but the condition of disease
dissemination with the involvement of other vital organs. The four
patients treated with bevacizumab and the current patient had
metastatic sites other than in the choroid. Singh et al
reported two cases treated with bevacizumab-containing
chemotherapy. In one of these patients, first line chemotherapy
without bevacizumab was not effective for the choroid metastasis;
however, second line chemotherapy with bevacizumab-containing
chemotherapy achieved resolution of the choroid metastasis and
visual improvement (16). Notably,
the patient in the present study received bevacizumab-containing
chemotherapy as the second line treatment and also achieved
resolution of the choroid metastasis and visual improvement. These
results suggested that systemic chemotherapy with bevacizumab may
have an significant role in improving visual power as well as
survival of the patients.
 | Table I.Patients treated with bevacizumab. |
Table I.
Patients treated with bevacizumab.
| Age gender | Symptom | Duration of
symptoms | Pretreatment visual
power | Affected eye | Lung cancer | EGFR mutation | Other metastatic
sites | Size of choroid
metastasis (mm) | Intravitreal BEV | Systemic
chemotherapy | Improvement of
choroid metastasis | Visual power after
therapy | Systemic effect | Toxicity | Survival
(months) | First author,
year |
|---|
| 42 F | Blurred vision | 1 week | nd | Right | LA | nd | Lung, cervical
LN | 12×12×6.3 | No | CBDCA+GEM+BEV | Complete
resolution | Improved | PR | None | Alive | George, 2009 |
| 57 F | Decreased vision | 3 month | BCVA 20/200 | Left | AD | nd | Multiple
metastases | 8.37×7.56×2.48,
7.52×6.21×2.94 | Yes | Erlotinib | Completely
disappeared | Improved to
20/40 | nd | None | nd | Kim, 2009 |
| 53 M | Decreased vision | 1 month | 20/50 | Left | AD | nd | Lungs | nd | Yes | TS-1 | 20/100 | Improved to
20/25 | nd | None | 5 | Inagaki, 2011 |
| 34 F | Vision loss,
diplopia | nd | nd | Left | AD | nd | nd | Big (size, nd) | Yes | CDDP+GEM BEN | Dimensional
reduction | Complete
recovery | SD | None | 20 (alive) | D'Antonio, 2012 |
| 73 M | Decreased vision | nd | BCVA 20/200 | Left | AD | nd | Stage IV (nd) | nd | Yes | Not done | Regression of tumor
size | Improved to
20/60 | nd | None | 4 | Lai, 2012 |
| 42 F | Diminished
vision | 1.5 month | 2/60 | Left | NSCLC | nd | Liver | 14.8×13.0×4.1 | Yes | CDDP+PAC | Complete
resolution | Improved to
6/120 | nd | None | 9 | Singh, 2012 |
| 53 M | Loss of vision | 3 month | Mortus Manus | Right | NSCLC | nd | Liver, bone, adrenal
gland | 15.0×14.5×6.3 | Yes | CBDCA+DOC+BEV | Decreased | Improved to 6/24 | nd | None | 16 | Singh, 2012 |
| 69 F | Blurred vision | 1 month | Mortus Manus | Left | AD | Exon 21, L858R | Lung, abdominal LN,
adrenal | 10.4×6.4×2.6 | No | CBDCA+PEM+BEV | Completely
disappeared | Improved to
20/100 | PR | None | 16 | Present case |
Intravitreal bevacizumab administration has been
used to treat choroid metastases from organs other than the lungs
(17,18). In these two studies, antiangiogenic
and antipermeability effects of bevacizumab were observed on the
new tumor vessels by fluorescein angiography. These observations
demonstrate the obligate and vital dependence of choroidal tumors
on angiogenesis, which forms the rationale for the use of
intravitreal bevacizumab administration, regardless of the fact
that a platinum doublet in combination with bevacizumab is one of
the chemotherapy options for the treatment of lung cancer patients
with choroid metastasis. Two of the patients who were treated with
systemic bevacizumab-containing chemotherapy received intraviteral
administration of bevacizumab (14,16)
(Table I).
In conclusion, the present case report demonstrated
the efficacy and safety of systemic bevacizumab therapy in
combination with a platinum doublet for the treatment of choroid
metastasis, with resulting morphological and functional
improvements in the choroidal metastatic tumor. Therefore, systemic
administration of bevacizumab with intravitreal injections may be
selected as a therapeutic approach due to the greater potential to
produce effective chemotherapeutic concentrations around the
metastasis site via the rich choroidal blood supply, which is
within the systemic circulation and not protected by the
blood-retina barrier.
References
|
1
|
Small W Jr: Management of ocular
metastasis. Cancer Control. 5:326–332. 1998.PubMed/NCBI
|
|
2
|
Shields CL, Shields JA, Gross NE, Schwartz
GP and Lally SE: Survey of 520 eyes with uveal metastases.
Ophthalmology. 104:1265–1276. 1997. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Soysal HG: Metastatic tumors of the uvea
in 38 eyes. Can J Ophthalmol. 42:832–835. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Kreusel KM, Wiegel T, Stange M, Bornfeld
N, Hinkelbein W and Foerster MH: Choroidal metastasis in
disseminated lung cancer: frequency and risk factors. Am J
Ophthalmol. 134:445–447. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Tsina EK, Lane AM, Zacks DN, Munzenrider
JE, Collier JM and Gragoudas ES: Treatment of metastatic tumors of
the choroid with proton beam irradiation. Ophthalmology.
112:337–343. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Bunn PA Jr and Thatcher N: Systemic
treatment for advanced (stage IIIb/IV) non-small cell lung cancer:
more treatment options; more things to consider. Conclusion.
Oncologist. 13(Suppl 1): 37–46. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Freedman MI and Folk JC: Metastatic tumors
to the eye and orbit. Patient survival and clinical
characteristics. Arch Ophthalmol. 105:1215–1219. 1987. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Kanthan GL, Jayamohan J, Yip D and Conway
RM: Management of metastatic carcinoma of the uveal tract: an
evidence-based analysis. Clin Experiment Ophthalmol. 35:553–565.
2007. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Battikh MH, Ben Yahia S, Ben Sayah MM, et
al: Choroid metastases revealing pulmonary adenocarcinoma resolved
with chemotherapy. Rev Pneumol Clin. 60:353–356. 2004.(In French).
View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Shields JA, Perez N, Shields CL, Foxman S
and Foxman B: Simultaneous choroidal and brain metastasis as
initial manifestations of lung cancer. Ophthalmic Surg Lasers.
33:323–325. 2002.PubMed/NCBI
|
|
11
|
George B, Wirostko WJ, Connor TB and
Choong NW: Complete and durable response of choroid metastasis from
non-small cell lung cancer with systemic bevacizumab and
chemotherapy. J Thorac Oncol. 4:661–662. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Kim SW, Kim MJ, Huh K and Oh J: Complete
regression of choroidal metastasis secondary to non-small-cell lung
cancer with intravitreal bevacizumab and oral erlotinib combination
therapy. Ophthalmologica. 223:411–413. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Inagaki E, Shinoda H, Uchida A, et al:
Effect of intravitreal injection of bevacizumab for exudative
retinal detachment secondary to metastatic choroidal tumor: Case
report. Atarashii Ganka. 28:587–592. 2011.(In Japanese).
|
|
14
|
D'Antonio C, Viterbo A, Romiti A, Enrici
MM, Lauro S and Marchetti P: Complete regression of a non-small
cell lung cancer choroidal metastasis with intravitreal
bevacizumab. J Thorac Oncol. 7:468–469. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Lai CL, Fan KS, Lee YH, Chen HC and Fan
WH: Intravitreal administration of bevacizumab in the treatment of
choroidal metastasis in a patient with erlotinib-failed pulmonary
adenocarcinoma. Lung Cancer. 76:496–498. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Singh N, Kulkarni P, Aggarwal AN, et al:
Choroidal metastasis as a presenting manifestation of lung cancer.
A report of 3 cases and systematic review of the literature.
Medicine (Baltimore). 91:179–194. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Amselem L, Cervera E, Díaz-Llopis M, et
al: Intravitreal bevacizumab (Avastin) for choroidal metastasis
secondary to breast carcinoma: Short-term follow-up. Eye (Lond).
21:566–567. 2007.PubMed/NCBI
|
|
18
|
Kuo IC, Haller JA, Maffrand R, Sambuelli
RH and Reviglio VE: Regression of a subfoveal choroidal metastasis
of colorectal carcinoma after intravitreous bevacizumab treatment.
Arch Ophthalmol. 126:1311–1313. 2008. View Article : Google Scholar : PubMed/NCBI
|