Introduction
Lung cancer is a threat to people's health and life,
and according to the pathological features it may be divided into
small cell lung cancer and non-small cell lung cancer (NSCLC).
NSCLC accounts for ~80% of all lung cancer cases (1). Adenocarcinoma is the most common
pathological type of NSCLC (1).
Although surgery, comprehensive treatment and postoperative
chemotherapy have been applied to treat lung cancer, the 5-year
survival rate of lung cancer is only 10–15% (2,3).
Kruppel-like factor 8 (KLF8) is a member of the KLF
family and has various roles in the regulation of the cell cycle,
apoptosis, proliferation, differentiation, development and
carcinogenesis (4–6). Previous studies have demonstrated that
KLF8 is identified in various types of cancer to a large extent,
including gastric, lung, ovarian, breast and renal cancer (7–9). KLF8
may also affect the invasion and metastasis of tumors (10). However, no data is currently
available on KLF8 in lung adenocarcinoma (LAC).
Ki67 is a nuclear protein that is associated with
cellular proliferation (11). Ki67
protein is present during all active phases of the cell cycle (G1,
S, G2 and mitosis) (11). Ki67 has a
short life span, thus it is absent in resting cell phases (G0)
(12). Ki67 has been widely used as
a cell proliferation marker to determine the degree of growth,
invasion and prognosis of cancer (13).
The present study aimed to investigate the
expression of KLF8 in LAC, the association between KLF8 and
clinical features, and the expression of Ki67 in patients with LAC.
The relationship between KLF8 and patient survival was also
investigated in Kaplan-Meier survival curves.
Materials and methods
LAC tissues were collected from 140 patients who
underwent surgical resection without preoperative systemic
chemotherapy or radiotherapy at the Affiliated Hospital of Nantong
University (Nantong, China) between January 2009 and December 2010.
LAC tissues were obtained by surgery using protocols approved by
the Ethics Committee of the Affiliated Hospital of Nantong
University. Written informed consent was provided by all patients
enrolled in the study. Among the cases, there were 72 male and 68
female patients. These patients were aged between 39–77 years, and
the mean age was 61 years. All samples were fixed in 10% buffered
formalin for 24 h, which was performed at 20°C and embedded in
paraffin at the time of collection. All 140 patients with LAC had
corresponding history data and follow-up records.
Tumor tissues of these 140 specimens and
corresponding tumor-adjacent tissues were used for construction of
tissue microarrays (TMA). Briefly, each patient's tumor was
represented by 2.0-mm cores. Hematoxylin and eosin-stained slides
(4-µm thick) for each patient were histologically analysed using an
Olympus BX41 microscope (magnification, ×200; Olympus Corporation,
Tokyo, Japan) according to the the Union for International Cancer
Control (UICC) TNM staging system predominantly for the scope of
the primary tumor, regional lymph node metastasis and distant
metastasis stage.
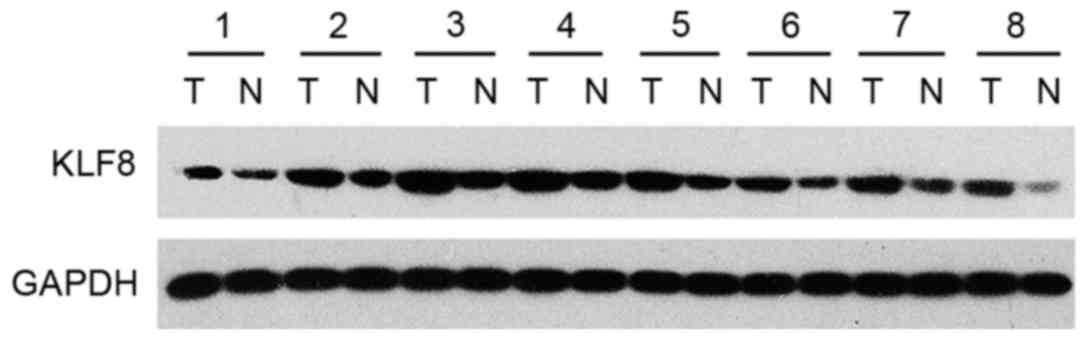
Another 8 samples of tumor tissues and adjacent
non-tumor tissue were collected for western blot analysis. These
samples were collected from 8 cases of patients who underwent
curative resection between January 2009 and December 2010 of LAC
tissues in the same hospital. Fresh samples were frozen in liquid
nitrogen immediately after surgical removal and maintained at −80°C
until they were used for western blot analysis.
Western blot analysis
Protein was extracted from ~0.1 g of fresh tissue
from the 8 cases of tumor and matched adjacent normal samples.
Tissues were immediately homogenized in a homogenization buffer
containing 50 mM Tris-HCl (pH 7.5), 150 mM NaCl, 0.1% NP-40, 5 mM
EDTA, 60 mM β-glycerophosphate, 0.1 mM sodium orthovanadate, 0.1 mM
NaF and complete protease inhibitor cocktail (Roche Diagnostics,
Basel, Switzerland), and then centrifuged at 12,000 × g for 30 min
to collect the supernatant (4°C). The bicinchoninic acid assay
method was used to determine the protein concentration in the
samples after the addition of SDS buffer and 100°C for 10 min.
Following this, protein samples (60 µg) were separated with 12%
SDS-PAGE and transferred to polyvinylidene fluoride membranes. The
membranes were blocked with Tris-buffered saline with Tween-20
(TBST) supplemented with 5% skimmed milk for 1 h and then incubated
with rabbit anti-human KLF8 antibody (1:150; ARP31533 P050; Aviva
Systems Biology Corp., San Diego, CA, USA) or mouse anti-human
GAPDH antibody (1:150; OAAD00231; Aviva Systems Biology Corp)
overnight at 4°C. Membranes were washed three times with TBST and
incubated with goat anti-rabbit IgG-HRP (1:8,000; sc-2004) and goat
anti-mouse IgG-HRP (1:5,000; sc-2005; both from Santa Cruz
Biotechnology, Inc., Santa Cruz, USA) secondary antibodies for 2 h
at room temperature. Enhanced chemiluminescence reagents (Thermo
Fisher Scientific, Inc.) were used for band detection using a Tanon
5200 Imaging System (Tanon Science Technology Co., Shanghai,
China). The band intensity was measured using the ImageJ 1.40
analysis system (National Institutes of Health, Bethesda, MD,
USA).
Immunohistochemistry
The EnVision method (14) was used for immunohistochemical
staining. A total of 140 LAC samples were produced for TMA. The
samples were incubated for 40 min at 70°C, dewaxed and dehydrated
in graded ethanol. Using TMA in antigen repairing 22 min at 99°C,
dripping with 3% hydrogen peroxide for 20 min at room temperature.
Then the samples were washed with phosphate-buffered saline with
Triton X-100 three times, and incubated with rabbit anti-human KLF8
antibody (1:150; Aviva Systems Biology Corp.) or rabbit anti-human
Ki67 (1:500; ab15580; Abcam, Cambridge, UK) overnight at 4°C.
Subsequently, the samples were incubated with goat anti-rabbit
IgG-HRP antibody (1:500; sc-2004; Santa Cruz Biotechnology, Inc.)
for 2 h at room temperature. PBS was used as a negative control
instead of the primary antibody. The Olympus BX41microscope was
used to capture images of the samples.
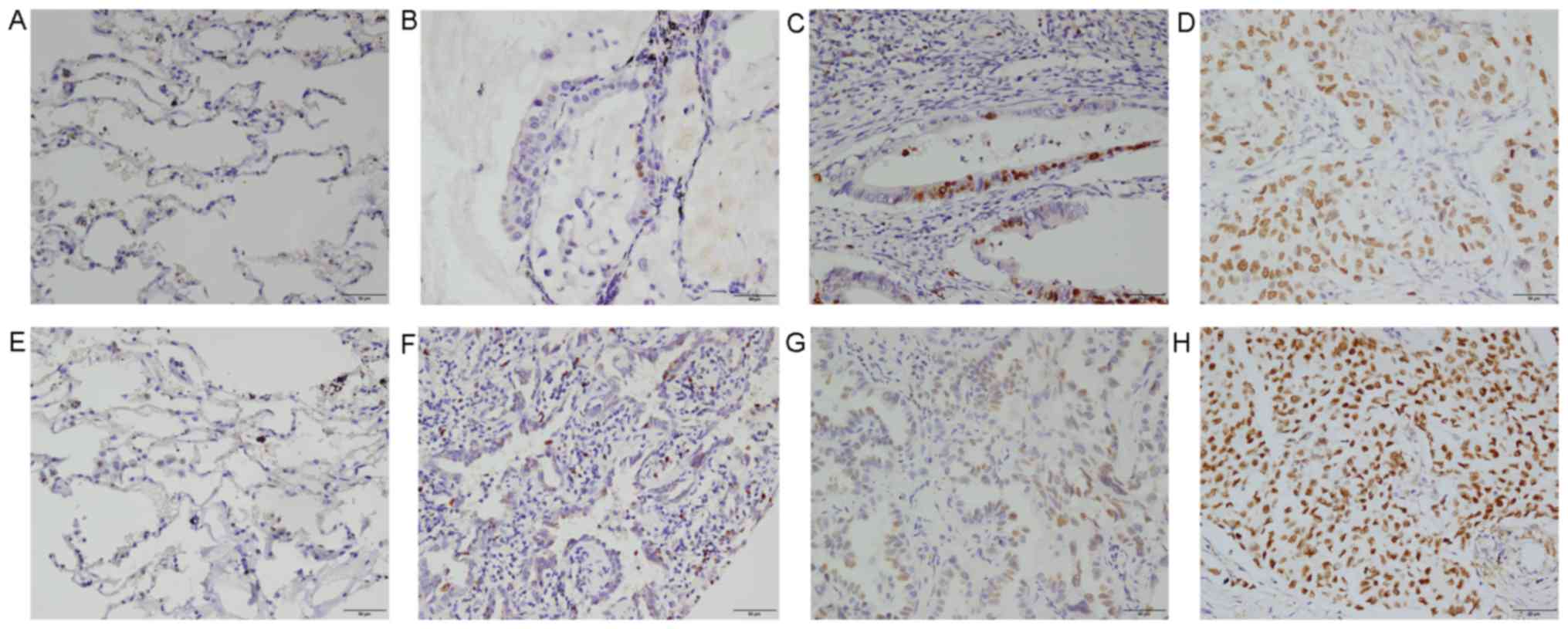
Evaluation of staining
The analysis of these sections following
immunostaining was conducted by two independent experienced
pathologists. Both pathologists were unaware of the clinical
pathological data and patient's outcome. KLF8 was predominantly
located in the cytomembrane, also it was also observed in the
cytoplasm and nuclei. Ki67 was also located in tumor cell nuclei.
The positive cells were those with yellow/brown granules in the
nucleus and whose staining intensity was higher than those with
specific staining in the background. Under the microscope
(magnification, ×400), 100 cells were counted at each site, and the
staining intensity and the percentage of positive cells were
recorded in four sites. The staining intensity score assessment was
as follows: 0, no staining; 1, weakly stained; 2, moderately
stained; and 3, strongly stained. The final score was the product
of KLF8 and Ki67 staining: <3 points was defined as negative and
low staining; and ≥3 points was defined as positive and high
staining.
Statistical analysis
Statistical analysis was performed using SPSS v.
21.0 (IBM Corp., Armonk, NY, USA). The relationship between KLF8,
Ki67 and clinical pathological features of lung adenocarcinoma were
examined using χ2 testing. The correlation between KLF8
and Ki67 was analyzed according to Spearman's rank correlation.
Survival curves were calculated by the Kaplan-Meier method.
P<0.05 was considered to indicate a statistically significant
difference.
Results
KLF8 is present in LAC samples at high
levels
In an attempt to verify whether KLF8 was involved in
LAC, protein expression levels of KLF8 in 8 tumor tissue samples
and adjacent non-tumor tissue were analyzed by western blot
analysis. It was demonstrated that KLF8 expression levels were
markedly higher in tumor samples than in normal lung samples
(Fig. 1). Immunohistochemical
staining was conducted on 140 LAC samples. As demonstrated in
Fig. 2, positive cell percentages of
KLF8 were as follows: <10% (Fig.
2E); F, 11–50% (Fig. 2F); G,
51–75% (Fig. 2G); and >75%
(Fig. 2H).
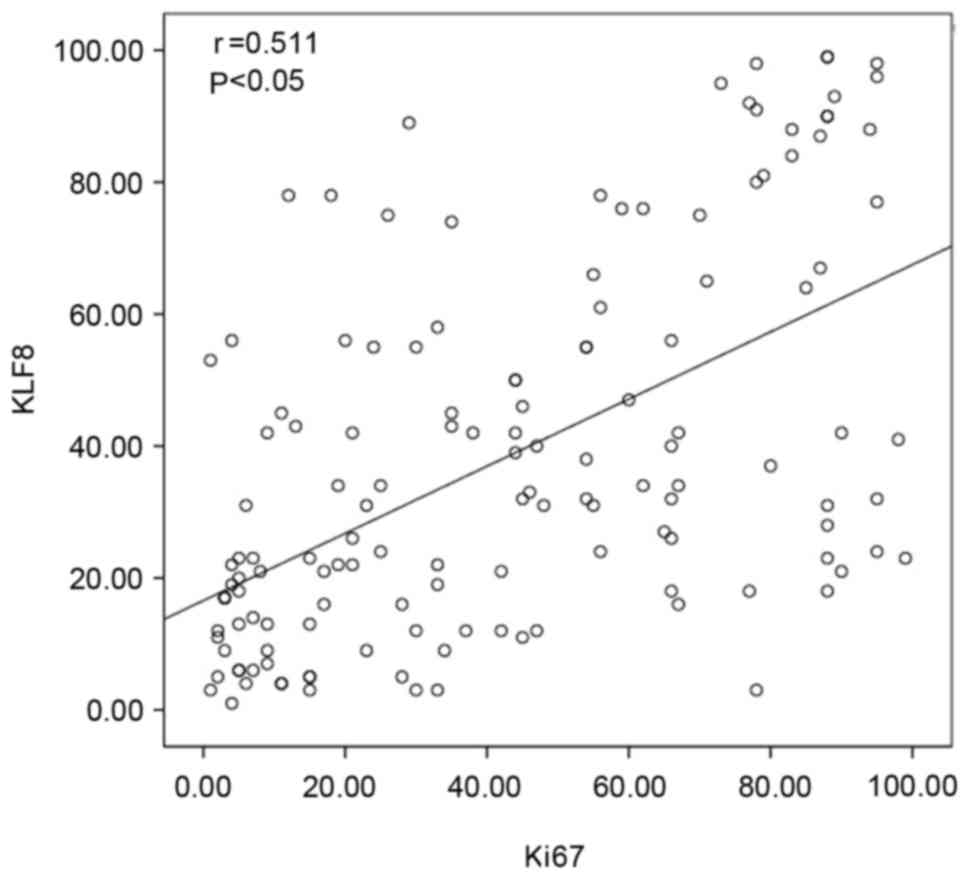
Correlation exists between KLF8
expression and clinical pathological parameters in patients with
LAC
The relationship between KLF8 protein expression
levels and patient clinical pathological parameters (Table I) was analyzed. KLF8 expression was
significantly correlated with differentiation (P=0.035), TNM
(P=0.001), lymph node metastasis (P=0.015) and median survival
(P=0.018). However, no significant association was identified
between KLF8 expression and the other clinical pathological
characteristics, including sex, age and tumor size. Furthermore,
there was a significant positive association between KLF8 and Ki67
expression (Table II; P<0.01).
Additionally, the correlation between KLF8 and Ki67 was analyzed by
using Pearson's rank correlation, which indicated a significant
positive correlation between the expression of these proteins
(r=0.511; P<0.05; Fig. 3).
 | Table I.KFL8 and Ki67 expression and
clinicopathological parameters in 140 lung adenocarcinoma
samples. |
Table I.
KFL8 and Ki67 expression and
clinicopathological parameters in 140 lung adenocarcinoma
samples.
|
|
| KLF8 expression |
|
|
|
|---|
|
|
|
|
|
|
|
|---|
| Parameters | Total | Low | High | % of total | x2 | P-value |
|---|
| Sex |
0.057 |
| Male | 72 | 34 | 38 | 52.8 |
3.623 |
|
|
Female | 68 | 43 | 25 | 36.8 |
|
|
| Age, years |
0.731 |
|
<60 | 60 | 34 | 26 | 43.3 |
0.118 |
|
| ≥60 | 80 | 43 | 37 | 46.3 |
|
|
| Tumor size, cm |
0.170 |
|
<3 | 60 | 37 | 23 | 38.3 |
1.886 |
|
| ≥3 | 80 | 40 | 40 | 50.0 |
|
|
| Differentiation |
0.035 |
| Well | 33 | 23 | 10 | 30.3 |
6.707 |
|
|
Moderate | 71 | 40 | 31 | 43.7 |
|
|
|
Poor | 36 | 14 | 22 | 61.1 |
|
|
| TNM stage |
0.001 |
| I | 69 | 48 | 21 | 30.4 | 16.915 |
|
| II | 34 | 17 | 17 | 50.0 |
|
|
|
III | 31 | 12 | 19 | 61.3 |
|
|
| IV | 6 | 0 | 6 | 100 |
|
|
| Lymph node
metastasis |
0.015 |
| No | 78 | 50 | 28 | 35.9 |
5.896 |
|
|
Yes | 62 | 27 | 35 | 56.5 |
|
|
| Median survival,
months |
0.018 |
|
<37 | 69 | 31 | 38 | 55.1 |
5.577 |
|
|
≥37 | 71 | 46 | 25 | 35.2 |
|
|
| Ki67
expression | <0.01 |
|
High | 101 | 43 | 58 | 57.4 | 22.618 |
|
|
Low | 39 | 34 | 5 | 12.8 |
|
|
 | Table II.Correlation between expression of
KLF8 and Ki67 in 140 lung adenocarcinoma specimens. |
Table II.
Correlation between expression of
KLF8 and Ki67 in 140 lung adenocarcinoma specimens.
|
| KLF8
expression |
|
|
|---|
|
|
|
|
|
|---|
| Ki67
expression | High | Low | r | P-value |
|---|
| High | 58 | 43 | 0.402 | <0.01 |
| Low | 5 | 34 |
|
|
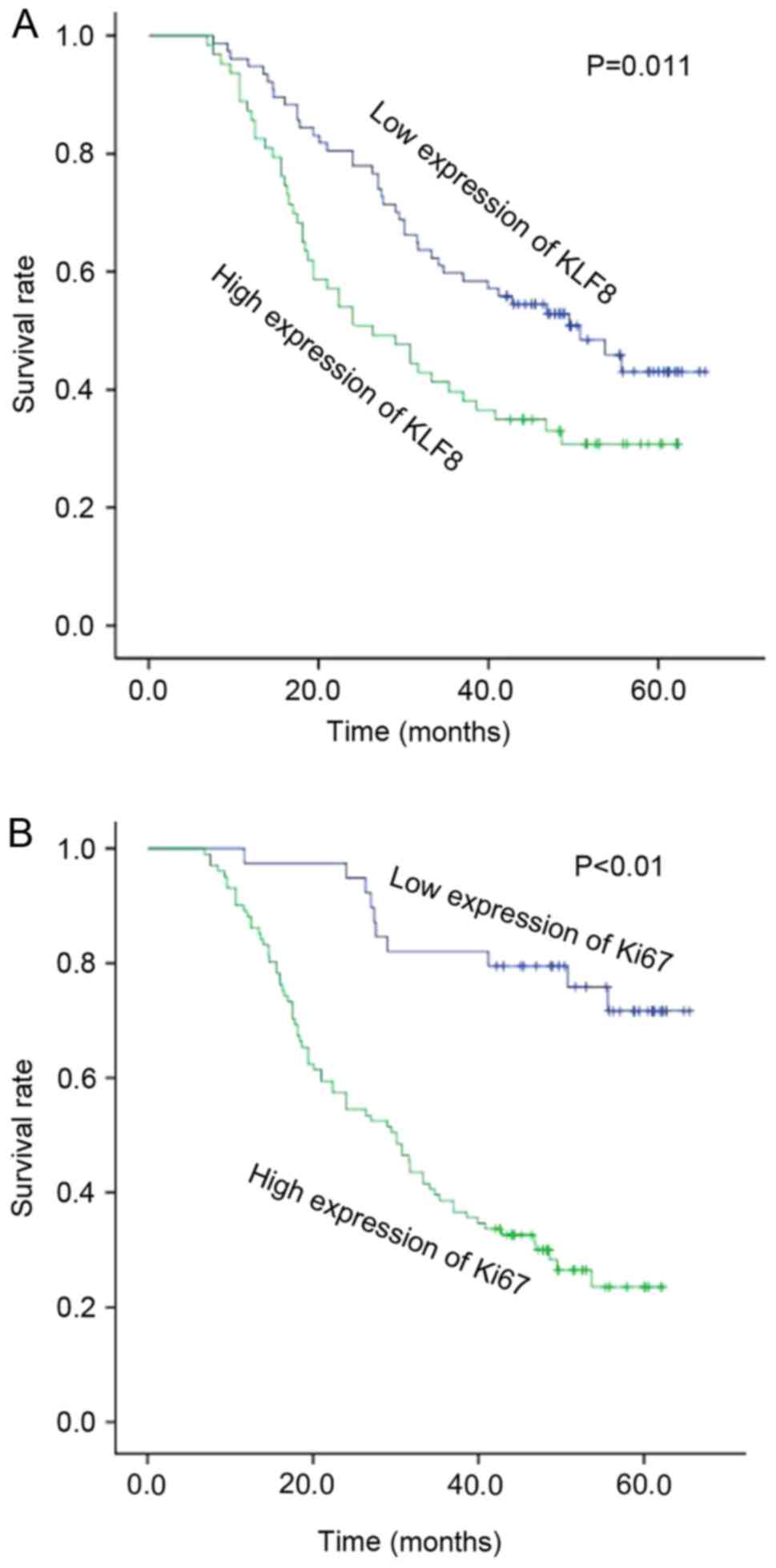
KLF8 and Ki67 expression correlates
with patient survival
The association between KLF8 expression and patient
survival status was investigated. Kaplan-Meier survival curves
demonstrated that high expression of KLF8 was significantly
correlated with poor overall patient survival (Fig. 4A; P=0.011). The prognosis of patients
with high expression of KLF8 was worse than the prognosis of
patients with lower expression levels. Furthermore, patients with
higher expression levels of Ki67 demonstrated a significantly
reduced survival rate compared with those who had low expression
levels of Ki67 (P<0.01; Fig.
4B).
Discussion
Lung cancer is one of the most common malignant
tumors in China (15). The main
causes of lung cancer include smoking, environmental pollution,
population aging and lifestyle changes (15). A variety of molecular pathways and
proteins participate in the development of LAC, and the current
medical level is incapable of diagnosing LAC at an early stage,
meaning that it usually metastasizes before being clinically
diagnosed (3). Therefore, it is
vital to identify new specific molecules to predict LAC
prognosis.
KLFs are recognized as transcriptional inhibitor
proteins of the Kruppel-like cys2/His2 zinc finger protein family
(16). KLFs are DNA-binding
transcription regulation factors, with a highly conserved zinc
finger structure in the C-terminal domain, which may combine with a
variety of gene promoter components, particularly the GC box
(17). The KLF family has an
important role in cell cycle regulation and cell proliferation and
also has an important function in the process of tumor development,
invasion and metastasis (4,18). The KLF family is composed of 14
members, KLF1-14. KLF8 was isolated from K562 leukemia and has been
the focus of research (19). KLF8 is
located on the X chromosome in humans and consists of 359 amino
acid residues (20). The zinc
fingers of KLF8 identify CACCC elements in DNA, and the full-length
KLF8 may inhibit a CACCC-dependent promoter (21). Sometimes the zinc finger domain
regulates protein-protein interactions (4,16). Some
researchers believe that KLF8 may be stimulated by small ubiquitin
like modifiers (SUMO)-1, SUMO-2 and SUMO-3, primarily by SUMO-1
(17). Research has demonstrated
that the function of KLF8 is limited when SUMO-1 is bound at Lys67
(17,22,23).
Various studies have demonstrated that high
expression of KLF8 exists in a variety of tumors, including as
breast (24,25), ovarian (26), bladder (27) and gastric cancer (28,29). A
previous study indicated that KLF8 may act on matrix
metalloproteinase 9 transcription in breast cancer, promoting cell
invasion and metastasis of human breast cancer (24). KLF8 is also tightly regulated by
focal adhesion kinase through Src and phosphoinositide 3-kinase
signaling pathways via transcription factors specificity protein 1,
KLF1 and KLF3 (26,30). KLF8 also regulates the expression of
vimentin and N-cadherin, and increases the expression of β-catenin,
thus promoting the proliferation and migration of bladder cancer
cells (27). In addition, KLF8
regulates epithelial-mesenchymal transition (EMT) induced by
transforming growth factor (TGF)-β1 in gastric cancer cells
(28). Downregulation of KLF8 by
small interfering RNA has been demonstrated to block TGF-β1-induced
EMT-like transformation and TGF-β1-prompted cell migration,
invasion and motility (28).
In the present study, the expression of KLF8 in 8
paired cases of fresh lung adenocarcinoma tissues and non-cancerous
tissues was investigated using western blotting. The results
demonstrated that the expression of KLF8 in lung adenocarcinoma was
markedly higher than that in non-cancerous tissues. Additionally,
the expression of KLF8 and Ki67 in patients with LAC using TMA was
evaluated. High expression of KLF8 was significantly correlated
with differentiation, TNM and lymph node metastasis. Furthermore,
the expression of KLF8 was correlated positively with Ki67. The
patients with high expression levels of KLF8 or Ki67 had a worse
prognosis than those with low expression levels of KLF8. In
conclusion, the KLF8 protein may be a novel therapeutic target for
LAC; however, further study of the molecular mechanisms of KLF8 in
LAC is required.
Acknowledgements
The present study was supported by the Suzhou
Science and Technology Development Program (grant no. SZS201509),
the Jiangsu Provincial Special Program of Clinical Medical Science
(grant no. BL2014040).
References
|
1
|
Liu Y, Lv L, Xue Q, Wan C, Ni T, Chen B,
Liu Y, Zhou Y, Ni R and Mao G: Vacuolar protein sorting 4B, an
ATPase protein positively regulates the progression of NSCLC via
promoting cell division. Mol Cell Biochem. 381:163–171. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Rivera C, Pecuchet N, Wermert D, Pricopi
C, Le Pimpec-Barthes F, Riquet M and Fabre E: Obesity and lung
cancer: Incidence and repercussions on epidemiology, pathology and
treatments. Rev Pneumol Clin. 71:37–43. 2015.(In French).
View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Xu MM, Mao GX, Liu J, Li JC, Huang H, Liu
YF and Liu JH: Low expression of the FoxO4 gene may contribute to
the phenomenon of EMT in non-small cell lung cancer. Asian Pac J
Cancer Prev. 15:4013–4018. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Evans PM and Liu C: New insights into
KLF8-mediated transactivation. Cell Cycle. 9:649–650. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Shi H, Ji Y, Zhang D, Liu Y and Fang P:
MiR-135a inhibits migration and invasion and regulates EMT-related
marker genes by targeting KLF8 in lung cancer cells. Biochem
Biophys Res Commun. 465:125–130. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Schnell O, Romagna A, Jaehnert I, Albrecht
V, Eigenbrod S, Juerchott K, Kretzschmar H, Tonn JC and Schichor C:
Krüppel-like factor 8 (KLF8) is expressed in gliomas of different
WHO grades and is essential for tumor cell proliferation. PLoS One.
7:e304292012. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Chen G, Yang W, Jin W, Wang Y, Tao C and
Yu Z: Lentivirus-mediated gene silencing of KLF8 reduced the
proliferation and invasion of gastric cancer cells. Mol Biol Rep.
39:9809–9815. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Wang X, Urvalek AM, Liu J and Zhao J:
Activation of KLF8 transcription by focal adhesion kinase in human
ovarian epithelial and cancer cells. J Biol Chem. 283:13934–13942.
2008. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Fu WJ, Li JC, Wu XY, Yang ZB, Mo ZN, Huang
JW, Xia GW, Ding Q, Liu KD and Zhu HG: Small interference RNA
targeting Krüppel-like factor 8 inhibits the renal carcinoma 786–0
cells growth in vitro and in vivo. J Cancer Res Clin Oncol.
136:1255–1265. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Wang X and Zhao J: KLF8 transcription
factor participates in oncogenic transformation. Oncogene.
26:456–461. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Schwab U, Stein H, Gerdes J, Lemke H,
Kirchner H, Schaadt M and Diehl V: Production of a monoclonal
antibody specific for Hodgkin and Sternberg-Reed cells of Hodgkin's
disease and a subset of normal lymphoid cells. Nature. 299:65–67.
1982. View
Article : Google Scholar : PubMed/NCBI
|
|
12
|
Leuverink EM, Brennan BA, Crook ML,
Doherty DA, Hammond IG, Ruba S and Stewart CJ: Prognostic value of
mitotic counts and Ki-67 immunoreactivity in adult-type granulosa
cell tumour of the ovary. J Clin Pathol. 61:914–919. 2008.
View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Melling N, Kowitz CM, Simon R, Bokemeyer
C, Terracciano L, Sauter G, Izbicki JR and Marx AH: High Ki67
expression is an independent good prognostic marker in colorectal
cancer. J Clin Pathol. 69:209–214. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Sabattini E, Bisgaard K, Ascani S, Poggi
S, Piccioli M, Ceccarelli C, Pieri F, Fraternali-Orcioni G and
Pileri SA: The EnVision++ system: A new immunohistochemical method
for diagnostics and research. Critical comparison with the APAAP
ChemMate, CSA, LABC, and SABC techniques. J Clin Pathol.
51:506–511. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Siegel R, Ma J, Zou Z and Jemal A: Cancer
statistics, 2014. CA Cancer J Clin. 64:9–29. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Rodriguez E and Martignetti JA: The
Kruppel traffic report: Cooperative signals direct KLF8 nuclear
transport. Cell Res. 19:1041–1043. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Lahiri SK and Zhao J: Krüppel-like factor
8 emerges as an important regulator of cancer. Am J Transl Res.
4:357–363. 2012.PubMed/NCBI
|
|
18
|
Eaton SA, Funnell AP, Sue N, Nicholas H,
Pearson RC and Crossley M: A network of Krüppel-like Factors
(Klfs). Klf8 is repressed by Klf3 and activated by Klf1 in vivo. J
Biol Chem. 283:26937–26947. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Lossi AM, Laugier-Anfossi F, Depetris D,
Gecz J, Gedeon A, Kooy F, Schwartz C, Mattei MG, Croquette MF and
Villard L: Abnormal expression of the KLF8 (ZNF741) gene in a
female patient with an X;autosome translocation
t(X;21)(p11.2;q22.3) and non-syndromic mental retardation. J Med
Genet. 39:113–117. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Lee H, Kim HJ, Lee YJ, Lee MY, Choi H, Lee
H and Kim JW: Krüppel-like factor KLF8 plays a critical role in
adipocyte differentiation. PLoS One. 7:e524742012. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
van Vliet J, Turner J and Crossley M:
Human Krüppel-like factor 8: A CACCC-box binding protein that
associates with CtBP and represses transcription. Nucleic Acids
Res. 28:1955–1962. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Wei H, Wang X, Gan B, Urvalek AM,
Melkoumian ZK, Guan JL and Zhao J: Sumoylation delimits KLF8
transcriptional activity associated with the cell cycle regulation.
J Biol Chem. 281:16664–16671. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Urvalek AM, Lu H, Wang X, Li T, Yu L, Zhu
J, Lin Q and Zhao J: Regulation of the oncoprotein KLF8 by a switch
between acetylation and sumoylation. Am J Transl Res. 3:121–132.
2011.PubMed/NCBI
|
|
24
|
Wang X, Lu H, Urvalek AM, Li T, Yu L,
Lamar J, DiPersio CM, Feustel PJ and Zhao J: KLF8 promotes human
breast cancer cell invasion and metastasis by transcriptional
activation of MMP9. Oncogene. 30:1901–1911. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Lu H, Hu L, Yu L, Wang X, Urvalek AM, Li
T, Shen C, Mukherjee D, Lahiri SK, Wason MS and Zhao J: KLF8 and
FAK cooperatively enrich the active MMP14 on the cell surface
required for the metastatic progression of breast cancer. Oncogene.
33:2909–2917. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Lu H, Wang X, Urvalek AM, Li T, Xie H, Yu
L and Zhao J: Transformation of human ovarian surface epithelial
cells by Krüppel-like factor 8. Oncogene. 33:10–18. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Liang K, Liu T, Chu N, Kang J, Zhang R, Yu
Y, Li D and Lu D: KLF8 is required for bladder cancer cell
proliferation and migration. Biotechnol Appl Biochem. 62:628–633.
2015. View
Article : Google Scholar : PubMed/NCBI
|
|
28
|
Zhang H, Liu L, Wang Y, Zhao G, Xie R, Liu
C, Xiao X, Wu K, Nie Y, Zhang H and Fan D: KLF8 involves in
TGF-beta-induced EMT and promotes invasion and migration in gastric
cancer cells. J Cancer Res Clin Oncol. 139:1033–1042. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Hsu LS, Wu PR, Yeh KT, Yeh CM, Shen KH,
Chen CJ and Soon MS: Positive nuclear expression of KLF8 might be
correlated with shorter survival in gastric adenocarcinoma. Ann
Diagn Pathol. 18:74–77. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Zhao J, Bian ZC, Yee K, Chen BP, Chien S
and Guan JL: Identification of transcription factor KLF8 as a
downstream target of focal adhesion kinase in its regulation of
cyclin D1 and cell cycle progression. Mol Cell. 11:1503–1515. 2003.
View Article : Google Scholar : PubMed/NCBI
|