Introduction
First reported by Rosenthal et al (1) in 1953, congenital factor XI
deficiency (CFXI) is a disease that causes deficiency in the
endogenous coagulation factor XI. It is also known as hemophilia C
or Rosenthal syndrome. The incidence of CFXI is one of every one
million individuals, making it a rare blood disease (2). Although CFXI is inherited as an
autosomal recessive trait, some FXI mutations exhibit an
autosomal-dominant inheritance pattern. The FXI gene, responsible
for CFXI, is located on chromosome 4. Unlike hemophilia A or B,
which follows an X-linked inheritance, CFXI follows an autosomal
inheritance pattern. It differs from hemophilia A or B in that
affected patients show a variable bleeding tendency despite severe
deficiency (<20%). While spontaneous bleeding is rare,
individuals with CFXI may experience significant bleeding after
trauma or surgery (3).
The oral region is hyperfibrinolytic and more prone
to bleeding than other regions (4). There are few reports (5-8)
of surgical procedures being performed in the oral cavity of CFXI
patients. In the present report, we were able to perioperatively
perform multiple tooth extractions without inducing abnormal
bleeding by administering fresh frozen plasma (FFP) prior to
surgery and maintaining sufficient local hemostasis in patients
with CFXI.
Case presentation
The patient was a 43-year-old man with a height of
170 cm, weight of 90 kg and good nutrition. He had a history of
meniscal injury due to sports trauma. Prolonged activated partial
thromboplastin time (APTT) was observed during preoperative
assessment for meniscal injury and further evaluation by a
hematologist confirmed the diagnosis of CFXI. However, the patient
did not receive any treatment or follow-up for CFXI. A family
history investigation after establishing the diagnosis revealed
that the patient's father had CFXI. The patient's son was not
tested; hence, it was uncertain whether he also had CFXI. The
patient had a history of tooth extraction before the diagnosis of
CFXI was established, but there were no abnormal bleeding episodes.
The patient visited a referring physician with a chief concern of
chewing difficulty due to tooth mobility. Owing to severe
periodontal disease, teeth 721┴1235 and 721┬12 have been diagnosed
as requiring extraction. Considering the patient's history of CFXI
and the requirement to perform multiple extractions, a high risk of
bleeding was anticipated and the patient was referred to Kyoto
University Affiliated Hospital (Kyoto, Japan). During the initial
visit, subcutaneous bleeding or purpura were not observed in the
limbs or joints. Extraoral examination revealed symmetric facial
appearance, with no signs of subcutaneous bleeding or purpura.
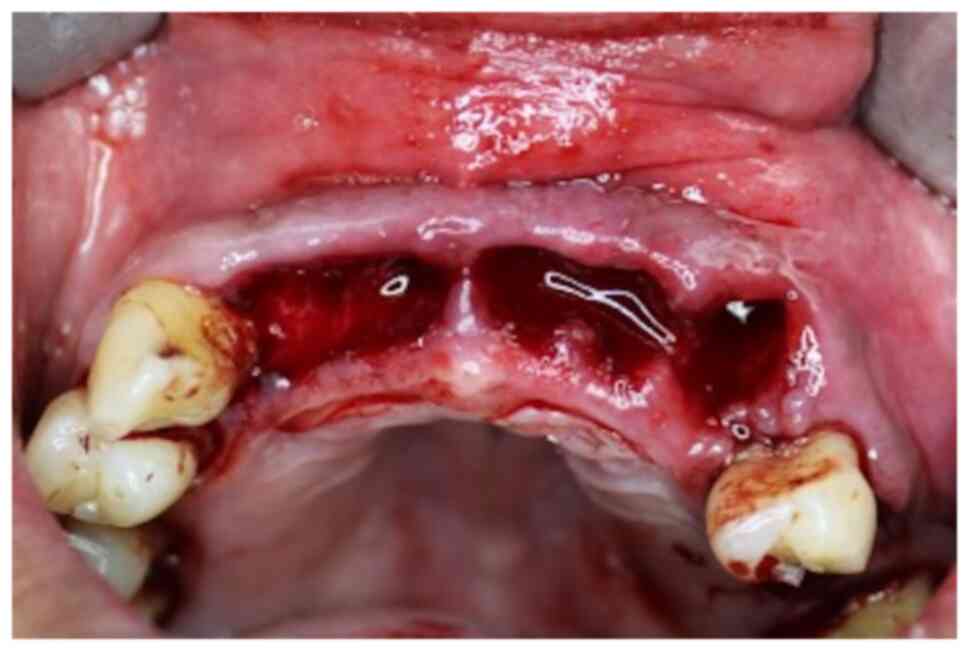
Intraoral examination revealed mobility of teeth 721┴1235 and
721┬12, as well as the presence of dental calculus. The gingiva
showed mild redness and swelling but no purpura or bleeding were
observed (Fig. 1). Panoramic
radiography findings showed horizontal bone resorption in the
mandible (Fig. 2). Blood test
results at the initial visit showed a white blood cell count of
5,400/µl, a red blood cell count of 530x104/µl and a
normal prothrombin time (PT) of 11.4 sec. The APTT was prolonged to
97.8 sec and the activity of FXI was <3%, indicating an abnormal
value. Factors II, V, VII, VIII, IX, X and XI levels were within
the normal range.
Prior to performing multiple tooth extractions, we
conferred with the hematologist and decided to perform an FFP
transfusion to replenish FXI. The maxillary teeth were extracted on
the 2nd day of admission and the mandibular teeth on the 4th day.
FFP was administered with 2 units each on the day before the
extraction and the day prior to that.
The extraction in the maxilla was first performed at
7┘. Infiltration anesthesia was applied with 2% xylocaine
(containing 1/80,000 epinephrine) and 7┘ extracted. The bleeding
was similar to that of a normal tooth extraction and the blood clot
was stable. Therefore, infiltration anesthesia to 21┴1235 was
applied in the same manner and the teeth extracted in order. Here
too, the bleeding was normal and blood clot retention was good. A
gelatin sponge (Spongel®) was placed in the extraction
socket, pressure hemostasis and suturing performed and a wound
protection splint we had prepared in advance attached (Fig. 3). Although we achieved sufficient
hemostasis, 1,000 mg of tranexamic acid (TXA) was required for
additional hemostasis. No postoperative bleeding was observed and
found that the blood clots were retained sufficiently on day 3 of
admission.
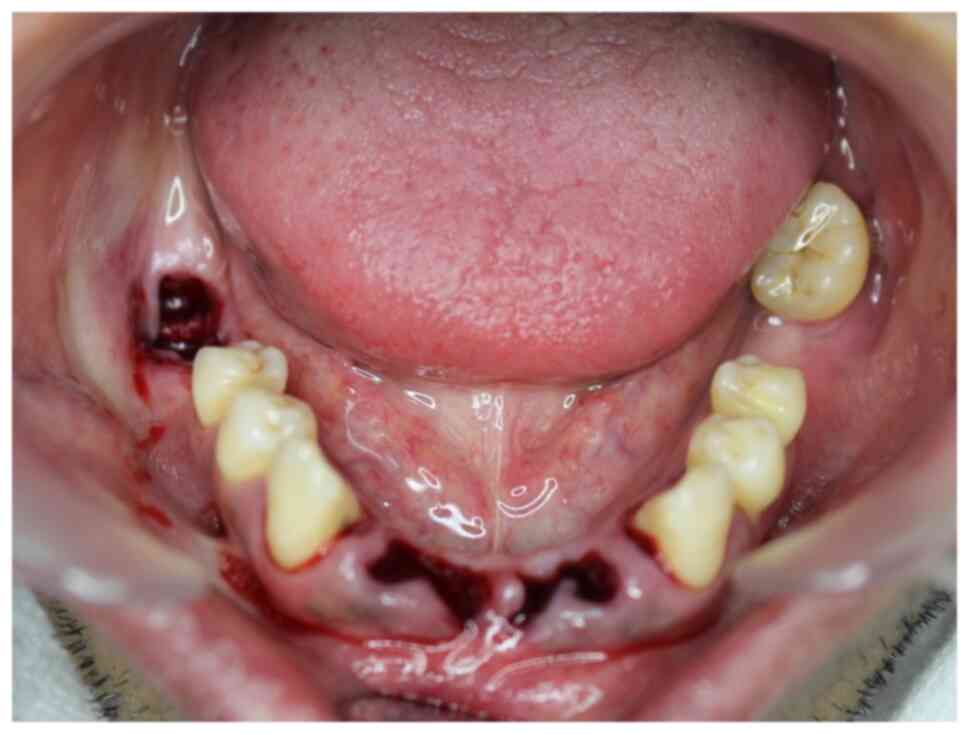
The extraction of tooth 7┐ was performed on the 4th
day of admission. The method of anesthesia, post-surgical bleeding
and clot retention was similar to the maxillary teeth. Considering
that hemostasis was possible, infiltration anesthesia was applied
to 21┬12 in the same manner and the teeth extracted. Since the
blood clot was well-retained, a gelatin sponge was not inserted
(Fig. 4). Instead, hemostasis was
achieved through coagulation using a carbon dioxide laser, sutures
placed and a wound protection splint attached. TXA was not
administered and postoperative bleeding was not observed. On day 5
of admission, a carbon dioxide laser was applied for tissue
activation. On the following day (day 6), the patient was
discharged because of good blood clot retention was good and no
postoperative bleeding.
To manage the wound protection splint hygienically,
the patient was instructed to gargle after meals and clean the
surface of the wound protection splint. After discharge, the wound
protection splint was to be worn for the entire day. The thread and
the splint were removed 7 days after each tooth extraction. There
was no abnormal bleeding or delayed healing postoperatively.
Discussion
CFXI is a rare disease that causes deficiency in
endogenous blood coagulation factor XI (a plasma thromboplastin
precursor) (9). CFXI rarely causes
spontaneous bleeding in patients with other coagulation factor
deficiencies, such as hemophilia A and B, but may cause major
bleeding after trauma or surgery (3). This is because platelet factor XI
-like activity is involved in the contact phase of endogenous
coagulation, which means that even if the activity of plasma factor
XI in CFXI patients is low, it becomes compensated for by platelet
factor-like activity and blood coagulates (10).
Bleeding is generally considered to occur easily in
the oral cavity, pharynx and genitourinary system, i.e., areas with
high fibrinolytic activity (4)
that fall within the range of oral surgical procedures. FFP
replacement therapy is generally used as a preventive and
therapeutic method to control bleeding due to factor deficiency and
has also been administered to CFXI patients in receiving oral and
maxillofacial surgery (5-8).
However, in clinical practice, it takes 2-5 days to
determine the test results of factor XI activity. This means that
it can be useful for preoperative evaluation but is not practical
as an index of perioperative bleeding. By monitoring the healing
process of patients who underwent FFP supplementation and local
hemostasis, it may be possible to reduce the amount of blood
transfused by supplementing with additional FFP when hemostasis is
difficult.
Hemostasis after tooth extraction includes filling
the extraction socket with cellulose oxide or collagen sponge,
suturing the wound edge and asking the patients to bite down on the
gauze for 20 to 30 min to stop bleeding by compression (11). In addition, the Food and Drug
Administration (FDA) describes the ‘coagulation of extraction
sites’ in the guidelines for using a dental laser during treatment
and irradiation with a carbon dioxide laser for coagulation after
tooth extraction as a recommended practice (12).
In the present case, considering that the effect of
coagulation was sustained due to the long half-life of FFP, 2 units
of FFP were administered before surgery and additional FFP added
when the hemostasis was insufficient even after applying local
hemostasis. For local hemostasis, the maxilla was filled with a
collagen sponge and sutured and the mandible was irradiated with a
carbon dioxide laser and sutured to ensure reduced perioperative
bleeding. TXA, an antifibrinolytic drug, is known to be very
effective in reducing bleeding (13), which is why it was administered
during the first maxillary tooth extraction when we did not know
the degree of bleeding. TXA was not administered when the
mandibular tooth was extracted because good hemostasis had been
achieved.
Previously, the timing of FFP use has varied in
patients with CFXI undergoing maxillofacial surgery (5-8)
(Table I). Gray et al
(5) reported that FFP was
administered preoperatively, intraoperatively and postoperatively
to treat multiple facial fractures without bleeding. Ilankovan
et al (6) reported the
administration of FFP pre-, intra- and post-operatively in
pharyngeal flap surgery, resulting in no postoperative bleeding. In
cases of Le Fort III osteotomy, where FFP was administered pre- and
intra-operatively but not post-operatively, they reported the
occurrence of a hematoma in the rib harvested for bone grafting.
Todd and Galbraith (7) reported
that while performing extraction and Le Fort I osteotomy and
sagittal split ramus osteotomy, FFP was administered pre- and
post-operatively with no bleeding. Data are scarce regarding oral
surgical procedures in patients with CFXI and future studies are
warranted to clarify the dosage and appropriate timing of
administering FFP. Poker et al (8) reported that a patient observed
significant hemorrhage after one week of continuous bleeding
following extraction of a mobile tooth at another hospital. A close
examination following a hemostatic procedure revealed that the
patient had CFXI. Furthermore, because hemostasis was difficult to
achieve, the extraction socket was filled with thrombin-soaked
cellulose oxide, closed with two intermittent polyvicryl sutures
and pressure was applied with a gauze pack to achieve hemostasis.
In the absence of special hemostatic measures during surgery in the
maxillofacial region in patients with CFXI, there may be persistent
or profuse bleeding after tooth extraction. Bleeding tendency of
patients with CFXI is generally considered mild, even in severe
deficiency and the bleeding phenotype does not correlate with FXI
activity level and even mild deficiency may result in bleeding
episodes (3).
 | Table ICongenital factor XI deficiency with
oral and maxillofacial surgery. |
Table I
Congenital factor XI deficiency with
oral and maxillofacial surgery.
| | FFP | |
|---|
| First author/s,
year | Age, years | Sex | Operation | Pre-op | Intra-op | Post-op | Hemostatic | History of
bleeding | Timing of diagnosis
of CFXI | (Refs.) |
|---|
| Ilankovan et
al, 1990 | 23 | Male | Le Fort III | + | + | - | - | Post-Ext
hemorrhage | Pre-ope exam | (6) |
| | | | pharyngoplasty | + | + | + | - | | | |
| Poker et al,
1990 | 50 | Male | Ext | - | - | - | Oxidized cellulose
soaked in topical thrombin | Post-tonsillectomy
hemorrhage Hematoma after appendicectomy post-Ext hemorrhage | Blood test to search
for the cause of bleeding | (8) |
| Gray et al,
1993 | 40 | Male | ORIF | + | + | + | - | - | Pre-ope exam | (5) |
| Todd et al and
Galbraith, 1993 | 16 | Female | Ext | + | - | + | - | Gingival bleeding
after toothbrush Scalp hematoma due to blunt head trauma | Pre-ope exam of
myringotomy tube placement | (7) |
| | | | Le Fort +SSRO | + | - | + | EACA | - | Pre-ope exam of
meniscal injury | |
| The present case,
2023 | 43 | Male | Ext | + | - | - | Gelatin sponge+ TX A
carbon dioxide laser | | | |
Information on patients with CFXI undergoing oral
maxillofacial surgery is currently limited. Although the use of
FFP, local hemostatic agents and monotherapy antifibrinolytic
therapy with TXA or ε-aminocaproic acid have been used for bleeding
management, there is no definitive evidence regarding their
effectiveness in reducing bleeding risk (3,5-8).
Furthermore, the optimal combination of these multiple hemostatic
agents has not been clearly established. Given the potential
variations due to surgical invasiveness, systematic reviews of case
series should be conducted to evaluate the efficacy of hemostatic
methods. When unexpected or unexplained bleeding occurs after
surgery or trauma, it is even more important to consider CFXI as a
possible cause. If preoperative test results show a prolonged APTT,
it may be necessary to consider coagulopathy to exclude or identify
CFXI deficiency.
In the present case, we hypothesized that by
supplementing FXI with FFP before surgery and by carefully
administering appropriate hemostatic procedures, we could safely
perform tooth extractions without supplementing FFP during and
after surgery and without persistent postoperative bleeding. This
is considered an important report for future data accumulation and
is, therefore, reported here.
CFXI may not be diagnosed during oral and
maxillofacial surgery but can become apparent after the surgery.
CFXI should be considered if there is an increase in ATPP during
the preoperative examination or abnormal bleeding during or after
surgery. Further, in patients who have already been diagnosed with
CFXI, preoperative FFP administration and appropriate local
hemostatic methods may reduce the risk of perioperative bleeding
and ensure patient safety. Since appropriate local hemostasis
appears to reduce the need for FFP, we have reported our results
with a review of the literature.
Acknowledgements
The authors would like to thank Dr Satomi Ueda
(Department of Hematology, Hirakata Kosai Hospital, Hirakata,
Japan) who contributed to patient treatment and care.
Funding
Funding: No funding was received.
Availability of data and materials
All data generated or analyzed during this study are
included in this published article.
Authors' contributions
TK acquired patient data, performed the literature
review and edited the manuscript. TK conceived and designed the
present study. MY, TW, SY, SF and KN acquired the data, provided
clinical advice and revised the manuscript. TK wrote the
manuscript. TK and MY confirm the authenticity of all the raw data.
All authors read and approved the final manuscript.
Ethics approval and consent to
participate
Not applicable.
Patient consent for publication
Written informed consent was obtained from the
patient for the publication of this case report and the
accompanying images.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Rosenthal RL, Dreski OH and Rosenthal N:
New hemophilia-like disease caused by deficiency of a third plasma
thromboplastin factor. Pros Soc Exp Biol Med. 82:171–174.
1953.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Mumford AD, Ackroyd S, Alikhan R, Bowles
L, Chowdary P, Grainger J, Mainwaring J, Mathias M and O'Connell N:
BCSH Committee. Guideline for the diagnosis and management of the
rare coagulation disorders: A United Kingdom Haemophilia Centre
Doctors' Organization guideline on behalf of the British Committee
for standards in Haematology. Br J Haematol. 167:304–326.
2014.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Lewandowska MD and Connors JM: Factor XI
deficiency. Hematol Oncol Clin North Am. 35:1157–1169.
2021.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Wheeler AP and Gailani D: Why factor XI
deficiency is a clinical concern. Expert Rev Hematol. 9:629–637.
2016.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Gray PB, Leen MM and Loftus MJ: Late
retrobulbar hemorrhage and blindness following malar fracture
complicated by factor XI deficiency. J Oral Maxillofac Surg.
51:699–702. 1993.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Ilankovan V, Blesing NE, Moos KF and
Davidson JF: Correction of facial deformities in patients with mild
bleeding disorders: A report of three cases. Br J Oral Maxillofac
Surg. 28:398–400. 1990.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Todd D and Galbraith D: Management of an
orthognathic surgery patient with factor XI deficiency: Review and
case report. J Oral Maxillofac Surg. 51:417–420. 1993.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Poker ID, Reade PC and Cook RM: Factor XI
deficiency disclosed following haemorrhage related to a dental
extraction. Brief review and case report. Aust Dent J. 35:258–260.
1990.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Emsley J, McEwan P and Gailani D:
Structure and function of factor XI. Blood. 115:2569–2577.
2010.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Tuszynski GP, Bevacqua SJ, Schmaier AH,
Colman RW and Walsh PN: Factor XI antigen and activity in human
platelets. Blood. 59:1148–1156. 1982.PubMed/NCBI
|
|
11
|
Perry DJ, Noakes TJC and Helliwell PS:
British Dental Society. Guidelines for the management of patients
on oral anticoagulants requiring dental surgery. Br Dent J.
203:389–393. 2007.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Sulewski JG: Clearing the FDA hurdle, from
initial device application through regulatory approval to the
clinical operatory: An update on dental laser marketing clearances.
J Laser Dent. 17:81–86. 2009.
|
|
13
|
Berliner S, Horowitz I, Martinowitz U,
Brenner B and Seligsohn U: Dental surgery in patients with severe
factor XI deficiency without plasma replacement. Blood Coagul
Fibrinolysis. 3:465–468. 1992.PubMed/NCBI
|