Introduction
A laryngocele is a rare benign dilatation of the
laryngeal saccule containing air and/or fluid that interacts with
the laryngeal lumen. It may be characterized as internal, exterior
or mixed, depending on its location (1). This condition may be congenital or
acquired and is usually unilateral (2). Laryngocele is considered an uncommon
diagnosis, with a frequency of ~1 in 2.5 million individuals per
year (3). According to other
clinical studies (1,4), males are about five times more likely
than females to suffer from laryngocele. Scholars have reported a
higher incidence of the condition throughout the fifth and sixth
decades of life (5). Common
clinical manifestations include hoarseness of the voice and
swelling of the neck. Imaging studies are critical for making a
diagnosis, determining the type, location and extent of a
laryngocele, and outlining the best treatment options. Despite the
fact that it is a benign condition, a laryngocele may occasionally
appear as an acute airway emergency and be threatening to patients'
lives (6). The definitive surgical
approach and tracheostomy depend on the type of laryngopyocele, its
presentation and the patient's comorbidities. Since laryngopyoceles
are rarely reported, no large case series has been published to
date, to the best of our knowledge (7). This article introduces the management
of an internal laryngocele and mixed laryngocele along with review
of literature and proposed plasma resection of laryngoceles.
Case report
Case 1
A 59-year-old male patient who had been complaining
of hoarseness for almost 1 year presented at Affiliated Hospital of
Jining Medical University in February 2022. The patient had been
treated with ‘traditional medicine’, but his condition did not
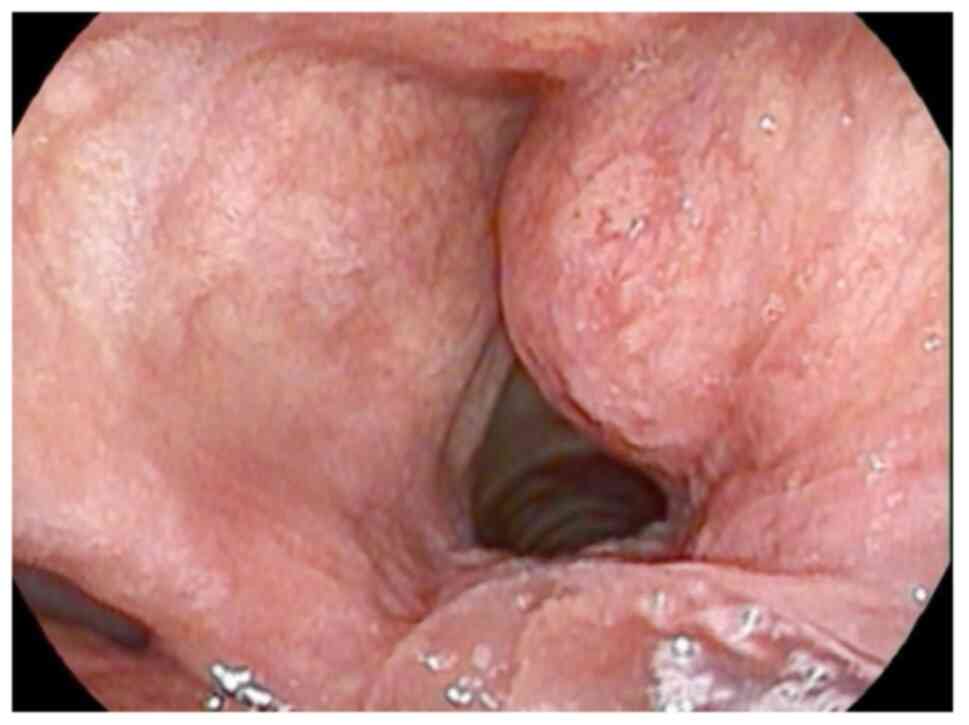
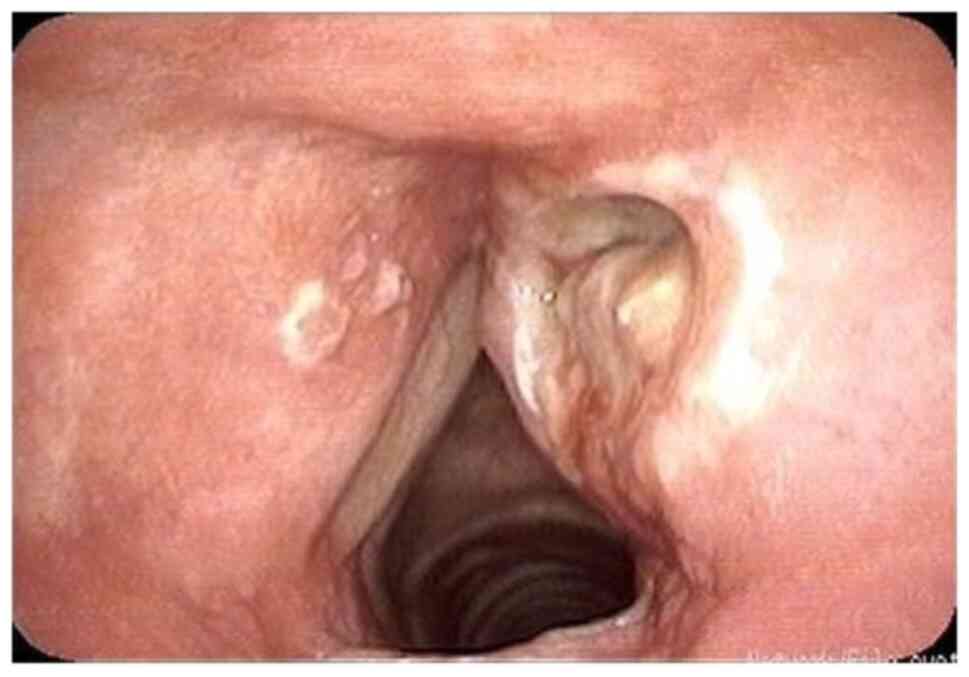
sufficiently improve. This time, laryngoscopy revealed an expanded
right false vocal fold with unremarkable underlying mucosa
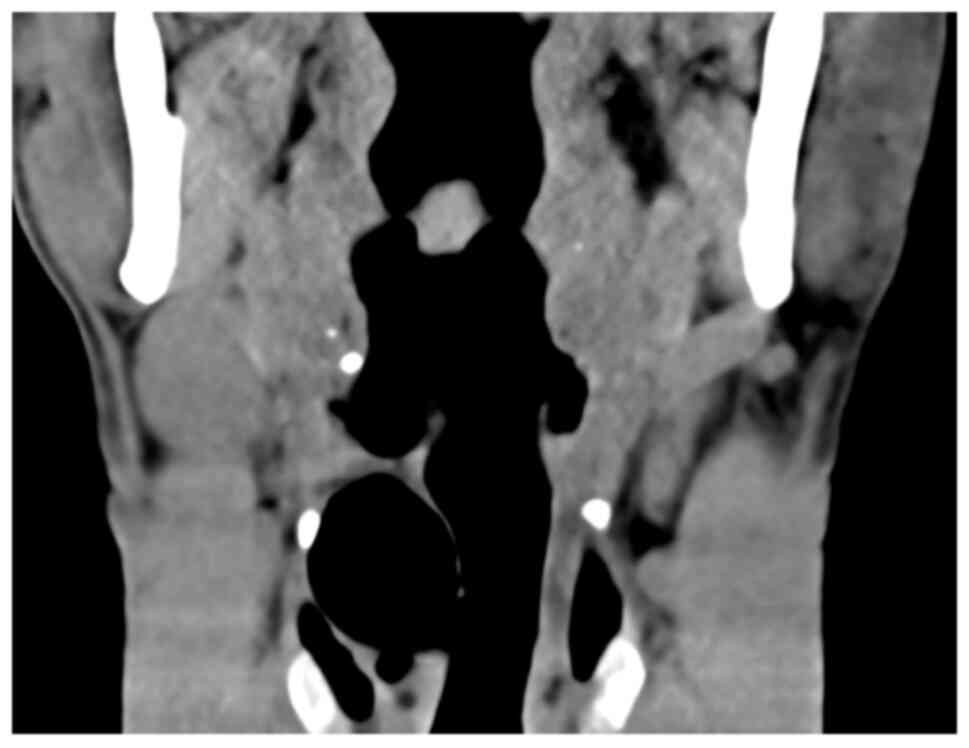
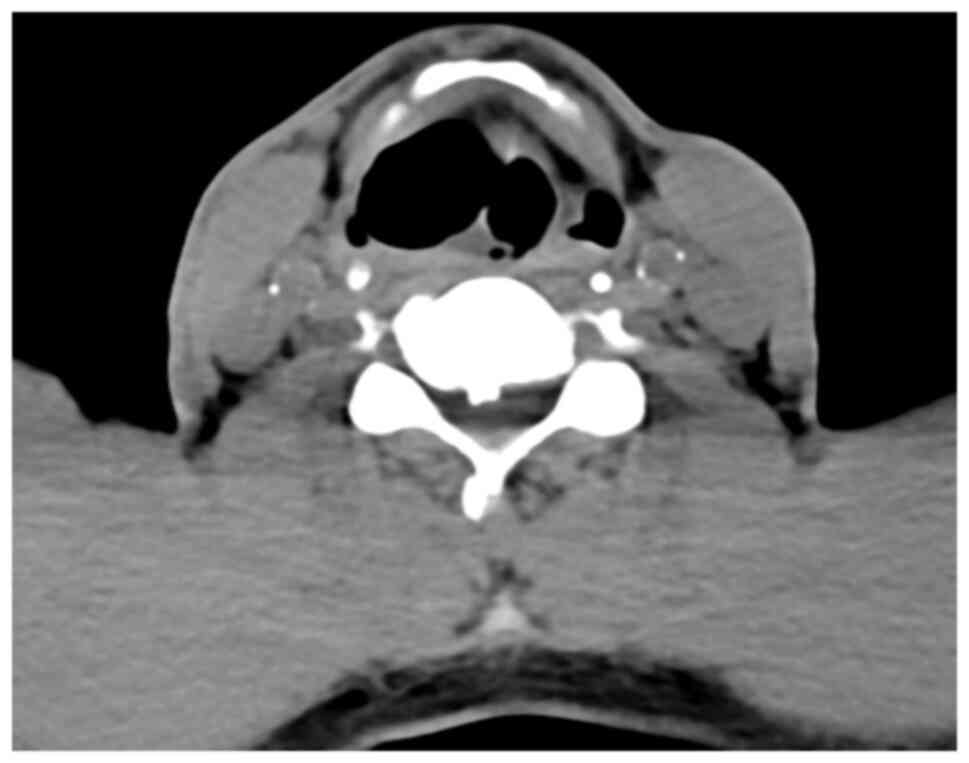
(Fig. 1). Neck CT in the coronal
plane (Fig. 2) and axial plane
(Fig. 3) indicated a cystic
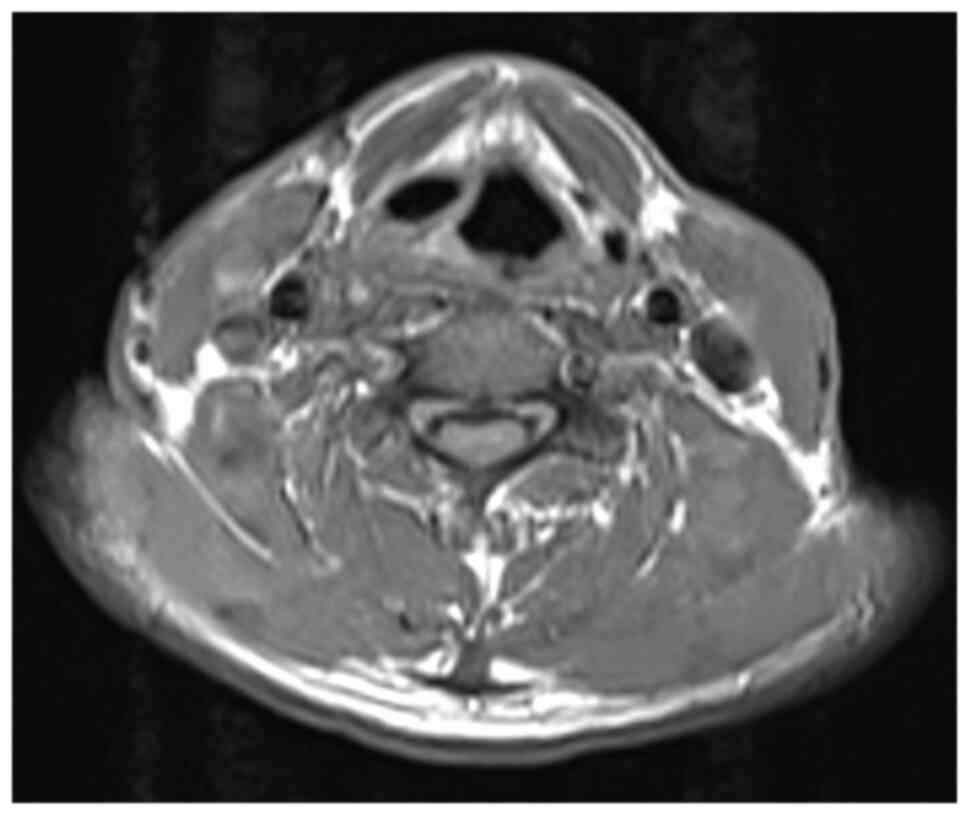
dilatation on the right side of the larynx. MRI showed a
1.3x0.7x1.9 cm cystic dilatation on the right side of the larynx,
towards the level of the 4-5 cervical vertebra. Small patchy areas
surrounding the saccular dilatation were hypointense on T1-weighted
imaging (T1WI) and hyperintense on T2WI (Fig. 4). After analysing the results,
laryngocele was considered along with certain infectious diseases.
The patient had no edema on either side of the upper neck and was
diagnosed with internal laryngocele after admission. Surgical
therapy was performed after all contraindications were ruled
out.
The medical team used a suspension laryngoscope to
evaluate the right laryngeal ventricle bulge. The first procedure
was to use plasma to excise the mucosa over the cyst and the
laryngeal ventricle mucosa. After the excision along the root of
the mass was completed, an intraoperative clear fluid with visible
bubbles flowed from the capsule, and the root was cauterized with
plasma radiofrequency ablation. Once the laryngocele was totally
removed, the incision was rinsed and checked for bleeding. The
operation was completed successfully without any surgical harm to
the vocal cords. After the procedure, it was concluded that there
was also no need for a tracheostomy. On the second postoperative
day, a laryngoscope revealed white pseudomembrane adherence on the
trauma surface, with no obvious swelling (Fig. 5). There were no perioperative or
early postoperative issues. Within 24 h, the patient was allowed to
resume his oral diet. A follow-up was conducted 6 months after the
procedures and the patient showed no recurrence or other relevant
changes to his clinical condition.
Case 2
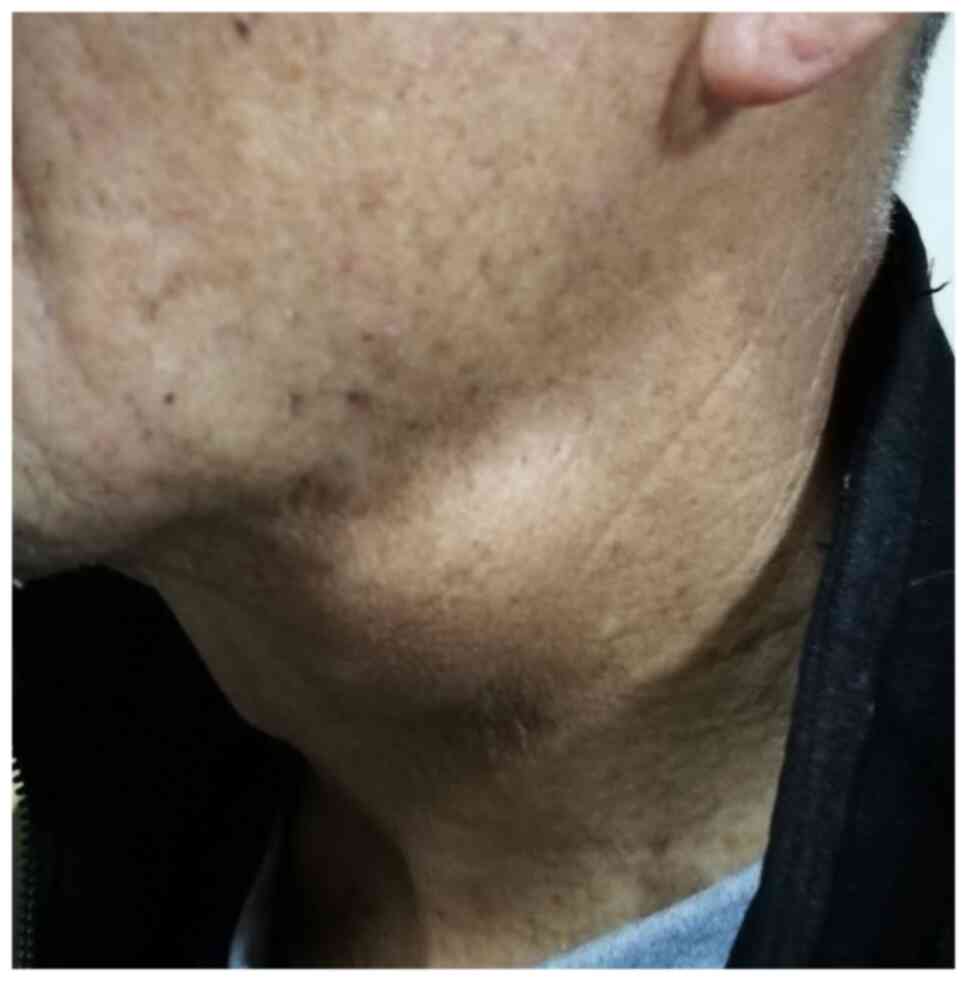
A 68-year-old male patient presented at the
Affiliated Hospital of Jining Medical University in December 2017
with a major sign of a swelling on the left side of the upper
aspect of the neck (Fig. 6) and
complained of pain for >1 month. Upon coughing or using the
Valsalva maneuver, the swelling grew larger. The patient reported
that recently, the swelling's size had been progressively
increasing and that he had been frequently experiencing
breathlessness and hoarseness after activities. The results of a
laryngoscopy revealed a cystic neoplasm with a smooth surface in
the left ventricle zone and normal mobility of the bilateral vocal
cords. The patient works as a farmer and has a positive smoking
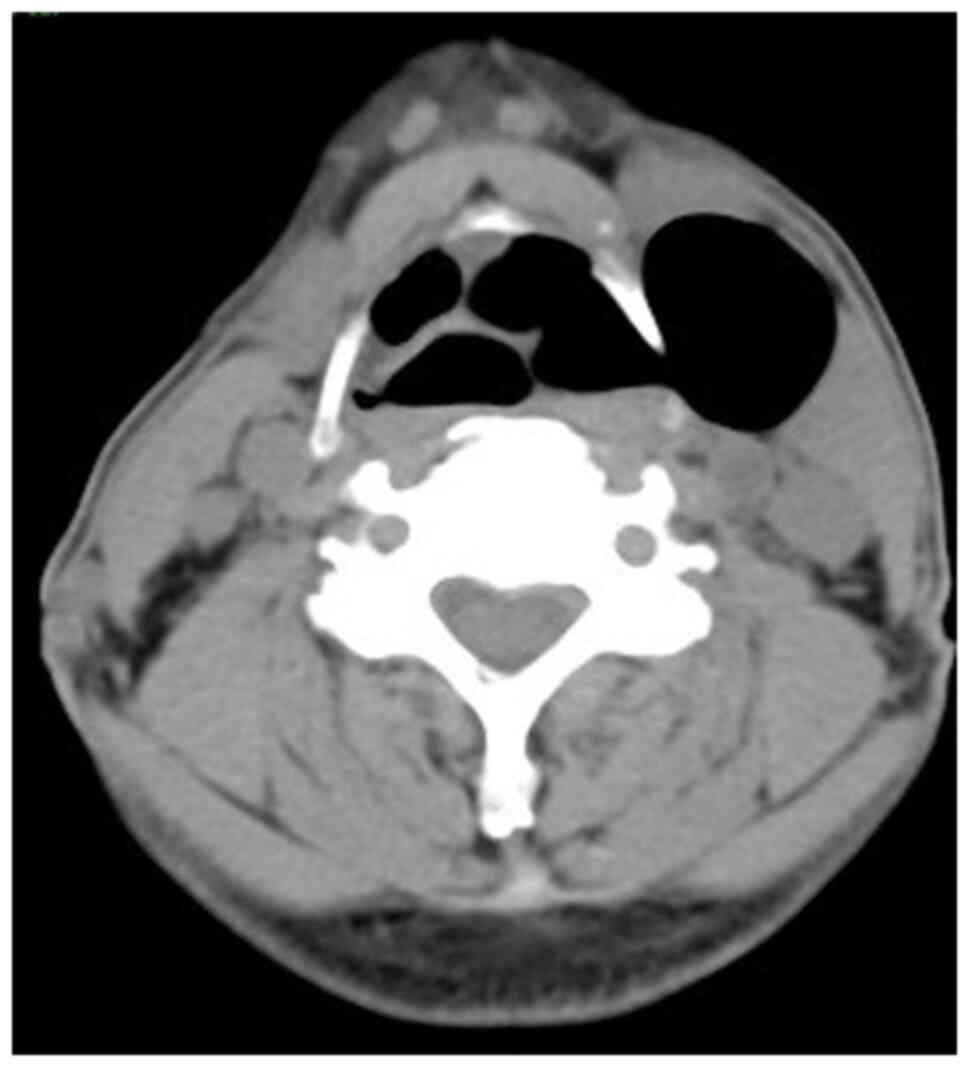
history. After collection of the case data, the patient underwent a
complete CT scan, which revealed a huge air-filled lump in the left
neck (Fig. 7). Furthermore, on
MRI, a 4.3x3.1x4.6 cm rounded aberrant signal was visible in the
left false vocal cords. The lesion had a clear boundary and a
homogeneous signal, which was hypointense on T1WI and T2WI and
absent on diffusion-WI and spread to the neck, leading to the
diagnosis of a combination laryngocele.
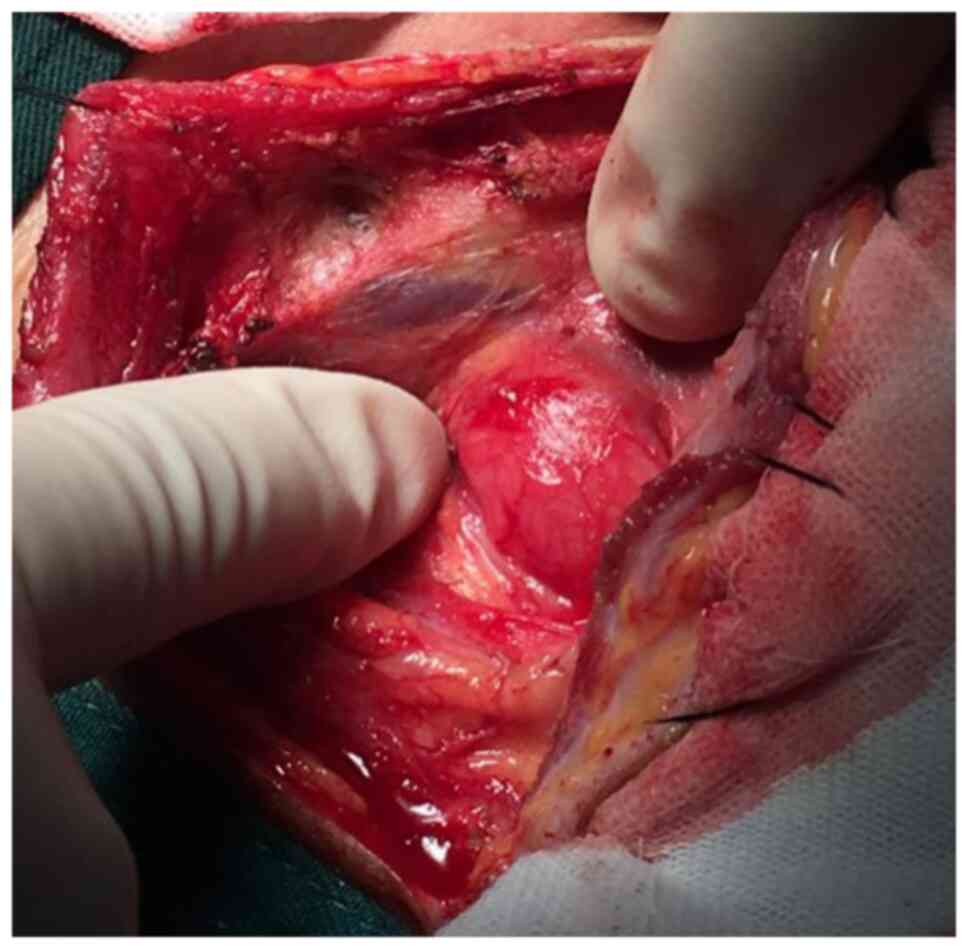
Routine tests were subsequently performed and the
patient was prepped for excision by an external transcervical
technique under general anesthesia. An incision was made at the
anterior border of the sternocleidomastoid muscle, approximately at
the level between the hyoid bone and the thyroid cartilage,
meticulously separated from its surroundings (Fig. 8). The tumor entered the laryngeal
cavity via the left lower margin of the epiglottis, then the left
laryngeal chamber and finally the median split laryngeal cavity.
During the procedure, the medical team discovered that it had
extended to the anterior commissure. After being peeled off to the
root of the cyst, the mass was removed after ligation at the root.
Rapid pathology revealed benign cystic lesions, so a tracheostomy
was performed. The pathological features observed after the
operation revealed a cyst lined with ciliated columnar epithelium.
A laryngoscopy was conducted one week after the surgery and showed
that the wound had closed without any recurrences (Fig. 9).
Discussion
Dr Larrey, a distinguished physician of Napoleon's
forces in Egypt, reported laryngocele for the first time in 1829.
However, the condition was officially defined by Virchow many years
later, in 1867(8). Most
specialists divide laryngocele into three types (9): i) Internal, which is restricted to
the thyrohyoid membrane and presents as a mass in the false vocal
cord; ii) external, which extends into the neck subcutaneous
tissue; and iii) a combination of both. Al-Yahya et al
(7) analysed 61 papers published
between 1952 and 2015, concluding that 79% of the diagnosed cases
were combined, 17% were internal and 4% were external.
When the neck of a diagnosed patient with
laryngocele is constricted, it can be filled with mucus and develop
into a laryngomucocel, which may escalate into a laryngopyocele
once infected (10). While this
scenario is considered unlikely, it may have serious consequences,
such as acute airway blockage and dysphagia (7). According to Zelenik et al
(11), the incidence of
laryngopyoceles in general laryngoceles cases is 5-8%.
Over 85% of laryngoceles cases are unilateral
(12) and >8% become infected
and develop into a laryngopyocele, with the major consequence being
throat enlargement (13). The
death of diagnosed patients usually results from either accumulated
pus causing airway blockage or pus discharge into the airway
resulting in aspiration death.
It is worth mentioning that the pathogenesis of
laryngocele is still unclear. Several etiologies of laryngocele
were identified in the literature, including a congenital origin,
increased intralaryngeal pressure and mechanical obstruction
(14). According to most scholars,
laryngocele may be either congenital or acquired. In newborns, they
may be identified by an abnormal enlargement of the laryngeal
saccule. By contrast, an acquired laryngocele is caused by a
congenital malformation of the patient's laryngeal ventricle or is
a consequence of the obstruction of the laryngeal ventricle opening
by laryngeal tumors or scarring causing a valve effect.
The relationship between laryngoceles and laryngeal
cancer is also controversial, despite the large amount of studies
focusing on both phenomena. Soler et al (15) treated a total of 60 cases of
laryngoceles, 35 of which developed into laryngeal cancer. McDonald
et al (16) reported that
4.9-28.8% of patients with laryngeal cancer with laryngoceles
included in their study developed laryngoceles induced by laryngeal
cancer blocking the opening of the laryngeal chambers and creating
a one-way valve that allowed air to enter and exit easily,
resulting in increased internal pressure. However, in certain
studies, the results were completely different from this. Close
et al (17) followed up 38
patients with laryngoceles and none of them developed cancer.
Various studies have also reported on laryngoceles
complicated by laryngeal carcinoma (18,19).
Although none of the patients of the present study developed
laryngeal cancer, it was important to remain alert and conduct
pathological examinations after surgery to review patient data
regularly. In a proper follow-up, any signs of laryngeal cancer may
be detected early and treated properly to avoid worsening of the
case.
Marom et al (20) reported two cases of laryngoceles
secondary to neck surgery. These occurrences are a reminder that
the diagnosis of laryngocele may also be associated with local
irritants. However, the patients of the present study are both
farmers who frequently engage in manual labor and do not have any
history of neck surgical intervention, and thus, this scenario is
unlikely to be associated with their conditions. They had all
smoked for >40 years, but had no history of exposure to poisons,
dust or radioactive substances. There was no evidence of laryngeal
carcinoma.
Speech hoarseness and neck enlargement are the most
common clinical findings among diagnosed patients, frequently
resulting in dysphagia, pain, stridor and snoring. While the
majority of laryngocele cases are asymptomatic (21), symptoms may differ depending on the
type of disease. Internal laryngoceles may cause coughing,
hoarseness, sore throat, dysphonia, dysphagia, stridor and even
airway obstruction. On the other hand, external laryngocele
frequently appears as a compressible neck mass between the
sternocleidomastoid and hyoid bones. The Valsalva movement,
coughing and breath-holding may increase the volume of the mass,
making it more prominent and identifiable.
Cases of combined laryngoceles may have symptoms of
both internal and external laryngoceles and may have severe health
consequences, particularly dyspnea, which is caused when the air
moves from the outside of the laryngocele to the inside after the
outside mass is squeezed (7). One
of the patients included in the present study had an internal
laryngocele, which caused hoarseness. The other patient with
combined laryngocele presented to our department complaining of a
painless swelling across his neck throughout the preceding month,
as well as choking after activities. With coughing and the Valsalva
technique, the swelling increased gradually and considerably.
High-quality imaging is essential for the diagnosis
of a laryngocele. Currently, CT scans are the most precise
radiological method (22) and may
help diagnose and classify patients, and guide clinicians to
accurately locate lesions, observe specific size ranges and examine
the relationship between surrounding tissues. CT examination of
cysts with complete gas or the presence of a gas-liquid plane is
the most effective diagnostic basis in cases of cystic mass
connected to the larynx cavity, which may be distinguished from the
neck branchial cleft cyst, thyroid bone cyst, neck epidermoid cyst,
submandibular gland cyst and other types of masses. Numerous
professionals suggest that a CT scan is the gold standard, with MRI
having an adjuvant role in the diagnosis of laryngoceles.
MRI provides extensive information on the
laryngocele's boundary and its relation to the thyrohyoid membrane.
The method may also be used to identify cases of blocked mucus,
inflammation and malignant illness and distinguish between
laryngopyocele, laryngomucocele and ordinary laryngocele. On MRI,
an air-filled laryngocele frequently displays as a low-signal
cystic dilatation of the laryngeal ventricle. If there is a
possibility of a contemporaneous laryngeal tumor and a laryngocele,
this is the best technique to obtain more accurate data regarding a
patient's clinical condition. MRI images can clearly show the
paralaryngeal space, thyrohyoid membrane, and genuine and false
folds, which is helpful to pursue the right diagnosis.
Ultrasonography of the neck may be used to perform
an initial assessment of a neck mass, primarily to differentiate
the type of the lesion and define its contents and position
(23). According to numerous
clinicians, a CT scan can help determine the nature, location and
laryngeal structures of a laryngopyocele. Although MRI delivers
high-quality images of the soft tissue and may be beneficial during
the diagnostic process, it is still a costly method (15). Thus, at our department, electronic
laryngoscopy is usually performed first in patients with
hoarseness, and CT and MRI are routinely performed in patients with
suspected laryngoceles to further confirm the diagnosis and
determine the scope of surgery.
A small number of cases of laryngopyocele regression
with only the use of antibiotics have been recorded. In most cases,
the most successful therapy is still surgical intervention. While
surgery is the treatment of choice for laryngocele, the type of
surgery is mostly determined by the size and type of laryngocele.
Small internal laryngoceles should be removed utilizing an oral
route, but large internal, external or mixed laryngoceles have
traditionally been treated by external surgery. In certain cases, a
tracheotomy is necessary for the transcervical approach (24,25).
Tracheostomy has been performed as an emergency
operation to reduce the risk of respiratory distress, suggesting
that laryngocele may also present as an emergency. This type of
intervention may be performed in 10-20% of individuals with
laryngopyocele who have acute airway impairment (8). Zelenik et al (13) described three types of external
surgery: The trans-thyrohyoid membrane approach (no thyroid
cartilage resection), thyrotomy with top 1/3 thyroid cartilage
removal and V-shaped thyrotomy. In addition, other studies have
suggested that microlaryngoscopic resection with a CO2
laser or cold instruments, marsupialization and endoscopic robotic
surgery may be used in endolaryngeal surgery. The advantages of
external approaches are excellent exposure of the laryngocele,
precision, lower recurrence rates and minimal morbidity, as well as
negligible complications. On the other hand, skin scarring, longer
operation time and inpatient stay, and a higher cost are all
drawbacks of such techniques.
Endolaryngeal surgery now yields much better results
for patients thanks to advances in microsurgical technology.
Furthermore, as compared to an external approach, the endolaryngeal
procedure eliminates the need for a tracheotomy, avoids scarring of
the neck skin and causes less impairment to the glottic area, vocal
function and laryngeal structural muscles. Patients also have
shorter surgical times and hospital stays, and they may resume
their normal diets sooner. However, it is still important to
consider that the endolaryngeal treatment for laryngoceles provides
limited surgical exposure, causing endolaryngeal scarring, and also
requires highly specific tool training (26,27).
Since its introduction in otolaryngology head and
neck surgery in 2000, low-temperature plasma was originally used
for tonsillectomy. It has also been used for surgical resection of
benign and malignant tumors, performing a variety of functions
including cutting, hemostasis, attraction and flushing. This method
of intervention has been adapted and adjusted by clinicians to look
at different angles of the endoscope and process ‘hidden’ positions
that cannot be seen directly under endoscopy, achieving positive
outcomes (27). The procedure
performed at our clinic relied on low-temperature plasma for the
treatment of the patient diagnosed with internal laryngocele and
the results were satisfying, positively affecting voice quality and
swallowing. To our knowledge, the present study is a pioneer for
the use of low-temperature plasma to treat internal laryngocele.
The preoperative imaging of the patient was evaluated, indicating
that the patient had internal laryngocele with limited lesions, and
the surgeon had rich clinical experience in endoscopic plasma
resection of laryngeal lesions. Therefore, endoscopic
low-temperature plasma radiofrequency surgery was an option for
this patient. However, due to the small number of patients, the
success rate, intraoperative precautions, postoperative
complications, long-term prognosis and other issues still require
more extensive research. The case of mixed laryngocele was treated
by a transcervical approach and required a tracheotomy. Although
the interventions were more severe, the patient had no recurrence
and remains alive.
As already mentioned, the main complication of
laryngocele is laryngopyocele, but other complications may also
include aspiration of pathogens, subsequent bronchitis and
pneumonia, rupture and upper airway obstruction after infection.
Thus, both conditions may lead to sudden death. Maweni et al
(28) presented data that
suggested that in >8% of cases, diagnosed patients may develop
laryngopyocele. Although laryngocele is still considered a benign
and rare clinical entity, it occasionally presents as an acute
respiratory emergency that may be life-threatening. Certain fatal
cases of laryngocele have also been reported in other related
studies. Töro et al (29)
presented the case of a 55-year-old housewife with a blocked
combined laryngocele who refused emergency treatment and died
minutes after being discharged. Another 70-year-old male with
laryngocarcinoma was found dead in his bed while waiting for
surgery. The autopsy revealed that the subject was suffering from
an internal type of laryngocele and the asphyxia was caused by a
mucous sputum filling the larynx, which was released by the right
llaryngocele (30). Byard and
Gilbert (31) also reported one
case of death from laryngopyceles secondary to airway obstruction.
Congenital laryngoceles may also cause respiratory distress and
possibly death in newborns (32).
In other cases, the spontaneous rupture of internal or external
components spilling into the airway or parapharyngeal space may
lead to a mediastinal abscess or jugular vein thrombosis (33).
Although laryngoceles and laryngopyoceles are
considered uncommon diagnoses in clinical practice, they should
still be considered in the differential diagnosis of any patient
with a history of hoarseness, varying degrees of airway obstruction
and smooth ventricle enlargement. It is important to recognize the
existence of such conditions because the lesions, although easily
curable, may still be fatal in rare cases. The successful treatment
of a patient included in the present study demonstrated that the
application of low-temperature plasma is an advantageous clinical
method that may be used to treat cases of internal laryngocele. The
other aspect that is important to consider is that, due to the
possibility of laryngoceles associated with tumors, doctors need to
retain the tissue for pathological examination as a best practice
to avert further and more serious consequences of the
condition.
Acknowledgements
Not applicable.
Funding
Funding: This study was financially supported by grants from
Jining City Key Research and Development Project of Jining Science
and Technology Bureau (grant nos. 2021YXNS028, 2021YXNS048 and
2021YXNS052), Research Fund project of Academician Helin New
Medical Clinical Transformation Workstation (grant no.
JYHL2022FMS11) and Special Research Plan of Attending Physician
Team of the Affiliated Hospital of Jining Medical College (grant
no. ZZTD-2022-007).
Availability of data and materials
The datasets used and/or analyzed during the current
study are available from the corresponding author on reasonable
request.
Authors' contributions
YGW substantially contributed to the conception and
design of the study. PPS and JZ collected and analyzed the
patients' data. XYL and YGW determined the final surgical method.
XYL performed surgical treatment for case 2, with PPS and XM as his
assistants. With the help of JZ, YGW performed surgery on case 1.
XM followed up the patients. JZ and XM collected, read and shared a
large number of studies in the Chinese and English languages on
laryngocele and wrote the manuscript. PPS and YGW provided critical
revisions of the intellectual content. XYL and YGW confirmed the
authenticity of all the raw data. All authors have read and
approved the final manuscript.
Ethics approval and consent to
participate
Not applicable.
Patient consent for publication
Written informed consent has been obtained from the
two patients to publish the present study, including patient
information, laboratory test results and treatment procedures.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Keles E, Alpay HC, Orhan I and Yildirim H:
Combined laryngocele: A cause of stridor and cervical swelling.
Auris Nasus Larynx. 37:117–120. 2010.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Bisogno A, Cavaliere M, Scarpa A, Cuofano
R, Troisi D and Iemma M: Left mixed laryngocele in absence of risk
factors: A case report and review of literature. Ann Med Surg
(Lond). 60:356–359. 2020.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Trivedi S, Karna ST, Baghel KS and Thaware
P: Undiagnosed laryngocele: An airway emergency. BMJ Case Rep.
15(e248126)2022.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Stell PM and Maran AG: Laryngocoele. J
Laryngol Otol. 89:915–924. 1975.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Juneja R, Arora N, Meher R, Mittal P,
Passey JC, Saxena A and Bhargava EK: Laryngocele: A rare case
report and review of literature. Indian J Otolaryngol Head Neck
Surg. 71(Suppl 1):S147–S151. 2019.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Spinosi MC, Mezzedimi C, Monciatti G and
Passali D: Internal laryngocele: Unusual onset in a 91-year-old
female patient. Sultan Qaboos Univ Med J. 18:e104–e106.
2018.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Al-Yahya SN, Baki MM, Saad SM, Azman M and
Mohamad AS: Laryngopyocele: Report of a rare case and systematic
review. Ann Saudi Med. 36:292–297. 2016.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Prasad KC, Vijayalakshmi S and Prasad SC:
Laryngoceles-presentations and management. Indian J Otolaryngol
Head Neck Surg. 60:303–308. 2008.PubMed/NCBI View Article : Google Scholar
|
|
9
|
James DL, Garry S, Corbett M and Lang J:
Mixed infected laryngocoele presenting as airway obstruction: A
case report. J Surg Case Rep. 2021(rjaa615)2021.PubMed/NCBI View Article : Google Scholar
|
|
10
|
de Campos MÁ, de Siqueira EC, de Souza
FTA, Gama HVP, Gomide TP, Faleiro CSF, Prado FFM, Antunes PRB and
Álvares MCB: Mixed laryngocele mimicking thyroid nodule. J
Ultrasound. 25:733–736. 2022.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Zelenik K, Stanikova L, Smatanova K, Cerny
M and Kominek P: Treatment of Laryngoceles: What is the progress
over the last two decades? Biomed Res Int.
2014(819453)2014.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Dhambri S, Tebini M, Turki S, Dhaha M,
Jebali S, Kedous S, Touati S and Gritli S: Bilateral external
laryngocele: A case report. Tunis Med. 97:736–738. 2019.PubMed/NCBI
|
|
13
|
Lebecque O, Coulier B and Cloots V:
Laryngopyocele. JBR-BTR. 95:74–76. 2012.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Biswas S and Saran M: Blunt trauma to the
neck presenting as dysphonia and dysphagia in a healthy young
woman; A rare case of traumatic laryngocele. Bull Emerg Trauma.
8:129–131. 2020.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Matiño Soler E, Martínez Vecina V, León
Vintró X, Quer Agustí M, Burgues Vila J and de Juan M: Laryngocele:
clinical and therapeutic study of 60 cases. Acta Otorrinolaringol
Esp. 46:279–286. 1995.PubMed/NCBI
|
|
16
|
McDonald SE, Pinder DK, Sen C and Birchall
MA: Oncocytic cyst presenting as laryngocele with surgical
emphysema. Eur Arch Otorhinolaryngol. 263:237–240. 2006.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Close LG, Merkel M, Burns DK, Deaton CW Jr
and Schaefer SD: Asymptomatic laryngocele: Incidence and
association with laryngeal cancer. Ann Otol Rhinol Laryngol.
96:393–399. 1987.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Rosso M, Marjanović K, Males J, Sepić T,
Segec I, Rosso M and Manestar D: .: Bilateral laryngoceles in
association with squamos cell carcinoma: A case report and
literature review. Coll Antropol. 34:727–730. 2010.PubMed/NCBI
|
|
19
|
Akdogan O, Ibrahim O, Selcuk A and Dere H:
The association of laryngoceles with squamous cell carcinoma of the
larynx presenting as a deep neck infection. B-ENT. 3:209–211.
2007.PubMed/NCBI
|
|
20
|
Marom T, Roth Y and Cinamon U:
Laryngocele: A rare long-term complication following neck surgery?
J Voice. 25:272–274. 2011.PubMed/NCBI View Article : Google Scholar
|
|
21
|
Sakci Z, Aydin Y and Ogul H: Reformatted
thoracic computed tomography imaging findings of an internal
laryngocoele. Br J Hosp Med (Lond). 82:1–2. 2021.PubMed/NCBI View Article : Google Scholar
|
|
22
|
Storck C and Buitrago-Tellez C:
Multidetector computed tomography in nonmalignant laryngeal
disease. Curr Opin Otolaryngol Head Neck Surg. 20:443–449.
2012.PubMed/NCBI View Article : Google Scholar
|
|
23
|
Swain SK, Chandra Mallik K, Mishra S and
Chandra Sahu M: Laryngocele: Experience at a tertiary care hospital
of eastern India. J Voice. 29:512–516. 2015.PubMed/NCBI View Article : Google Scholar
|
|
24
|
Kusunoki T, Wada R, Homma H, Kidokoro Y,
Yanai A and Ikeda K: . Two cases of the laryngeal cystic lesions.
Clin Pract. 6(822)2016.PubMed/NCBI View Article : Google Scholar
|
|
25
|
Mobashir MK, Basha WM, Mohamed AE, Hassaan
M and Anany AM: Laryngoceles: Concepts of diagnosis and management.
Ear Nose Throat J. 96:133–138. 2017.PubMed/NCBI View Article : Google Scholar
|
|
26
|
Kozhanov AL, Kozhanov LG, Kravtsov SA and
Sdvizhkov AM: Modern aspects of organ-preserving surgery for
laryngeal cancer. Vestn Otorinolaringol. 87:44–50. 2022.PubMed/NCBI View Article : Google Scholar : (In Russian).
|
|
27
|
Xiao SF, Zhao X, Zhang JB, Shen H and Zhao
EM: Clinical observation of coblation assisted transoral
microsurgery for the treatment of foral and oropharygneal
malignancy. Lin Chuang Er Bi Yan Hou Tou Jing Wai Ke Za Zhi.
31:1705–1710. 2017.PubMed/NCBI View Article : Google Scholar : (In Chinese).
|
|
28
|
Maweni RM Jr, Shirazi S, Chatzoudis D and
Das S: Laryngopyocoele with contralateral laryngocoele: A rare
cause of respiratory distress. BMJ Case Rep.
2018(bcr2018225444)2018.PubMed/NCBI View Article : Google Scholar
|
|
29
|
Töro K, Kardos M and Dunay G: Fatal
asphyxia due to laryngomucocele. Forensic Sci Int. 190:e1–e4.
2009.PubMed/NCBI View Article : Google Scholar
|
|
30
|
Satou T, Naito T, Hayashi Y, Hashimoto S
and Sugiyama S: A sudden death case of laryngocele accompanied by
infarction of the dorso-lateral portion of the medulla oblongata.
Leg Med (Tokyo). 1:257–261. 1999.PubMed/NCBI View Article : Google Scholar
|
|
31
|
Byard RW and Gilbert JD: Lethal
laryngopyocele. J Forensic Sci. 60:518–520. 2015.PubMed/NCBI View Article : Google Scholar
|
|
32
|
Taskinlar H, Vayisoglu Y, Avlan D, Polat A
and Nayci A: Congenital laryngomucocele: A rare cause of airway
obstruction in a newborn. J Craniofac Surg. 26:e238–e240.
2015.PubMed/NCBI View Article : Google Scholar
|
|
33
|
Krekorian EA: Laryngocele and
laryngopyocele. Laryngoscope. 72:1297–1312. 1962.PubMed/NCBI View Article : Google Scholar
|