Introduction
Breast tuberculosis (BTB) is a rare type of
extrapulmonary tuberculosis (TB). A BTB case was first described by
Sir Astley Cooper in 1829 as a scrofulous swelling of the breast.
Mammary gland tissues, skeletal muscles and the spleen are
resistant to the multiplication and survival of the tubercle
bacillus. It has been reported that the uncommon occurrence of
BTB may be due to this feature (1).
BTB commonly affects females of a reproductive age (range, 20–40
years), whereas it is rare in prepubescent females, elderly women
and males. BTB lesions can mimic carcinoma in elderly patients,
while it may be misdiagnosed as a pyogenic breast abscess in young
patients. Thus, establishing an accurate diagnosis of BTB is often
challenging. Breast tuberculosis has no specific clinical features
and has been termed as a ‘great masquerader’ as a result of its
different presentation. The history of the presenting symptoms in
BTB is typically less than a year; however, it varies from a few
months to several years (2). A lump
in the central or upper outer quadrant of the breast is the most
common form of presentation. Upon physical examination, common
symptoms include a mass, tenderness, pain, swelling or fluctuation
in abscess formation in the breast, presenting with or without
discharging sinuses (2,3).
Radiological imaging is not diagnostic. Diagnosis is
based on the identification of typical histological features or the
tubercle bacilli under microscopy or culture (2–4).
However, smear positivity for acid-fast bacilli by Ziehl-Neelsen
staining is low, and in the majority of cases, the diagnosis can
only be accurately diagnosed by histological identification of the
typical necrotizing granulomatous lesion (5). It has been reported that, in endemic
countries, the incidence is 3.0–4.5% of all breast lesions
(6). BTB constitutes <1% of all
diseases of the breast in developed countries. However, the
incidence of the disease is higher in countries endemic for TB,
such as the Indian subcontinent, where BTB may comprise up to 4.0%
of breast diseases (4,7). In addition, tuberculosis constitutes
0.025–0.1% of all surgically treated diseases of the breast
(8). The treatment of breast
tuberculosis consists of anti-tubercular chemotherapy and surgery
with specific indications (2).
In the present study, a retrospective analysis of 7
BTB cases was conducted, with the aim to evaluate the
characteristics of this disease. The aims of the present study was
to evaluate the clinical features, demographic data, diagnostic
methods, therapeutic regimens and duration of therapy in BTB
cases.
Materials and methods
Cases
The medical files of BTB cases among TB patients
registered and treated at the Ankara Tuberculosis Control
Dispensary No. 7 (Ankara, Turkey) between January 2006 and December
2013 were retrospectively evaluated. The information gathered from
the medical documents included the age, gender, occupation, marital
status, gestation, lactation, number of children (as well as gender
and child age upon admission of the patient), TB family contact
history, symptoms, diagnostic duration, diagnostic methods, BCG
vaccine scar, tuberculin skin test (TST) results, pathological
results, chest X-ray scans, anti-TB treatment duration and
existence of a TB type other than BTB. The cases were divided as
PTB, NPTB and PTB plus NPTB cases. This retrospective study was
approved by the Department of Tuberculosis Control at the Ministry
of Health, No. 63519166/620/2840 (Ankara, Turkey).
X-ray, computed tomography and
ultrasonography
The results of chest X-ray, computed tomography and
ultrasonography were used for radiological investigation were
obtained from patients files.
Histopathological examination
Histopathological analysis data was retrospectively
analyzed. The samples were obtained by fine-needle aspiration in 2
cases, excisional biopsy in 2 cases, incisional biopsy in 1 case,
tru-cut biopsy in 1 case and surgical resection in 1 case for
histopathological examination. Both smear with Ziehl-Neelsen
staining and Lowenstein Jensen culture were performed for a
microbiological diagnosis.
TB treatment regimen
TB treatment was administered according to the
Turkish national guidelines TB treatment consisted of 2 months of
HRZE plus 4 to 7 months of HR (H, isoniazid, R, rifampin, E,
ethambutol and Z, pyrazinamide). The duration and drugs may have
been adapted according to the advice of a physician.
Results
TB cases
A total of 648 cases diagnosed TB were identified
during 2006–2013. Among them, there were 296 cases (50%) of
pulmonary TB (PTB), 278 cases (43%) of non-pulmonary TB (NPTB) and
45 cases (7%) PTB plus NPTB cases. In total, 7 of the NPTB cases
involved the breast, constituting 1.08% (7/648) of all TB cases and
2.51% (7/278) of all NPTB. All the identified BTB patients were
newly-diagnosed cases, with a time from symptom to definite
diagnosis between 2 and 6 months.
Patient characteristics
The demographic and clinical features of study group
are shown in Table I. The mean age
of BTB patients was 34±9.46 years (age range, 24–53 years).
Unilateral breast involvement was observed in 6/7 cases, including
involvement of the right breast in 3 cases, and of the left breast
in another 3 cases). In addition, 1 case presented bilateral breast
involvement. All the included BTB cases had one or two children,
with the exception of 1 case that did not have any children. There
were no pregnant or lactating women within the included cases. All
cases had a scar from the BCG TB vaccine, while a TST test
indicated a mean size of induration of 14.28±6.79 mm (size range,
7–26 mm). One patient had family history of contact with TB.
 | Table I.Demographic and clinical features of
study group. |
Table I.
Demographic and clinical features of
study group.
| Patient no. | Date | Age
(years)/gender | Contact with TB | TST size, mm | Number of children
(age/gender) | Characteristics and
symptoms | Diagnosis method | Histopathological
results | Treatment duration,
monthsa |
|---|
| 1 | 2006 | 53/F | Yes | 12 | 0 | 4×3×3-cm painful
swelling in the upper-inner quarter of the right breast at right
parasternal border | Fine-needle
aspiration biopsy | Granulomatous
inflammation with typical caseous necrosis, positive AFB smear | 9 |
| 2 | 2009 | 30/F | No | 20 | 2 (8/M, 13/F) | 6×10-mm discharging
sinus in the upper outer quadrant of right breast; 8×11.mm solid
mass in the left breast | Fine-needle
aspiration biopsy | Granulomatous
inflammation, negative AFB smears | 9 |
| 3 | 2010 | 38/F | No | 26 | 2 (8/M, 6/M) | Discharging sinus
invading the pectoral muscle and rib in the lower outer quadrant of
the right breast | Excisional
biopsy | Granulomatous
inflammation; positive AFB DNA | 9 |
| 4 | 2012 | 34/F | No | 7 | 2 (15/M, 7/M) | Firm and tender
breast; painful swelling and erythema of the breast skin; acne-like
lesion in border of the left nipple | Incisional
biopsy | Non-caseous necrosis,
inflammation; positive AFB smear | 6 |
| 5 | 2012 | 24/F | No | 9 | 2 (5/F, 2/M) | Two solid masses in
the upper outer quadrant of the left breast | Left segmental
mastectomy + total excision | Non-caseous necrosis,
inflammation | 6 |
| 6 | 2013 | 31/F | No | 16 | 2 (14/M, 5/M) | 2×3-cm lump with
fluctuation border areola of the right breast | True-cut biopsy +
total excision (lumpectomy) | Granulomatous
inflammation | 9 |
| 7 | 2013 | 28/F | No | 10 | 1 (4/F) | Painful swelling,
discharging sinus in the left breast | Excisional
biopsy | Mastitis and fat
necrosis; negative, AFB smears | 6 |
Common symptoms
The commonly observed symptoms among the BTB
patients included presence of a mass, tenderness, pain, swelling
and fluctuation in abscess formation in the breast, which presented
with or without discharging sinuses. Nipple retraction or discharge
were not observed in any of the included BTB patients. In addition,
no respiratory symptoms were observed.
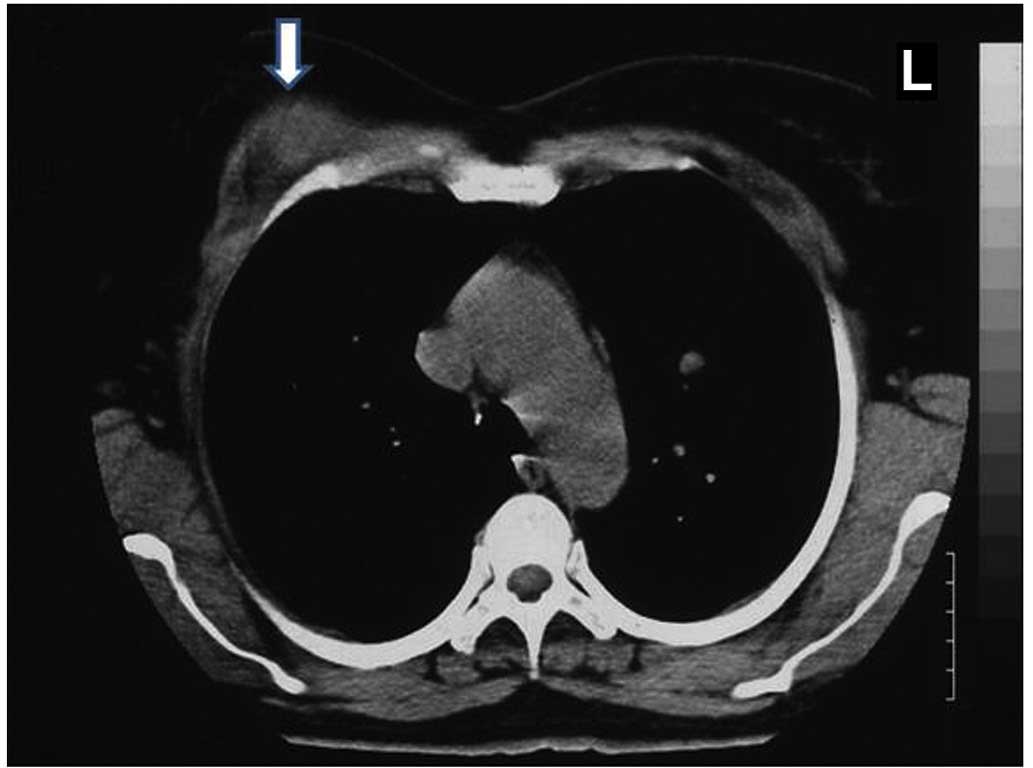
Examinations and diagnosis
Chest X-ray scans were normal in all the included
BTB cases. The diagnostic methods included mammography,
ultrasonography, thorax computed tomography (CT), fine needle
aspiration cytology (FNAC), staining for acid-fast bacilli (AFB) in
smear and culture tests, excisional or incisional biopsy, and
excision (including mastectomy or lumpectomy). Representative
examples of CT and ultrasonic examinations performed for the
diagnosis of BTB are shown in Figs.
1 and 2, respectively. AFB
testing was positive in 2/7 cases.
Histopathological examination
Upon histopathological examination of tissue
samples, the following characteristics were observed: Granulomatous
inflammation was observed in 3 cases; granulomatous inflammation
with typical caseous necrosis was detected in 1 case; non-caseous
necrosis inflammation was detected in 2 cases; and mastitis and fat
necrosis inflammation was observed in 1 case.
Treatments
All cases were successfully treated with anti-TB
drugs. The TB treatment consisted of 2 months of isoniazid +
rifampin + ethambutol + pyrazinamide (HRZE regimen), followed by
4–7 months of isoniazid + rifampin (HR regimen). Recurrence was not
observed in any of the cases.
Representative BTB case
In the case presenting with mastitis and fat
necrosis inflammation (case no. 7, Table
I), right mastitis was developed while the patient was
lactating 4 years prior to TBT diagnosis. The disease improved
following nonspecific antibiotherapy; however, mastitis was again
developed (1 year later), which was not resolved after further
nonspecific antibiotherapy. Subsequent to biopsy and further
investigation, the patient was diagnosed with TB and received
anti-TB drugs, which resulted in successful treatment. The patient
in this case received 6 months anti TB drugs (2 months of HRZE plus
4 months of HR) (H: 300 mgr, R: 600 mgr, Z: 2,000 mgr, E: 1,500
mgr) This case has been reported in further detail as an exact
diagnosis was not established
Discussion
BTB is a rare form of extrapulmonary TB that is
associated with risk factors including past history of suppurative
mastitis, trauma, lactation, multiparity and acquired immune
deficiency syndrome. Lactation has been demonstrated to increase
the susceptibility of the breast to TB. During lactation, the
increased vascularity of the breast may facilitate infection and
dissemination of the bacilli. However, there were no pregnant or
lactating women in the patient cohort of the present study. The
majority of cases had an age between 20 and 40 years. It has been
previously shown that unilateral involvement is common in BTB. In
the current study, unilateral involvement was observed in 6/7
cases, which is consistent with previous reports.
BTB commonly presents with the following clinical
characteristics: Ill-defined, solitary, unilateral solid lump
located in central or upper outer quadrant of the breast. The mass
may be solid, irregular and occasionally fixed to the muscle, skin
or chest wall. Bilateral involvement and presence of multiple lumps
are rarely reported (in <3% of cases) (9). In the cases reported in the current
study, the symptoms included presence of a mass, tenderness, pain,
swelling and fluctuation in abscess formation in the breast, with
or without discharging sinuses, while the lesions were generally
located in the upper outer quadrant of the breast.
The main routes through which TB lesions spread and
the breast may become infected with TB bacilli includes by
haeamatogenous routes, lymphatic extension from primary foci of
disease in the lymph nodes of the mediastinum, axilla and
parasternal and cervical regions, direct inoculation and by ductal
infection (10) The disease presents
in two forms, primary and secondary BTB. Primary BTB is rarely
reported, and the breast is the only affected area in this form of
the disease. By contrast, secondary BTB is more frequently
reported, and a prior history of TB is common in these cases
(4,7,9). In the
present study, the only organ involved was the breast, and thus all
cases presented primary BTB.
No specific features of BTB are observed in
mammography and ultrasonography examinations. Mammography can be
used to identify the three different patterns of TB, which include
the nodular, disseminated and sclerosing lesions. The nodular
pattern is indicated by the presence of slow-growing, painless and
well-circumscribed lesions. At an advanced stage, retraction and
sinus formation may be observed through involvement of the skin. In
addition, the disseminated pattern presents as interconnected focal
lesions, sinus formation and skin thickening. Finally, the
sclerosing pattern commonly occurs in older females and presents as
slow-growing, dense fibrous tissue. Generally, no
microcalcification or nipple retraction are observed. According to
radiological findings, the nodular pattern may be misdiagnosed as
fibroadenoma. Thorax computed tomography is important for
evaluating chest wall, musculoskeletal and other involvement, and
can also be used as a guide for obtaining tissue samples for
diagnosis (4).
A suspicion of BTB is essential for diagnosis. The
gold standard for diagnosis of BTB is the detection of the
etiologic agent using Ziehl-Neelsen staining or culturing; however,
AFB test is rarely positive. Histopathological examination, FNAC,
true-cut biopsy or open biopsy are also important for diagnosis,
with FNAC being the most widely used initial invasive diagnostic
method. In order to establish a diagnosis, the present study, FNAC
was used in 2 cases, excisional biopsy in a another 2 case,
incisional biopsy in 1 case and total excision in 2 cases.
Granulomas may be detected anywhere in breast tissue and granuloma
is often composed of histiocytes, Langhans giant cells,
lymphocytes, rare plasma cell and eosinophilic caseous necrosis. In
the case with mastitis and fat necrosis inflammation presented in
the current study, no improvement was observed following
nonspecific antibiotherapy and the patient was then successfully
treated with anti-TB drugs. In past years, mastectomy was the
common treatment of BTB; however, in recent years, the success of
antituberculous drug therapy is high and surgical intervention is
rare (10–12).
Tanrikulu et al (13) reported 27 BTB cases between 2004 and
2008, with all cases being newly-diagnosed patients with a mean age
of 31.5±8.4 years. The study reported that cases presented with
breast swelling (48.1%), mass and fluctuation in abscess formation
(40.7% each) and painful breasts (18.5%) (13). Of the included patients, 1 case had
previous TB lymphadenitis in the cervical region, while the
remaining cases had no history of TB; thus, 26/27 cases were
diagnosed with primary BTB, and ~73.0% of cases were diagnosed
using FNAC (13). In addition, Kalaç
et al (8) presented 5 BTB
cases with a mean age between 20 and 63 years. All the reported
cases had children and were breast-feeding, while all lesions were
found to be unilateral and AFB testing revealed negative results.
One of the cases had received anti-TB treatment for pulmonary TB 10
years earlier (8). Diagnosis was
established histopathologically from the excisional biopsy
material. Caseating granulomatosis was also identified in the
axillary lymph nodes of 3 patients (8). Furthermore, Khanna et al
(14) reported 52 cases of BTB
within a 15-year period, which accounted for 3% of all breast
lesions reported at their hospital. The authors reported presence
of a breast mass with associated sinus in 39% of cases, isolated
breast lump in 23% of cases, sinus with absence of a lump in 12% of
cases and tender nodules in 23% of cases, with associated axillary
lymphadenopathy reported in 41% of cases. The BTB diagnosis was
confirmed using FNAC or histological examination in all the
patients, and the main treatment administered was anti-TB therapy
(14). Another study by Al-Marri
et al (6) reported 13
multiparous women with BTB within a 10-year period, who were
diagnosed based on histological examination. All patients presented
with a mass, while 2 patients had symptoms of nipple discharge and
1 presented a palpable axillary node on the same side (6). Ben Hassouna et al (15) reported 65 BTB cases, which
represented 0.2% of the tubercular localizations and 0.3% of the
breast pathologies reported at their clinic within the investigated
time period. The initial suspected diagnosis was malignant tumor in
60% of the BTB cases, benign nodule in 24.6% of patients and
presence of an abscess in 16.4% of patients (15). Based on mammography examination, a
malignant lesion was suspected in 49% of cases, while FNAC was
performed in 8 patients, showing a negative result in 6 of these
(15). Eventually, the BTB diagnosis
was established using histological examination following
identification of typical TB lesions on tumorectomy or biopsy
samples, and all patients received anti-TB treatment (15). A study by Harris et al
(16) evaluated 38 patients with BTB
reported over a 5-year period, with a mean age of 29 years. Of
these, 10 patients (26%) experienced breast pain with or without
increased breast nodularity, while 14 patients (36%) presented
axillary lymph node involvement (16). Associated pulmonary TB was only
identified in 5/38 patients, with the remaining presenting isolated
involvement of the breast (16).
Patients were mainly treated with anti-TB drugs for 6–9 months
(16).
In an earlier study by Sharma et al (17), 7 females with BTB were diagnosed
between 1980–1988, with an age range of 17–50 years. The clinical
features included lumps, ulcers, multiple discharging sinuses and
recurring abscess of the breast. Diagnosis was established based on
histological examination results, while AFB positivity was found in
only 1 samples and positive culture in 1 other patient. Patients
received anti-TB treatment along with removal of the infected
breast tissue (17). Fukuoka et
al (18) reported 12 BTB cases
within a 10-year period, with a mean age of 42.8 years (range,
28–84 years). Only 1 case had past history of TB contact and in the
remaining cases TB of the breast was considered to be a primary
disease. Axillary lymph node involvement and formation of pyogenic
breast abscess occurred in 7 cases. The histological findings
revealed epithelioid cell granulomas with caseous necrosis in 11/12
cases, and 7/11 cases were treated with a combination of surgery
and anti-TB chemotherapy (18).
Furthermore, Morsad et al (19) treated 14 BTB cases at their hospital
over a 16-year period, with patient ages of 16–65 years. Contact
with TB was reported in 2 cases, and axillary nodes were observed
in 10 cases. The diagnosis of BTB was based on pathological
findings in 14 cases (including 2 biopsies and 12 perioperative
specimens) and isolation of bacilli from pus in 1 case. Medical
treatment was provided, as well as surgery when required, for
abscess drainage or treatment of residual lesions (19).
In conclusion, BTB is a rare form of TB and the
present retrospective study reported 7 cases of BTB along with the
results of histopathological examination, microbiological
examination and treatment. TB must be considered when there is
presence of breast masses presenting with tenderness, pain,
swelling and fluctuation in abscess formation, with or without
discharging sinuses.
References
|
1
|
Banerjee SN, Ananthakrishnan N, Mehta RB
and Parkash S: Tuberculous mastitis: A continuing problem. World J
Surg. 11:105–109. 1987. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Tewari M and Shukla HS: Breast
tuberculosis: Diagnosis, clinical features & management. Indian
J Med Res. 122:103–110. 2005.PubMed/NCBI
|
|
3
|
Baharoon S: Tuberculosis of breast. Ann
Thorac Med. 3:110–114. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
da Silva BB, Dos Santos LG, Costa PV,
Pires CG and Borges AS: Primary tuberculosis of the breast
mimicking carcinoma. Am J Trop Med Hyg. 73:975–976. 2005.PubMed/NCBI
|
|
5
|
Kakkar S, Kapila K, Singh MK and Verma K:
Tuberculosis of the breast: A cytomorphologic study. Acta Cytol.
44:292–296. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Al-Marri MR, Almosleh A and Almoslmani Y:
Primary tuberculosis of the breast in Qatar: Ten year experience
and review of the literature. Eur J Surg. 166:687–690. 2000.
View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Gon S, Bhattacharyya A, Majumdar B and
Kundu S: Tubercular mastitis-a great masquerader. Turk Patoloji
Derg. 29:61–63. 2013.PubMed/NCBI
|
|
8
|
Kalaç N, Ozkan B, Bayiz H, Dursun AB and
Demirağ F: Breast tuberculosis. Breast. 11:346–349. 2002.
View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Kervancıoğlu S, Kervancıoğlu R, Özkur A
and Sirikçi A: Primary tuberculosis of the breast. Diagn Interv
Radiol. 11:210–212. 2005.PubMed/NCBI
|
|
10
|
Marinopoulos S, Lourantou D, Gatzionis T,
Dimitrakakis C, Papaspyrou I and Antsaklis A: Breast tuberculosis.
Diagnosis, management and treatment. Int J Surg Case Rep.
3:548–550. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Afridi SP, Memon A, Rehman SU, Memon A and
Baig N: Spectrum of breast tuberculosis. J Coll Physicians Surg
Pak. 19:158–161. 2009.PubMed/NCBI
|
|
12
|
Sen M, Gorpelioglu C and Bozer M: Isolated
primary breast tuberculosis: Report of three cases and review of
the literature. Clinics (Sao Paulo). 64:607–610. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Tanrikulu AC, Abakay A, Abakay O and Kapan
M: Breast tuberculosis in southeast turkey: Report of 27 cases.
Breast Care (Basel). 5:154–157. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Khanna R, Prasanna GV, Gupta P, Kumar M,
Khanna S and Khanna AK: Mammary tuberculosis: Report on 52 cases.
Postgrad Med J. 78:422–424. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Ben Hassouna J, Gamoudi A, Bouzaiene H,
Dhiab T, Khomsi F, Chargui R, Sifi H, Mtaallah M, Makhlouf R,
Chebbi A, et al: Mammary tuberculosis: A retrospective study of 65
cases. Gynecol Obstet Fertil. 33:870–876. 2005.(In French).
View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Harris SH, Khan MA, Khan R, Haque F, Syed
A and Ansari MM: Mammary tuberculosıs: Analysis of thirty-eight
patients. ANZ J Surg. 76:234–237. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Sharma PK, Babel AL and Yadav SS:
Tuberculosis of breast (study of 7 cases). J Postgrad Med. 3724–26.
(26A)1991.PubMed/NCBI
|
|
18
|
Fukuoka K, Choh S, Hamada K, Yoneda T and
Narita N: A case of tuberculosis of the breast-review of the
literature published during the last 10 years in Japan. Kekkaku.
70:111–115. 1995.(In Japanese). PubMed/NCBI
|
|
19
|
Morsad F, Ghazli M, Boumzgou K, Abbassi H,
El Kerroumi M, Matar N, Belabidia B, Aderdour M and El Mansouri A:
Mammary tuberculosis: A series of 14 cases. J Gynecol Obstet Biol
Reprod (Paris). 30:331–337. 2001.PubMed/NCBI
|