Cancer initiation and progression is a long and
complex biological phenomenon caused by any significant alterations
in the genome, proteome and chromatin or in any other cellular
levels. In total, 10-30% of breast cancer cases are genetically
inherited, 5-10% of cases are strongly correlated with hereditary
factors and nearly 5% of cases are caused by high penetrance gene
mutations such as BRCA1, BRCA2, TP53, CDH1, STK11 and
LKB1 (1,2). Among these high-penetrance genes,
BRCA1 and BRCA2 are the most crucial genes involved
in the regulation of DNA repair, transcription and the cell cycle.
Somatic/germline mutations in these two genes are associated with
breast cancer and are considered the strongest susceptibility
markers that have been identified, with a 45-80% life-time risk in
breast cancer in various ethnic and generalized population levels
(3-5). A number of these mutations are
largely from somatic cells and the majority are neutral/passenger
mutations, while certain mutations are more harmful (driver
mutations) and give specific cellular advantage, leading to cell
proliferation (6-8). Due to the increasing prevalence of
high-throughput next-generation sequencing (whole genome, exome and
targeted sequencing), the genomic information of thousands of
tumors from various cancer types can help researchers to identify
and characterize cancer samples in an easier and more robust way
(9-11). Besides, increasing the amount of
cancer sequencing data is also helpful to find ways to treat
patients using multiple approaches. One such approach is driver
gene mutation identification and treatment. To date, mutational
recurrence in patients is a highly reliable gene marker for driver
gene identification (12).
Most driver genes are cancer or subtype specific, so
identification of specific cancer drivers is an important step in
cancer therapy (13).
Additionally, these driver mutations lead to structural and
functional consequences that could lead to tumor heterogeneity and
drug resistance (14-16). Thus, identifying key driver
mutations is a prominent method for disease diagnosis and
management. However, identifying those key players is cumbersome
with insufficient tumor information (including low coverage and
sequence bias), a complex tumor microenvironment, intra/inter-tumor
heterogeneity and other biological issues (17). In recent years, several dedicated
cancer biology studies have made numerous notable contributions
including large cancer sequence depositories such as The Cancer
Genome Atlas (TCGA; https://portal.gdc.cancer.gov/), COSMIC database
(https://cancer.sanger.ac.uk/cosmic)
and International Cancer Genome Consortium (ICGC; https://icgc.org/), and several versatile sequence
analysis tools and servers (18). However, conventional treatments
and their outcomes are highly limited due to the diversity of
patient genome profiles (19,20). Hence, identification of
patient-specific treatment plans (precision oncology) is in urgent
need for cancer therapy (21,22).
A pharmacogenomics-based treatment strategy is the
most advanced and effective. Genetic testing (including DNA
sequencing technology) can identify specific mutational alterations
related to cancer, which is most likely to be helpful in the
development of a patient-specific treatment plan when the patient
does not respond to standard therapy. However, chemotherapeutic
agents with a narrow therapeutic window and adverse drug toxicities
are life-threatening (23).
Breast cancer targeted therapies generally target a specific gene
or protein and show an improved biological response to the disease
with minimal side effects. Precision cancer therapy makes clinical
decisions based on the identification of targets using
genomic/proteomics data (24).
Therefore, cancer treatment will be improved by increasing the
amount of tumor genomic data, including mutation, methylation and
expression data (25). One of
the standard precision oncology approaches is treating patients
with cancer based on subtyping (26). Besides, targeting the most
actionable, identified and reported driver gene mutations in
several cancer samples will help to treat patients in the new
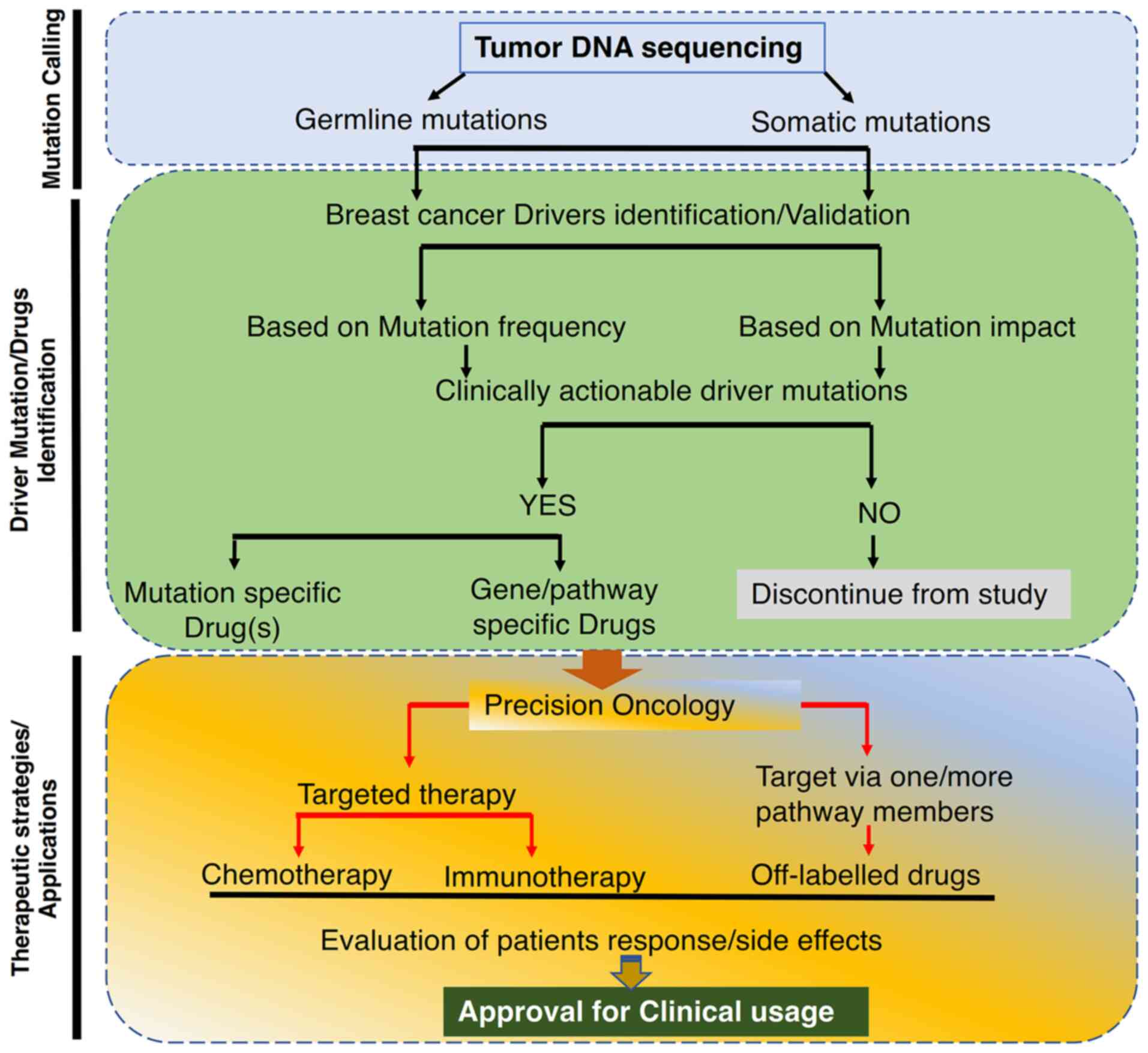
paradigm of breast cancer precision medicine (27-29). Furthermore, several additional
metrics are needed to further identify driver genes for
understanding precision oncology treatment (Fig. 1). In the present review, several
breast cancer-associated driver genes, existing strategies in
driver gene identification, actionable targets, various existing
challenges and applications of precision oncology in breast cancer
prognosis and treatment are covered.
The identification of breast cancer drivers is the
initial step in targeted therapy. Cancer driver identification
strategies are evolving, and several tools are being developed,
including sequence-based cancer driver prediction tools such as
MutSigCV (30), Mutation Set
Enrichment Analysis (31),
OncodriveFML (32),
OncodriveCLUST (33), MuSiC2
(34) and ActiveDriver (35) Similarly, several tools have been
developed to predict mutation consequences at the protein level
including Sorting Intolerant From Tolerant (SIFT) (36), Polymorphism Phenotyping v2
(PolyPhen-2) (37), CanDrA
(38), CHASM (39) and MutationAssessor (40). Several breast cancer drivers are
identified and classified based on their occurrence in cancer,
their histological and molecular functions and regulatory
properties (41). Most cancer
drivers have an oncogene, tumor suppressor or dual gene role
(42). Even a single mutation in
a driver gene may cause diverse effects and show differential
tumorigenic and drug response potentials in patients with cancer
(43).
Genome and proteome level data are screened for
mutations and their corresponding protein level impacts are
assessed using high-throughput technologies. However, only <10%
of mutations are actionable, hence targeting only actionable
mutations may not be beneficial in certain patients and thus lead
to a poor response to therapy (47). Several public oncogenomic
databases such as TCGA (48),
IGC and cBioportal (www.cbioportal.org) provide large scale multi-level
information that can be used in research to facilitate disease
prognosis, prevention and drug discovery (49). Several targetable breast cancer
mutations including oncogenic, truncating, amplifications and
fusions have been identified, and these mutations and their
corresponding U.S. Food and Drug Administration (FDA)-approved
drugs are listed in Table I and
detailed information about key gene mutations and targeted drugs
can be accessed using OncoKB, a data resource for precision
oncology (www.oncokb.org).
Trastuzumab is a widely tested drug against breast
cancer and understanding the action and resistance of this drug
will help to develop new viable therapeutic approaches (50). Several key pathways such as the
AKT, mTOR, PIK3CA and cell regulation pathways, and numerous
variants of tyrosine kinase receptors are targeted for drug
discovery and development. A study has demonstrated that the
resistance mechanism of trastuzumab is potentially caused by the
insulin-like growth factor I (IGF-1) receptor and mutation of IGF-1
shows a significant level of drug resistance against trastuzumab
(51). A high percentage of
somatic mutations in TP53, PI3KCA, PTEN and AKT have been
identified in breast cancer. Several large level mutational
landscape studies have paved the way to identify subgroup-specific
sensitivities in these pathways (52,53). Of the hotspot mutations
identified in the most commonly mutated gene, PIK3CA (~25%), 80-90%
of mutations occur in exon9 (E545K/E542K) and three hotspot
mutations occur in exon 20 (54).
Identification of DNA repair defects and their
mutational events could help to identify personalized treatment
strategies and targets. One such example is BRCA1/BRCA2
mutations or loss, which lead to deficiency in homologous
recombination and genomic instability (1,67). BRCA1 mutations are
proportionately higher in TNBC subtypes with several crucial gene
mutations considered to be a major risk in young women and crucial
for the scientific community for disease prevention and treatment
(68). Therefore, identifying
and characterizing BRCA1/2 functions and mutations may help
to design personalized approaches to treat patients with breast
cancer. Poly-(ADP ribose) polymerase 1 (PARP1) functions as a DNA
damage sensor for both single and double-stranded DNA breaks and
PARP2 is also responsible for base-excision DNA repair through homo
and heterodimerization with PARP1; thus, these two proteins play a
significant role in maintaining genomic stability through DNA
repair mechanisms (69,70). Deleterious mutations in
BRCA genes are highly sensitive to PARP1 inhibitors and DNA
alkylating agents (71). PARP1
inhibitors intensely reduce DNA single and double-stranded breaks
in BRCA1/2-deficient tumors, resulting in improved
sensitivity to DNA damaging agents such as cisplatin and PARP1
inhibitors, which are typically administered in BRCA
mutation-associated breast and ovarian cancer (72).
Trabectedin is another inhibitor recently approved
in Europe and North Korea for the treatment of soft tissue sarcomas
including breast, ovarian, prostate and other solid tumors.
Trabectedin functions by targeting the minor grooves of DNA,
bending the DNA toward the major grooves through which it increases
therapeutic efficiency by blocking transcription coupled nucleotide
excision repair machinery, leading to cell death (73-75). A previous study demonstrated that
the PARP1 inhibitor, olaparib, combined with cediranib potentially
inhibits homology-directed DNA repair via BRCA1/2 and
RAD51 downregulation and significantly improves
progression-free survival (76,77). A list of drugs used for DNA
repair defects at various levels of clinical trials are listed in
Table II (74,78-88). These inhibitors mainly target DNA
repair pathways in BRCA1/2 mutant/deficient breast
cancer.
Several breast and other cancer drivers can be
treated using different strategies, including combination therapy
(double or triple combination), by targeting more than one genetic
event (mutations/mutations plus copy number events or mutations
plus upregulation), which improves antitumor potential (89-91). The efficacy of immunotherapies
are tested with positive outcomes in both primary and metastatic
tumors and are the most potent alternatives to the cytotoxic chemo-
and radiotherapies (92).
Immunotherapy enhances both progression-free and overall survival
and prevents disease recurrence in patients with breast cancer by
targeting specific genes or pathways. Checkpoint inhibition is a
known approach used in cancer treatment, which targets certain
checkpoint molecules such as programmed cell death protein 1,
programmed death-ligand 1 (PD-L1) and CTLA4 (93,94). Atezolizumab is an FDA approved
PD-L1 antibody for the treatment of metastatic TNBC along with
other cancer types (95).
Trastuzumab is the first antibody used for the treatment of
metastatic breast cancer with a gene amplification or upregulation
of CD340 and HER2 (96). At
present, several anti-HER2 inhibitors including afatinib,
lapatinib, gefitinib and neratinib are used alone or in combination
with several monoclonal antibodies and chemotherapeutic agents
(97). A list of monoclonal
antibodies and combined treatments administered for several breast
cancer subtypes are listed in Table
SI (88,98-122). In recent years, resistance
against a number of monoclonal and combination therapies has been
observed, hence antibody-drug conjugates (ADCs) have been
established to overcome this drug resistance. A T-cell bispecific
antibodies approach and an ADC-based FDA-approved drug combination
(ado-trastuzumab emtansine) are the most constructive approaches
for the treatment of patients with breast cancer (123).
Overall, ~10% of mutations in breast cancer are
deemed actionable, highlighting a significant challenge in the
realm of precision oncology. Several vital factors determine tumor
growth, immune escape and survival. The T-cell response is the most
crucial for identifying tumor cells from the normal cell population
to produce antitumor immunity (124,125). This immunogenic potentials may
vary from one breast cancer subtype to another (126). Drug efficacy is influenced not
only by targeted genes but also by various factors, including
genetic variability, individual drug performance and mutations that
affect drug metabolism. For instance, cytochrome P450 (CYP) pathway
members (including CYP3A4, CYP19A and CYP2D6) have been associated
with metabolizing anticancer drugs (127). A recent study revealed that
HER2+ breast cancer is more responsive to immunotherapy,
but estrogen receptor-negative and HER2+ breast cancer
has more immunogenic potential (128). Higher expression of estrogen
may lower interferon-γ signaling and human leukocyte antigen gene
complex-II expression, which facilitates tumor escape from immune
action (129). Besides,
estrogens are known to be a risk factor for breast cancer by
enhancing several key oncogenic growth factors including EGF, IGF,
vascular endothelial growth factor, fibroblast growth factor and
their corresponding receptors. An estrogen-high tumor
microenvironment plays an important immunosuppressive role for the
survival of tumor cells in weak immunogenic tumor cells (98,130,131). Hence, targeting these genes and
their active mutations may improve breast cancer prognosis and
treatment. Similarly, the use of anti-estrogen therapies combined
with aromatase inhibitors could be a better approach to improve the
further response to immunotherapies (132).
The identification of somatic driver genes from
germline variants is a crucial step in genomic oncology. In
addition to several known germline variants, a growing number of
vital somatic variants are being identified. Those somatic variants
are validated through modern computational strategies and
functional annotation resources including SIFT (36), Polyphen-2 (37), CHASM (39), Mutation Assessor (40), DbNSFP (133) and Mutation Taster (134). However, recent developments in
high-throughput techniques and potential computational
resources/tools have resulted in very few mutations being
clinically actionable. There are major difficulties in
differentiating driver from passenger mutations, a lack of
strategies to validate genomic variants and challenges associating
the clinical relevance of these mutations. Apart from single
nucleotide polymorphism, several copy number variations, including
copy-number gains and amplifications, and copy-number loss have
been identified in breast cancer (135). BRCA1 is a well-known
tumor suppressor gene in breast cancer and identifying the key
driver genes in BRCA1-associated tumorigenesis will help to
predict the road map of this cancer type. In a public sequence
repository (cBioportal), ~80 BRCA1-mutated/deficient breast
cancer types were found, and the majority of mutations belong to
deleterious single nucleotide variations and copy number events,
including homozygous deletions or amplifications. Among these
mutations TP53 and MYC are the most commonly copy
number altered driver genes in BRCA1-associated
tumorigenesis and contributing to over 65 and 40% of cases
respectively, highlighting their significant roles in cancer
progression and potential for targeted therapies (136). The highest number of MYC
driver mutations identified in BRCA1-associated tumors was
in the TNBC subtype. Additionally, the amplification of MYC
along with the copy number amplification of PIK3CA and the
loss of copy number in RB1 and PTEN, supports
MYC amplification and promotes breast tumorigenesis
(137,138). However, due to a low number of
cases in this cohort, it is challenging to determine the outcomes
of these drivers.
Along with genomic data for the prediction of breast
cancer driver genes, mRNA expression data plays a crucial role in
predicting drivers in disease prognosis and their involvement in
the tumor microenvironment (139). A recent study revealed a list
of differentially expressed breast cancer driver genes to help
predict disease prognosis and overall survival (140). The mRNA expression levels of
the most enriched driver genes including DDX3X, BRD7, CCR7
and UBE2A are associated with a higher hazard ratio. Several
key breast cancer drivers, in conjunction with the tumor
microenvironment, significantly influence treatment response in
patients with breast cancer. These drivers are responsible for
tumor heterogeneity and for varied responses to drug (141). In precision oncology,
high-throughput sequencing data including genomics, transcriptomics
and proteomics data helps to predict the characteristics of
patients and the tumor behavior at the genome/proteome level. Tumor
heterogeneity is a prime cause for overall patient survival,
disease-free survival and response to chemo- or immunotherapy.
The identification of driver mutations has allowed
for new targeted therapeutic approaches in combination with
standard chemo- and immunotherapies in breast cancer. Existing
drugs for the identified actionable mutations in breast cancer are
also used to treat other cancer types; however, whether these drugs
are beneficial to other cancer types is still unclear. For example,
trastuzumab, which targets HER2 amplification/upregulation,
is beneficial to both breast and gastric cancer, while it shows no
significant results in lung and ovarian cancer (142,143). Even with the developing modern
applications in clinical trial design, challenges continue,
including tumor cellularity, intra- and inter-tumor heterogeneity
and the tumor microenvironment. Hence, identifying new strategies
to overcome these challenges and identifying new therapeutic
targets/biomarkers will help to improve the overall and
disease-free survival of patients through efficient breast cancer
medicine. The present review connects the current strategies with
future approaches for identifying novel breast cancer drivers,
aiming to aid researchers and ultimately benefit patients.
Differential drug responses among breast cancer subtypes influence
overall efficacy. Therefore, identifying new driver genes, novel
susceptibility regions or loci, and alternative pathways will
expedite the discovery of new therapeutic targets. The ultimate
goal of breast cancer precision oncology is to identify more
therapeutic targets and to increase the drug efficacy while
reducing toxicity for patients.
Not applicable.
WH and BKR designed this study. WH generated the
figure. BKR, WH, TP, JS, YZ, MMS and TC performed the background
research. BKR and WH drafted and revised the manuscript. All
authors contributed to editorial changes in the manuscript. All
authors have read and approved the final version of the manuscript.
Data authentication is not applicable.
Not applicable.
Not applicable.
The authors declare that they have no competing
interests.
Not applicable.
This research was supported by the Excellent Young Scientist
Foundation of Xinjiang Uyghur Autonomous Region of China (grant no.
2022D01E52) and the Natural Science Foundation of Xinjiang Uygur
Autonomous Region (grant no. 2023D01C39).
|
1
|
Harvey-Jones E, Raghunandan M,
Robbez-Masson L, Magraner-Pardo L, Alaguthurai T, Yablonovitch A,
Yen J, Xiao H, Brough R, Frankum J, et al: Longitudinal profiling
identifies co-occurring BRCA1/2 reversions, TP53BP1, RIF1 and
PAXIP1 mutations in PARP inhibitor resistant advanced breast
cancer. Ann Oncol. 35:364–380. 2024. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Waghela BN, Vaidya FU, Ranjan K, Chhipa
AS, Tiwari BS and Pathak C: AGE-RAGE synergy influences programmed
cell death signaling to promote cancer. Mol Cell Biochem.
476:585–598. 2021. View Article : Google Scholar
|
|
3
|
Ayers M, Lunceford J, Nebozhyn M, Murphy
E, Loboda A, Kaufman DR, Albright A, Cheng JD, Kang SP, Shankaran
V, et al: IFN-ү-related mRNA profile predicts clinical response to
PD-1 blockade. J Clin Invest. 127:2930–2940. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Bhaskaran SP, Huang T, Rajendran BK, Guo
M, Luo J, Qin Z, Zhao B, Chian J, Li S and Wang SM: Ethnic-specific
BRCA1/2 variation within Asia population: evidence from over 78 000
cancer and 40 000 non-cancer cases of Indian, Chinese, Korean and
Japanese populations. J Med Genet. 58:752–759. 2021. View Article : Google Scholar
|
|
5
|
Yuan H, Xiu L, Li N, Li Y, Wu L and Yao H:
PARPis response and outcome of ovarian cancer patients with BRCA1/2
germline mutation and a history of breast cancer. J Gynecol Oncol.
35:e512024. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Ranjan K and Pathak C: Expression of
cFLIPL Determines the Basal Interaction of Bcl-2 With Beclin-1 and
Regulates p53 Dependent Ubiquitination of Beclin-1 During
Autophagic Stress. J Cell Biochem. 117:1757–1768. 2016. View Article : Google Scholar
|
|
7
|
Ranjan K, Hedl M, Sinha S, Zhang X and
Abraham C: Ubiquitination of ATF6 by disease-associated RNF186
promotes the innate receptor-induced unfolded protein response. J
Clin Invest. 131:e1454722021. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Salvadores M and Supek F: Cell cycle gene
alterations associate with a redistribution of mutation risk across
chromosomal domains in human cancers. Nat Cancer. 5:330–346. 2024.
View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Xie F, Guo W, Wang X, Zhou K, Guo S, Liu
Y, Sun T, Li S, Xu Z, Yuan Q, et al: Mutational profiling of
mitochondrial DNA reveals an epithelial ovarian cancer-specific
evolutionary pattern contributing to high oxidative metabolism.
Clin Transl Med. 14:e15232024. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Zhu J, Yang J, Chen X, Wang Y, Wang X,
Zhao M, Li G, Wang Y, Zhu Y, Yan F, et al: Integrated Bulk and
Single-cell RNA sequencing data constructs and validates a
prognostic model for non-small cell lung cancer. J Cancer.
15:796–808. 2024. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Zhao H, Yu L and Wang L, Yin X, Liu K, Liu
W, Lin S and Wang L: Integrated analysis of single-cell and bulk
RNA sequencing data reveals immune-related lncRNA-mRNA prognostic
signature in triple-negative breast cancer. Genes Dis. 11:571–574.
2024. View Article : Google Scholar
|
|
12
|
Brown AL, Li M, Goncearenco A and
Panchenko AR: Finding driver mutations in cancer: Elucidating the
role of background mutational processes. PLoS Comput Biol.
15:e10069812019. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Li F, Gao L, Wang P and Hu Y: Identifying
cancer specific driver modules using a network-based method.
Molecules. 23:11142018. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Pala L, Sala I, Pagan E, De Pas T,
Zattarin E, Catania C, Cocorocchio E, Rossi G, Laszlo D, Ceresoli
G, et al: 'Heterogeneity of treatment effect on patients' long-term
outcome according to pathological response type in neoadjuvant RCTs
for breast cancer.'. Breast. 73:1036722024. View Article : Google Scholar
|
|
15
|
Schade E: A differentform for the
certification of cause of death. Ned Tijdschr Geneeskd.
130:2310–2312. 1986.In Dutch.
|
|
16
|
Dagogo-Jack I and Shaw AT: Tumour
heterogeneity and resistance to cancer therapies. Nat Rev Clin
Oncol. 15:81–94. 2018. View Article : Google Scholar
|
|
17
|
Akinpelu A, Akinsipe T, Avila LA, Arnold
RD and Mistriotis P: The impact of tumor microenvironment:
unraveling the role of physical cues in breast cancer progression.
Cancer Metastasis Rev. 43:823–844. 2024. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Pabinger S, Dander A, Fischer M, Snajder
R, Sperk M, Efremova M, Krabichler B, Speicher MR, Zschocke J and
Trajanoski Z: A survey of tools for variant analysis of
next-generation genome sequencing data. Brief Bioinform.
15:256–278. 2014. View Article : Google Scholar :
|
|
19
|
Phillips KA, Deverka PA, Sox HC, Khoury
MJ, Sandy LG, Ginsburg GS, Tunis SR, Orlando LA and Douglas MP:
Making genomic medicine evidence-based and patient-centered: A
structured review and landscape analysis of comparative
effectiveness research. Genet Med. 19:1081–1091. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Ranjan K, Hedl M and Abraham C: The E3
ubiquitin ligase RNF186 and RNF186 risk variants regulate innate
receptor-induced outcomes. Proc Natl Acad Sci USA.
118:e20135001182021. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Krebs K and Milani L: Translating
pharmacogenomics into clinical decisions: Do not let the perfect be
the enemy of the good. Hum Genomics. 13:392019. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Ding RB, Chen P, Rajendran BK, Lyu X, Wang
H, Bao J, Zeng J, Hao W, Sun H, Wong AH, et al: Molecular landscape
and subtype-specific therapeutic response of nasopharyngeal
carcinoma revealed by integrative pharmacogenomics. Nat Commun.
12:30462021. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Nain P, Seth L, Bell AS, Raval P, Sharma
G, Bethel M, Sharma G and Guha A: Chemotherapy in Pregnancy:
Assessing the safety of adriamycin administration in pregnancy
complicated by breast cancer. JACC Case Rep. 28:1021412023.
View Article : Google Scholar
|
|
24
|
Dey N, Williams C, Leyland-Jones B and De
P: Mutation matters in precision medicine: A future to believe in.
Cancer Treat Rev. 55:136–149. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Rajendran BK and Deng CX: A comprehensive
genomic meta-analysis identifies confirmatory role of OBSCN gene in
breast tumorigenesis. Oncotarget. 8:102263–102276. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Tsuchida J, Rothman J, McDonald KA,
Nagahashi M, Takabe K and Wakai T: Clinical target sequencing for
precision medicine of breast cancer. Int J Clin Oncol. 24:131–140.
2019. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Ramage KS, Lock A, White JM, Ekins MG,
Kiefel MJ, Avery VM and Davis RA: Semisynthesis and Cytotoxic
Evaluation of an Ether Analogue Library Based on a Polyhalogenated
Diphenyl Ether Scaffold Isolated from a Lamellodysidea Sponge. Mar
Drugs. 22:332024. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Hyman DM, Taylor BS and Baselga J:
Implementing Genome-Driven Oncology. Cell. 168:584–599. 2017.
View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Ranjan K and Pathak C: Expression of FADD
and cFLIPL balances mitochondrial integrity and redox signaling to
substantiate apoptotic cell death. Mol Cell Biochem. 422:135–150.
2016. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Lawrence MS, Stojanov P, Mermel CH,
Robinson JT, Garraway LA, Golub TR, Meyerson M, Gabriel SB, Lander
ES and Getz G: Discovery and saturation analysis of cancer genes
across 21 tumour types. Nature. 505:495–501. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Jia P, Wang Q, Chen Q, Hutchinson KE, Pao
W and Zhao Z: MSEA: Detection and quantification of mutation
hotspots through mutation set enrichment analysis. Genome Biol.
15:4892014. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Mularoni L, Sabarinathan R, Deu-Pons J,
Gonzalez-Perez A and Lopez-Bigas N: OncodriveFML: A general
framework to identify coding and non-coding regions with cancer
driver mutations. Genome Biol. 17:1282016. View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Tamborero D, Gonzalez-Perez A and
Lopez-Bigas N: OncodriveCLUST: Exploiting the positional clustering
of somatic mutations to identify cancer genes. Bioinformatics.
29:2238–2244. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Dees ND, Zhang Q, Kandoth C, Wendl MC,
Schierding W, Koboldt DC, Mooney TB, Callaway MB, Dooling D, Mardis
ER, et al: MuSiC: Identifying mutational significance in cancer
genomes. Genome Res. 22:1589–1598. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Reimand J and Bader GD: Systematic
analysis of somatic mutations in phosphorylation signaling predicts
novel cancer drivers. Mol Syst Biol. 9:6372013. View Article : Google Scholar : PubMed/NCBI
|
|
36
|
Ng PC and Henikoff S: Accounting for human
polymorphisms predicted to affect protein function. Genome Res.
12:436–446. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
37
|
Adzhubei I, Jordan DM and Sunyaev SR:
Predicting functional effect of human missense mutations using
PolyPhen-2. Curr Protoc Hum Genet Chapter. 7:Unit7 20. 2013.
|
|
38
|
Carter H, Douville C, Stenson PD, Cooper
DN and Karchin R: Identifying Mendelian disease genes with the
variant effect scoring tool. BMC Genomics. 14(Suppl 3): S32013.
View Article : Google Scholar : PubMed/NCBI
|
|
39
|
Wong WC, Kim D, Carter H, Diekhans M, Ryan
MC and Karchin R: CHASM and SNVBox: Toolkit for detecting
biologically important single nucleotide mutations in cancer.
Bioinformatics. 27:2147–2148. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
40
|
Reva B, Antipin Y and Sander C: Predicting
the functional impact of protein mutations: application to cancer
genomics. Nucleic Acids Res. 39:e1182011. View Article : Google Scholar : PubMed/NCBI
|
|
41
|
Rajendran BK and Deng CX: Characterization
of potential driver mutations involved in human breast cancer by
computational approaches. Oncotarget. 8:50252–50272. 2017.
View Article : Google Scholar : PubMed/NCBI
|
|
42
|
Shen L, Shi Q and Wang W: Double agents:
Genes with both oncogenic and tumor-suppressor functions.
Oncogenesis. 7:252018. View Article : Google Scholar : PubMed/NCBI
|
|
43
|
Dong X, Huang D, Yi X, Zhang S, Wang Z,
Yan B, Chung Sham P, Chen K and Jun Li M: Diversity spectrum
analysis identifies mutation-specific effects of cancer driver
genes. Commun Biol. 3:62020. View Article : Google Scholar : PubMed/NCBI
|
|
44
|
Zhao J, Cheng F and Zhao Z: SGDriver: A
novel structural genomics-based approach to prioritize cancer
related and potentially druggable somatic mutations. BMC
Bioinformatics. 16(suppl 15): P212015. View Article : Google Scholar :
|
|
45
|
Kamburov A, Lawrence MS, Polak P,
Leshchiner I, Lage K, Golub TR, Lander ES and Getz G: Comprehensive
assessment of cancer missense mutation clustering in protein
structures. Proc Natl Acad Sci USA. 112:E5486–E5495. 2015.
View Article : Google Scholar : PubMed/NCBI
|
|
46
|
Tokheim CJ, Papadopoulos N, Kinzler KW,
Vogelstein B and Karchin R: Evaluating the evaluation of cancer
driver genes. Proc Natl Acad Sci USA. 113:14330–14335. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
47
|
Ipe J, Swart M, Burgess KS and Skaar TC:
High-Throughput assays to assess the functional impact of genetic
variants: A road towards genomic-driven medicine. Clin Transl Sci.
10:67–77. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
48
|
Cancer Genome Atlas Research N, Weinstein
JN, Collisson EA, Mills GB, Shaw KR, Ozenberger BA, Ellrott K,
Shmulevich I, Sander C and Stuart JM: The Cancer Genome Atlas
Pan-Cancer analysis project. Nat Genet. 45:1113–1120. 2013.
View Article : Google Scholar
|
|
49
|
Leyens L, Reumann M, Malats N and Brand A:
Use of big data for drug development and for public and personal
health and care. Genet Epidemiol. 41:51–60. 2017. View Article : Google Scholar
|
|
50
|
Pierobon M, Ramos C, Wong S, Hodge KA,
Aldrich J, Byron S, Anthony SP, Robert NJ, Northfelt DW, Jahanzeb
M, et al: Enrichment of PI3K-AKT-mTOR pathway activation in hepatic
metastases from breast cancer. Clin Cancer Res. 23:4919–4928. 2017.
View Article : Google Scholar : PubMed/NCBI
|
|
51
|
Stratton MR, Campbell PJ and Futreal PA:
The cancer genome. Nature. 458:719–724. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
52
|
Cancer Genome Atlas Network: Comprehensive
molecular portraits of human breast tumours. Nature. 490:61–70.
2012. View Article : Google Scholar : PubMed/NCBI
|
|
53
|
Korkaya H and Wicha M: Reprogramming of
normal stem cells and cancer stem cells by the tumor
microenvironment. Nat Rev Cancer. 13:763–776. 2013.
|
|
54
|
Pipek O, Alpar D, Rusz O, Bodor C,
Udvarnoki Z, Medgyes-Horvath A, Csabai I, Szallasi Z, Madaras L,
Kahan Z, et al: Genomic Landscape of Normal and Breast Cancer
Tissues in a Hungarian Pilot Cohort. Int J Mol Sci. 24:85532023.
View Article : Google Scholar : PubMed/NCBI
|
|
55
|
Nakai K, Hung MC and Yamaguchi H: A
perspective on anti-EGFR therapies targeting triple-negative breast
cancer. Am J Cancer Res. 6:1609–1623. 2016.PubMed/NCBI
|
|
56
|
Zhao S, Ma Y, Liu L, Fang J, Ma H, Feng G,
Xie B, Zeng S, Chang J, Ren J, et al: Ningetinib plus gefitinib in
EGFR-mutant non-small-cell lung cancer with MET and AXL
dysregulations: A phase 1b clinical trial and biomarker analysis.
Lung Cancer. 188:1074682024. View Article : Google Scholar : PubMed/NCBI
|
|
57
|
Wu G, Chen Q, Lv D, Lin L and Huang J:
Pulmonary Adenocarcinoma Patient with Complex Mutations on EGFR
benefits from furmonertinib after acquiring gefitinib resistance: A
case report. Recent Pat Anticancer Drug Discov. 19:247–252. 2024.
View Article : Google Scholar : PubMed/NCBI
|
|
58
|
Lewis GD, Li G, Guo J, Yu SF, Fields CT,
Lee G, Zhang D, Dragovich PS, Pillow T, Wei B, et al: The
HER2-directed antibody-drug conjugate DHES0815A in advanced and/or
metastatic breast cancer: Preclinical characterization and phase 1
trial results. Nat Commun. 15:4662024. View Article : Google Scholar : PubMed/NCBI
|
|
59
|
Bose R, Kavuri SM, Searleman AC, Shen W,
Shen D, Koboldt DC, Monsey J, Goel N, Aronson AB, Li S, et al:
Activating HER2 mutations in HER2 gene amplification negative
breast cancer. Cancer Discov. 3:224–237. 2013. View Article : Google Scholar :
|
|
60
|
Rexer BN, Ghosh R, Na rasanna A, Estrada
MV, Chakrabarty A, Song Y, Engelman JA and Arteaga CL: Human breast
cancer cells harboring a gatekeeper T798M mutation in HER2
overexpress EGFR ligands and are sensitive to dual inhibition of
EGFR and HER2. Clin Cancer Res. 19:5390–5401. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
61
|
Ben-Baruch NE, Bose R, Kavuri SM, Ma CX
and Ellis MJ: HER2-Mutated Breast Cancer Responds to Treatment With
Single-Agent Neratinib, a Second-Generation HER2/EGFR Tyrosine
Kinase Inhibitor. J Natl Compr Canc Netw. 13:1061–1064. 2015.
View Article : Google Scholar : PubMed/NCBI
|
|
62
|
Hanker AB, Brewer MR, Sheehan JH, Koch JP,
Sliwoski GR, Nagy R, Lanman R, Berger MF, Hyman DM, Solit DB, et
al: An Acquired HER2(T798I) Gatekeeper Mutation Induces Resistance
to Neratinib in a Patient with HER2 mutant-driven breast cancer.
Cancer Discov. 7:575–585. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
63
|
Hyman DM, Piha-Paul SA, Won H, Rodon J,
Saura C, Shapiro GI, Juric D, Quinn DI, Moreno V, Doger B, et al:
HER kinase inhibition in patients with HER2- and HER3-mutant
cancers. Nature. 554:189–194. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
64
|
Savage P, Blanchet-Cohen A, Revil T,
Badescu D, Saleh SMI, Wang YC, Zuo D, Liu L, Bertos NR, Munoz-Ramos
V, et al: A Targetable EGFR-Dependent tumor-initiating program in
breast cancer. Cell Rep. 21:1140–1149. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
65
|
Herrera-Abreu MT, Palafox M, Asghar U,
Rivas MA, Cutts RJ, Garcia-Murillas I, Pearson A, Guzman M,
Rodriguez O, Grueso J, et al: Early Adaptation and Acquired
Resistance to CDK4/6 Inhibition in Estrogen Receptor-Positive
Breast Cancer. Cancer Res. 76:2301–2313. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
66
|
Condorelli R, Spring L, O'Shaughnessy J,
Lacroix L, Bailleux C, Scott V, Dubois J, Nagy RJ, Lanman RB,
Iafrate AJ, et al: Polyclonal RB1 mutations and acquired resistance
to CDK 4/6 inhibitors in patients with metastatic breast cancer.
Ann Oncol. 29:640–645. 2018. View Article : Google Scholar
|
|
67
|
Woodward ER, Lalloo F, Forde C, Pugh S,
Burghel GJ, Schlecht H, Harkness EF, Howell A, Howell SJ, Gandhi A
and Evans DG: Germline testing of BRCA1, BRCA2, PALB2 and CHEK2
c.1100delC in 1514 triple negative familial and isolated breast
cancers from a single centre, with extended testing of ATM, RAD51C
and RAD51D in over 400. J Med Genet. 61:385–391. 2023. View Article : Google Scholar : PubMed/NCBI
|
|
68
|
Belli C, Duso BA, Ferraro E and Curigliano
G: Homologous recombination deficiency in triple negative breast
cancer. Breast. 45:15–21. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
69
|
Miao K, Lei JH, Valecha MV, Zhang A, Xu J,
Wang L, Lyu X, Chen S, Miao Z, Zhang X, et al: NOTCH1 activation
compensates BRCA1 deficiency and promotes triple-negative breast
cancer formation. Nat Commun. 11:32562020. View Article : Google Scholar : PubMed/NCBI
|
|
70
|
McCann KE and Hurvitz SA: Advances in the
use of PARP inhibitor therapy for breast cancer. Drugs Context.
7:2125402018. View Article : Google Scholar : PubMed/NCBI
|
|
71
|
Caron MC, Sharma AK, O'Sullivan J, Myler
LR, Ferreira MT, Rodrigue A, Coulombe Y, Ethier C, Gagne JP,
Langelier MF, et al: Poly(ADP-ribose) polymerase-1 antagonizes DNA
resection at double-strand breaks. Nat Commun. 10:29542019.
View Article : Google Scholar : PubMed/NCBI
|
|
72
|
Bailly C, Thuru X and Quesnel B: Combined
cytotoxic chemotherapy and immunotherapy of cancer: Modern times.
NAR Cancer. 2:zcaa0022020. View Article : Google Scholar : PubMed/NCBI
|
|
73
|
van Kesteren Ch, de Vooght MM,
Lopez-Lazaro L, Mathot RA, Schellens JH, Jimeno JM and Beijnen JH:
Yondelis (trabectedin, ET-743): The development of an anticancer
agent of marine origin. Anticancer Drugs. 14:487–502. 2003.
View Article : Google Scholar : PubMed/NCBI
|
|
74
|
Zelek L, Yovine A, Brain E, Turpin F,
Taamma A, Riofrio M, Spielmann M, Jimeno J and Misset JL: A phase
II study of Yondelis (trabectedin, ET-743) as a 24-h continuous
intravenous infusion in pretreated advanced breast cancer. Br J
Cancer. 94:1610–1614. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
75
|
Le Cesne A, Martin-Broto J and Grignani G:
A review of the efficacy of trabectedin as second-line treatment of
advanced soft tissue sarcoma. Future Oncol. 18(30s): 5–11. 2022.
View Article : Google Scholar : PubMed/NCBI
|
|
76
|
Robson M, Im SA, Senkus E, Xu B, Domchek
SM, Masuda N, Delaloge S, Li W, Tung N, Armstrong A, et al:
Olaparib for metastatic breast cancer in patients with a Germline
BRCA Mutation. N Engl J Med. 377:523–533. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
77
|
Pujade-Lauraine E, Ledermann JA, Selle F,
Gebski V, Penson RT, Oza AM, Korach J, Huzarski T, Poveda A,
Pignata S, et al: Olaparib tablets as maintenance therapy in
patients with platinum-sensitive, relapsed ovarian cancer and a
BRCA1/2 mutation (SOLO2/ENGOT-Ov21): A double-blind, randomised,
placebo-controlled, phase 3 trial. Lancet Oncol. 18:1274–1284.
2017. View Article : Google Scholar : PubMed/NCBI
|
|
78
|
Kalra M, Tong Y, Jones DR, Walsh T, Danso
MA, Ma CX, Silverman P, King MC, Badve SS, Perkins SM and Miller
KD: Cisplatin +/− rucaparib after preoperative chemotherapy in
patients with triple-negative or BRCA mutated breast cancer. NPJ
Breast Cancer. 7:292021. View Article : Google Scholar
|
|
79
|
Kaplan AR, Gueble SE, Liu Y, Oeck S, Kim
H, Yun Z and Glazer PM: Cediranib suppresses homology-directed DNA
repair through down-regulation of BRCA1/2 and RAD51. Sci Transl
Med. 11:eaav45082019. View Article : Google Scholar : PubMed/NCBI
|
|
80
|
Telli ML, Jensen KC, Vinayak S, Kurian AW,
Lipson JA, Flaherty PJ, Timms K, Abkevich V, Schackmann EA, Wapnir
IL, et al: Phase II study of gemcitabine, carboplatin, and iniparib
as neoadjuvant therapy for triple-negative and BRCA1/2
mutation-associated breast cancer with assessment of a tumor-based
measure of genomic instability: PrECOG 0105. J Clin Oncol.
33:1895–1901. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
81
|
Shamseddine AI and Farhat FS:
Platinum-based compounds for the treatment of metastatic breast
cancer. Chemotherapy. 57:468–487. 2011. View Article : Google Scholar
|
|
82
|
Farmer H, McCabe N, Lord CJ, Tutt AN,
Johnson DA, Richardson TB, Santarosa M, Dillon KJ, Hickson I,
Knights C, et al: Targeting the DNA repair defect in BRCA mutant
cells as a therapeutic strategy. Nature. 434:917–921. 2005.
View Article : Google Scholar : PubMed/NCBI
|
|
83
|
Bryant HE, Schultz N, Thomas HD, Parker
KM, Flower D, Lopez E, Kyle S, Meuth M, Curtin NJ and Helleday T:
Specific killing of BRCA2-deficient tumours with inhibitors of
poly(ADP-ribose) polymerase. Nature. 434:913–917. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
84
|
Hyams DM, Chan A, de Oliveira C, Snyder R,
Vinholes J, Audeh MW, Alencar VM, Lombard J, Mookerjee B, Xu J, et
al: Cediranib in combination with fulvestrant in hormone-sensitive
metastatic breast cancer: A randomized Phase II study. Invest New
Drugs. 31:1345–1354. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
85
|
Litton JK, Rugo HS, Ettl J, Hurvitz SA,
Goncalves A, Lee KH, Fehrenbacher L, Yerushalmi R, Mina LA, Martin
M, et al: Talazoparib in patients with advanced breast cancer and a
germline BRCA Mutation. N Engl J Med. 379:753–763. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
86
|
Ettl J, Quek RGW, Lee KH, Rugo HS, Hurvitz
S, Goncalves A, Fehrenbacher L, Yerushalmi R, Mina LA, Martin M, et
al: Quality of life with talazoparib versus physician's choice of
chemotherapy in patients with advanced breast cancer and germline
BRCA1/2 mutation: patient-reported outcomes from the EMBRACA phase
III trial. Ann Oncol. 29:1939–1947. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
87
|
Bindra RS, Gibson SL, Meng A, Westermark
U, Jasin M, Pierce AJ, Bristow RG, Classon MK and Glazer PM:
Hypoxia-induced down-regulation of BRCA1 expression by E2Fs. Cancer
Res. 65:11597–11604. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
88
|
Kumar M, Ranjan K, Singh V, Pathak C,
Pappachan A and Singh DD: Hydrophilic Acylated Surface Protein A
(HASPA) of Leishmania donovani: Expression, Purification and
Biophysico-Chemical Characterization. Protein J. 36:343–351. 2017.
View Article : Google Scholar : PubMed/NCBI
|
|
89
|
Liu ZB, Zhang L, Bian J and Jian J:
Combination strategies of checkpoint immunotherapy in metastatic
breast cancer. Onco Targets Ther. 13:2657–2666. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
90
|
Kroemer G and Zitvogel L: Cancer
immunotherapy in 2017: The breakthrough of the microbiota. Nat Rev
Immunol. 18:87–88. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
91
|
Emens LA, Ascierto PA, Darcy PK, Demaria
S, Eggermont AMM, Redmond WL, Seliger B and Marincola FM: Cancer
immunotherapy: Opportunities and challenges in the rapidly evolving
clinical landscape. Eur J Cancer. 81:116–129. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
92
|
Wang Y, Xu Z, Wu KL, Yu L, Wang C, Ding H,
Gao Y, Sun H, Wu YH, Xia M, et al: Siglec-15/sialic acid axis as a
central glyco-immune checkpoint in breast cancer bone metastasis.
Proc Natl Acad Sci USA. 121:e23129291212024. View Article : Google Scholar : PubMed/NCBI
|
|
93
|
Krasniqi E, Barchiesi G, Pizzuti L,
Mazzotta M, Venuti A, Maugeri-Sacca M, Sanguineti G, Massimiani G,
Sergi D, Carpano S, et al: Immunotherapy in HER2-positive breast
cancer: state of the art and future perspectives. J Hematol Oncol.
12:1112019. View Article : Google Scholar : PubMed/NCBI
|
|
94
|
Pardoll DM: The blockade of immune
checkpoints in cancer immunotherapy. Nat Rev Cancer. 12:252–264.
2012. View Article : Google Scholar : PubMed/NCBI
|
|
95
|
Sharmni Vishnu K, Win TT, Aye SN and
Basavaraj AK: Combined atezolizumab and nab-paclitaxel in the
treatment of triple negative breast cancer: A meta-analysis on
their efficacy and safety. BMC Cancer. 22:11392022. View Article : Google Scholar : PubMed/NCBI
|
|
96
|
Darvin P, Toor SM, Sasidharan Nair V and
Elkord E: Immune checkpoint inhibitors: Recent progress and
potential biomarkers. Exp Mol Med. 50:1–11. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
97
|
Garcia-Aranda M and Redondo M:
Immunotherapy: A challenge of breast cancer treatment. Cancers
(Basel). 11:18222019. View Article : Google Scholar : PubMed/NCBI
|
|
98
|
Garcia-Aranda M and Redondo M: Protein
kinase targets in breast cancer. Int J Mol Sci. 18:25432017.
View Article : Google Scholar : PubMed/NCBI
|
|
99
|
Treilleux I, Blay JY, Bendriss-Vermare N,
Ray-Coquard I, Bachelot T, Guastalla JP, Bremond A, Goddard S, Pin
JJ, Barthelemy-Dubois C and Lebecque S: Dendritic cell infiltration
and prognosis of early stage breast cancer. Clin Cancer Res.
10:7466–7474. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
100
|
Bates GJ, Fox SB, Han C, Leek RD, Garcia
JF, Harris AL and Banham AH: Quantification of regulatory T cells
enables the identification of high-risk breast cancer patients and
those at risk of late relapse. J Clin Oncol. 24:5373–5380. 2006.
View Article : Google Scholar : PubMed/NCBI
|
|
101
|
Gobert M, Treilleux I, Bendriss-Vermare N,
Bachelot T, Goddard-Leon S, Arfi V, Biota C, Doffin AC, Durand I,
Olive D, et al: Regulatory T cells recruited through CCL22/CCR4 are
selectively activated in lymphoid infiltrates surrounding primary
breast tumors and lead to an adverse clinical outcome. Cancer Res.
69:2000–2009. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
102
|
Mackall CL, Fleisher TA, Brown MR, Magrath
IT, Shad AT, Horowitz ME, Wexler LH, Adde MA, McClure LL and Gress
RE: Lymphocyte depletion during treatment with intensive
chemotherapy for cancer. Blood. 84:2221–2228. 1994. View Article : Google Scholar : PubMed/NCBI
|
|
103
|
Guckel B, Stumm S, Rentzsch C, Marme A,
Mannhardt G and Wallwiener D: A CD80-transfected human breast
cancer cell variant induces HER-2/neu-specific T cells in
HLA-A*02-matched situations in vitro as well as in vivo. Cancer
Immunol Immunother. 54:129–140. 2005. View Article : Google Scholar
|
|
104
|
Morse MA, Chaudhry A, Gabitzsch ES,
Hobeika AC, Osada T, Clay TM, Amalfitano A, Burnett BK, Devi GR,
Hsu DS, et al: Novel adenoviral vector induces T-cell responses
despite anti-adenoviral neutralizing antibodies in colorectal
cancer patients. Cancer Immunol Immunother. 62:1293–1301. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
105
|
Kouloulias VE, Dardoufas CE, Kouvaris JR,
Gennatas CS, Polyzos AK, Gogas HJ, Sandilos PH, Uzunoglu NK, Malas
EG and Vlahos LJ: Liposomal doxorubicin in conjunction with
reirradiation and local hyperthermia treatment in recurrent breast
cancer: A phase I/II trial. Clin Cancer Res. 8:374–382.
2002.PubMed/NCBI
|
|
106
|
Morse MA, Hobeika AC, Osada T, Serra D,
Niedzwiecki D, Lyerly HK and Clay TM: Depletion of human regulatory
T cells specifically enhances antigen-specific immune responses to
cancer vaccines. Blood. 112:610–618. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
107
|
Meredith R, Torgue J, Shen S, Fisher DR,
Banaga E, Bunch P, Morgan D, Fan J and Straughn JM Jr: Dose
escalation and dosimetry of first-in-human α radioimmunotherapy
with 212Pb-TCMC-trastuzumab. J Nucl Med. 55:1636–1642. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
108
|
Bernal-Estevez DA, Garcia O, Sanchez R and
Parra-Lopez CA: Monitoring the responsiveness of T and antigen
presenting cell compartments in breast cancer patients is useful to
predict clinical tumor response to neoadjuvant chemotherapy. BMC
Cancer. 18:772018. View Article : Google Scholar : PubMed/NCBI
|
|
109
|
Wiseman C, Presant C, Rao R and Smith J:
Clinical responses to intralymphatic whole-cell melanoma vaccine
augmented by in vitro incubation with alpha-interferon. Ann N Y
Acad Sci. 690:388–391. 1993. View Article : Google Scholar : PubMed/NCBI
|
|
110
|
Rosenberg SA, Yang JC, Sherry RM, Kammula
US, Hughes MS, Phan GQ, Citrin DE, Restifo NP, Robbins PF,
Wunderlich JR, et al: Durable complete responses in heavily
pretreated patients with metastatic melanoma using T-cell transfer
immunotherapy. Clin Cancer Res. 17:4550–4557. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
111
|
Adams S, Kozhaya L, Martiniuk F, Meng TC,
Chiriboga L, Liebes L, Hochman T, Shuman N, Axelrod D, Speyer J, et
al: Topical TLR7 agonist imiquimod can induce immune-mediated
rejection of skipn metastases in patients with breast cancer. Clin
Cancer Res. 18:6748–6757. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
112
|
Czerniecki BJ, Koski GK, Koldovsky U, Xu
S, Cohen PA, Mick R, Nisenbaum H, Pasha T, Xu M, Fox KR, et al:
Targeting HER-2/neu in early breast cancer development using
dendritic cells with staged interleukin-12 burst secretion. Cancer
Res. 67:1842–1852. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
113
|
Koski GK, Koldovsky U, Xu S, Mick R,
Sharma A, Fitzpatrick E, Weinstein S, Nisenbaum H, Levine BL, Fox
K, et al: A novel dendritic cell-based immunization approach for
the induction of durable Th1-polarized anti-HER-2/neu responses in
women with early breast cancer. J Immunother. 35:54–65. 2012.
View Article : Google Scholar
|
|
114
|
Sharma A, Koldovsky U, Xu S, Mick R, Roses
R, Fitzpatrick E, Weinstein S, Nisenbaum H, Levine BL, Fox K, et
al: HER-2 pulsed dendritic cell vaccine can eliminate HER-2
expression and impact ductal carcinoma in situ. Cancer.
118:4354–4362. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
115
|
Garnett CT, Schlom J and Hodge JW:
Combination of docetaxel and recombinant vaccine enhances T-cell
responses and antitumor activity: Effects of docetaxel on immune
enhancement. Clin Cancer Res. 14:3536–3544. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
116
|
Mohebtash M, Tsang KY, Madan RA, Huen NY,
Poole DJ, Jochems C, Jones J, Ferrara T, Heery CR, Arlen PM, et al:
A pilot study of MUC-1/CEA/TRICOM poxviral-based vaccine in
patients with metastatic breast and ovarian cancer. Clin Cancer
Res. 17:7164–7173. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
117
|
Hodge JW, Sabzevari H, Yafal AG, Gritz L,
Lorenz MG and Schlom J: A triad of costimulatory molecules
synergize to amplify T-cell activation. Cancer Res. 59:5800–5807.
1999.PubMed/NCBI
|
|
118
|
Berinstein NL, Karkada M, Morse MA,
Nemunaitis JJ, Chatta G, Kaufman H, Odunsi K, Nigam R, Sammatur L,
MacDonald LD, et al: First-in-man application of a novel
therapeutic cancer vaccine formulation with the capacity to induce
multi-functional T cell responses in ovarian, breast and prostate
cancer patients. J Transl Med. 10:1562012. View Article : Google Scholar : PubMed/NCBI
|
|
119
|
Robbins PF, Eggensperger D, Qi CF and
Schlom J: Definition of the expression of the human
carcinoembryonic antigen and non-specific cross-reacting antigen in
human breast and lung carcinomas. Int J Cancer. 53:892–897. 1993.
View Article : Google Scholar : PubMed/NCBI
|
|
120
|
Madan RA, Arlen PM and Gulley JL:
PANVAC-VF: poxviral-based vaccine therapy targeting CEA and MUC1 in
carcinoma. Expert Opin Biol Ther. 7:543–554. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
121
|
Kwa M, Li X, Novik Y, Oratz R, Jhaveri K,
Wu J, Gu P, Meyers M, Muggia F, Speyer J, et al: Serial
immunological parameters in a phase II trial of exemestane and
low-dose oral cyclophosphamide in advanced hormone
receptor-positive breast cancer. Breast Cancer Res Treat.
168:57–67. 2018. View Article : Google Scholar
|
|
122
|
Rios-Doria J, Durham N, Wetzel L,
Rothstein R, Chesebrough J, Holoweckyj N, Zhao W, Leow CC and
Hollingsworth R: Doxil synergizes with cancer immunotherapies to
enhance antitumor responses in syngeneic mouse models. Neoplasia.
17:661–670. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
123
|
Nejadmoghaddam MR, Minai-Tehrani A,
Ghahremanzadeh R, Mahmoudi M, Dinarvand R and Zarnani AH:
Antibody-Drug Conjugates: Possibilities and Challenges. Avicenna J
Med Biotechnol. 11:3–23. 2019.PubMed/NCBI
|
|
124
|
Vonderheide RH, Domchek SM and Clark AS:
Immunotherapy for breast cancer: What are we missing? Clin Cancer
Res. 23:2640–2646. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
125
|
Zhang X, Kim S, Hundal J, Herndon JM, Li
S, Petti AA, Soysal SD, Li L, McLellan MD, Hoog J, et al: Breast
cancer neoantigens can induce CD8(+) T-Cell responses and antitumor
immunity. Cancer Immunol Res. 5:516–523. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
126
|
Ayoub NM, Al-Shami KM and Yaghan RJ:
Immunotherapy for HER2-positive breast cancer: recent advances and
combination therapeutic approaches. Breast Cancer (Dove Med Press).
11:53–69. 2019.PubMed/NCBI
|
|
127
|
Olopade OI, Grushko TA, Nanda R and Huo D:
Advances in breast cancer: Pathways to personalized medicine. Clin
Cancer Res. 14:7988–7999. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
128
|
Uma K and Jan FS: HER2 in breast cancer: A
review and update. Adv Anat Pathol. 21:100–107. 2014. View Article : Google Scholar
|
|
129
|
Mostafa AA, Codner D, Hirasawa K, Komatsu
Y, Young MN, Steimle V and Drover S: Activation of ERα signaling
differentially modulates IFN-ү induced HLA-class II expression in
breast cancer cells. PLoS One. 9:e873772014. View Article : Google Scholar
|
|
130
|
Rothenberger NJ, Somasundaram A and
Stabile LP: The role of the estrogen pathway in the tumor
microenvironment. Int J Mol Sci. 19:6112018. View Article : Google Scholar : PubMed/NCBI
|
|
131
|
Makhoul I, Atiq M, Alwbari A and
Kieber-Emmons T: Breast cancer immunotherapy: An update. Breast
Cancer (Auckl). 12:11782234187748022018. View Article : Google Scholar : PubMed/NCBI
|
|
132
|
Johnston SR, Martin LA, Leary A, Head J
and Dowsett M: Clinical strategies for rationale combinations of
aromatase inhibitors with novel therapies for breast cancer. J
Steroid Biochem Mol Biol. 106:180–186. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
133
|
Liu X, Li C, Mou C, Dong Y and Tu Y:
dbNSFP v4: A comprehensive database of transcript-specific
functional predictions and annotations for human nonsynonymous and
splice-site SNVs. Genome Med. 12:1032020. View Article : Google Scholar : PubMed/NCBI
|
|
134
|
Steinhaus R, Proft S, Schuelke M, Cooper
DN, Schwarz JM and Seelow D: MutationTaster2021. Nucleic Acids Res.
49(W1): W446–W451. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
135
|
Shahrouzi P, Forouz F, Mathelier A,
Kristensen VN and Duijf PHG: Copy number alterations: A
catastrophic orchestration of the breast cancer genome. Trends Mol
Med. 30:750–764. 2024. View Article : Google Scholar : PubMed/NCBI
|
|
136
|
Annunziato S, de Ruiter JR, Henneman L,
Brambillasca CS, Lutz C, Vaillant F, Ferrante F, Drenth AP, van der
Burg E, Siteur B, et al: Comparative oncogenomics identifies
combinations of driver genes and drug targets in BRCA1-mutated
breast cancer. Nat Commun. 10:3972019. View Article : Google Scholar : PubMed/NCBI
|
|
137
|
Kaysudu I, Gungul TB, Atici S, Yilmaz S,
Bayram E, Guven G, Cizmecioglu NT, Sahin O, Yesiloz G, Haznedaroglu
BZ and Cizmecioglu O: Cholesterol biogenesis is a PTEN-dependent
actionable node for the treatment of endocrine therapy-refractory
cancers. Cancer Sci. 114:4365–4375. 2023. View Article : Google Scholar : PubMed/NCBI
|
|
138
|
Lu Y, Dong K, Yang M and Liu J: Network
pharmacology-based strategy to investigate the bioactive
ingredients and molecular mechanism of Evodia rutaecarpa in
colorectal cancer. BMC Complement Med Ther. 23:4332023. View Article : Google Scholar : PubMed/NCBI
|
|
139
|
Pranav P, Palaniyandi T, Baskar G, Ravi M,
Rajendran BK, Sivaji A and Ranganathan M: Gene expressions and
their significance in organoid cultures obtained from breast cancer
patient-derived biopsies. Acta Histochem. 124:1519102022.
View Article : Google Scholar : PubMed/NCBI
|
|
140
|
Du XW, Li G, Liu J, Zhang CY, Liu Q, Wang
H and Chen TS: Comprehensive analysis of the cancer driver genes in
breast cancer demonstrates their roles in cancer prognosis and
tumor microenvironment. World J Surg Oncol. 19:2732021. View Article : Google Scholar : PubMed/NCBI
|
|
141
|
Liu X, Jin G, Qian J, Yang H, Tang H, Meng
X and Li Y: Digital gene expression profiling analysis and its
application in the identification of genes associated with improved
response to neoadjuvant chemotherapy in breast cancer. World J Surg
Oncol. 16:822018. View Article : Google Scholar : PubMed/NCBI
|
|
142
|
Martin V, Cappuzzo F, Mazzucchelli L and
Frattini M: HER2 in solid tumors: More than 10 years under the
microscope; where are we now? Future Oncol. 10:1469–1486. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
143
|
Slamon DJ, Leyland-Jones B, Shak S, Fuchs
H, Paton V, Bajamonde A, Fleming T, Eiermann W, Wolter J, Pegram M,
et al: Use of chemotherapy plus a monoclonal antibody against HER2
for metastatic breast cancer that overexpresses HER2. N Engl J Med.
344:783–792. 2001. View Article : Google Scholar : PubMed/NCBI
|