Introduction
Pancreatic cancer has the worst prognosis of all the
major types of cancers and it is the fourth leading cause of cancer
death (1). The survival ratio of 5
years in pancreatic cancer approximates 5% (2). This miserable lethality is caused by
the difficulty of diagnosis at an early operable stage and the
aggressiveness of the cancer cells (3,4).
Even if it is diagnosed at an early stage and resected curatively,
there is still a high incidence of recurrence (1). Gemcitabine (GEM)-based chemotherapy
is the established core of multimodal therapy for pancreatic cancer
(5). However, it is rarely
curative and only modestly effective against tumor recurrence. We
need to focus on the recurrence mechanism which is related to
biological cancer cell features, such as high invasiveness and
migration and find a novel biomarker which could predict the
prognosis in clinical situation.
Pancreatic cancer originates from pancreatic ductal
epithelium and acquires the characteristics of mesenchymal cells of
invading and the metastasizing process. It suggests the existence
of epithelial-mesenchymal transition (EMT) during cancer
progression (6). The phenomenon of
EMT was originally identified during an early embryonic development
program in which cells migrate to and colonize different embryonic
territories (7). Subsequently, EMT
was reported as a similar situation in which cancer cells progress
and invade into lymphatic tubes and microvessels (8) and it was shown to be a crucial event
during cancer progression and metastasis (9,10).
Tumor cancer cells that undergo EMT show reduced intercellular
adhesion with decreased expression of E-cadherin and translocation
of β-catenin from cell membrane to the nuclei, and obtain
fibroblast-like properties with increased mesenchymal marker
expression, such as fibronectin, vimentin and N-cadherin. EMT leads
to increased migratory and invasive properties and facilitates
metastasis (8–12). Especially in pancreatic cancer, it
has been reported that pancreatic cancer cells undergo EMT at an
early stage, such as PanIN (pancreatic intraepithelial neoplasia)
stage which is the precursor cancer lesion (13). It was demonstrated that cancer
cells had already spread into the liver as a micrometastasis at a
PanIN stage in vivo analysis. The high levels of invasive
and migratory abilities were proven in pancreatic cancer (13).
EMT requires the expression of various kinds of
regulators such as members of the Zeb, Snail and Twist
transcription factor families (14–16).
Moreover, EMT phenomenon is plastic and the totally reverse
phenomenon to EMT, namely MET (mesenchymal-epithelial transition),
is essential for regrowing at metastatic sites (17). It suggests that EMT programs are
regulated by some epigenome. Recently a novel pathway that
elucidates EMT mechanism induced by transforming growth factor-β
(TGF-β) was reported (18). The
authors demonstrated that TGF-β stimulated Sox4 expression, which
induced the histone methyltransferase, Ezh2 and reprogramed the
epigenome to induce EMT programs. Sox4 regulated existing EMT
inducers such as Zeb, Snail and Twist, acting upstream as a master
regulator. In addition, other reports have shown that restoration
of miR-335 expression interfered with Sox4 expression, suppressing
lung and bone metastasis (19)
(Fig. 1).
To date, however, no study has clarified the
importance of this Sox4/Ezh2 axis in clinical samples of pancreatic
cancer. The expression of Sox4 and Ezh2 could predict the
possibility of cancer metastasis and recurrence. Therefore, we
evaluated the prognostic significance of Sox4/Ezh2 axis and
expression of miR-335 regarding the clinical outcomes of 36
patients with pancreatic cancer in the present study.
Materials and methods
Study on primary tumor samples
Between March 2007 and October 2012, 92 patients
underwent surgery for pancreatic cancer at Osaka University
Hospital, Osaka, Japan. Among the patients, 36 consecutive patients
who underwent curative resection (R0) with histologically clear
margins with no preoperative therapy were enrolled in the present
study. The patients were staged before and after surgery according
to the criteria of the International Union Against Cancer (UICC).
The median follow-up period was 26.4 months (range, 3.8–79.7
months), the 5-year survival rate was 29.0% and recurrence of the
disease was observed in 19 patients. GEM was administered in 21
patients as an adjuvant chemotherapy (1000 mg/m2, 3
times/month for 6 months). No radiation therapy was performed
during the follow-up period. Table
I summarizes the characteristics of the 36 patients. The use of
resected samples was approved by the Human Ethics Review Committee
of the Graduate School of Medicine, Osaka University (approval
number 08226). The meaning of this study was explained to each
patient and written informed consent was obtained from all patients
included in the study.
 | Table IClinicopathological characteristics
of the 36 patients. |
Table I
Clinicopathological characteristics
of the 36 patients.
|
Characteristics | Data |
|---|
| Age (years) | 68.5±9.4 |
| Gender
(Male/female) | 21/15 |
| Location
(Ph/Pb/Pt) | 10/21/5 |
| Lymphatic invasion
(+/−) | 26/10 |
| Venous invasion
(+/−) | 15/21 |
| Intrapancreatic
perineural invasion (+/−) | 29/7 |
| Maximal diameter
(mm) | 25.9±14.6 |
| Histology
(well/mod/por) | 2/30/4 |
| pT
(T1/T2/T3/T4) | 4/4/28/0 |
| pN (+/−) | 16/20 |
| pStage
(IA/IB/IIA/IIB/III/IV) | 4/4/12/16/0/0 |
| Adjuvant therapy
(+/−) | 21/15 |
| Recurrence
(+/−) | 19/17 |
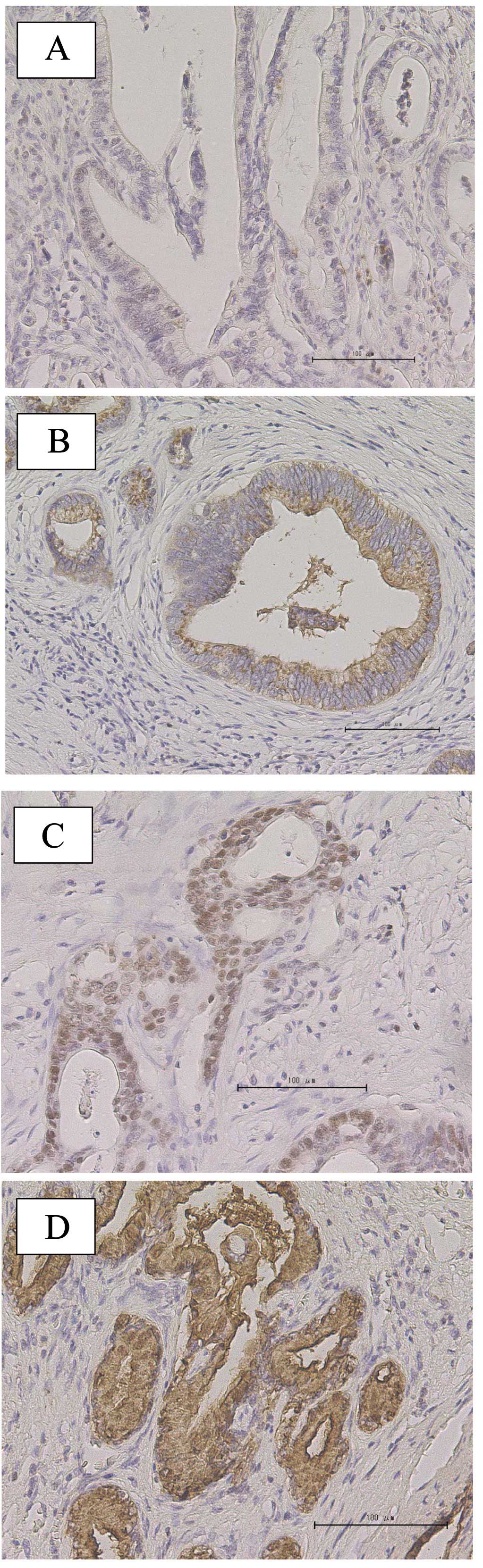
Immunohistochemical staining
The immunohistochemical staining for Sox4 and Ezh2
in 36 pancreatic cancer samples was performed using the method
previously described (20).
Briefly, formalin-fixed, paraffin-embedded 4 μm thick sections were
deparaffinized in xylene, then treated with an antigen-retrieval
procedure, and incubated in methanol containing 0.3% hydrogen
peroxide to block endogenous peroxidase. After incubation with
normal protein block serum, the sections were incubated overnight
at 4ºC with an anti-Sox4 (LifeSpan BioSciences Inc., Seattle, WA,
USA) and anti-Ezh2 (Cell Signaling Technology, Danvers, MA, USA) as
the primary antibodies. Thereafter, the labeling was revealed with
avidin-biotin complex reagents (Vector Laboratories Inc.,
Burlingame, CA, USA) and diaminobenzidine. All sections were
counterstained with hematoxylin. Positivity for Sox4 staining was
defined as detectable nuclear staining of >50% of the cancer
cells (Fig. 2C). Positivity for
Ezh2 staining was defined as detectable nuclear staining or nuclear
and cytoplasm staining of the cancer cells (Fig. 3C and D).
Laser captured microdissection (LCM)
For LCM, 8-μm-thick sections were prepared from the
formalin-fixed paraffin-embedded (FFPE) samples by utilizing the
LCM system (LMD7000; Leica Microsystems GmbH, Wetzlar, Germany) to
separate the epithelial and mesenchymal parts from 36 samples, as
previously shown (21). Total RNA
was extracted using an RNeasy FFPE kit (Qiagen, Tokyo, Japan) with
DNase I treatment, according to the manufacturer's instructions. We
measured the amount of miR-335 expression in cancer parts with
miRNA qRT-PCR. The relative quantification of miRNA expression was
calculated using the comparative CT method (2−ΔCT)
(22). Data were normalized using
RNU48 expression as an endogenous control according to the
manufacturer's instruction.
Statistical analysis
Data were expressed as means ± standard deviation.
The clinicopathological parameters were compared using the Fisher's
exact test, and the continuous variables were compared using the
Mann-Whitney U test. The survival curves were plotted using the
Kaplan-Meier method, and the differences between survival curves
were compared using the log-rank test. A P-value of <0.05
denoted the presence of a statistically significant difference.
Statistical analysis was performed using JMP software version
10.0.2 (SAS Institute Inc., Cary, NC, USA).
Results
The characteristics of the 36 patients
enrolled in the present study
Of the 36 patients in the study, 21 (58.3%) were
males and the mean age of the total patients was 68.5±9.4 years
(range, 47–83). In 10 (27.8%) patients, tumors were localized in
the head and the mean maximal diameter of the tumor was 25.9±14.6
mm. With the histological type of tumor, most of the patients were
moderately differentiated type. Other clinical and
histopathological information is listed in Table I.
The clinical significance of Sox4
expression in the tissue samples
The immunohistochemical staining for Sox4 was
performed in the 36 selected samples. In the cancer sections, the
functional Sox4 protein appears to localize in the nucleus. We
defined as Sox4-positive cases those in which the cells showed
diffused nuclear pattern (>50% of cancer cells) (Fig. 2C), and as Sox4-negative cases those
in which the cells showed spotted nuclear pattern (<50% of
cancer cells) (Fig. 2B) or a
negative pattern (not stained in nucleus or cytoplasm) (Fig. 2A) in the pancreatic cancer lesions.
Among the 36 samples examined, 19 (52.8%) samples were positive for
Sox4, whereas 17 (47.2%) samples were negative.
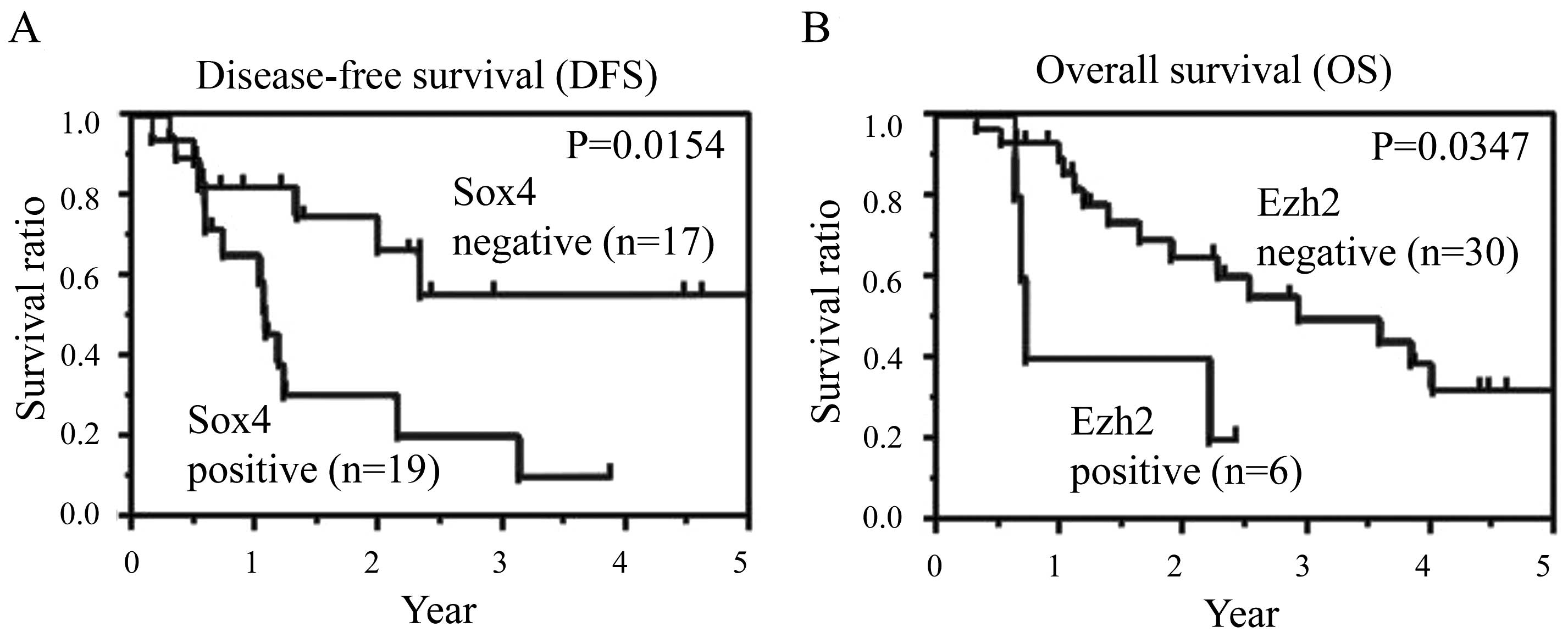
Subsequently, we studied the relationship between
Sox4 expression and clinical outcome. Disease-free survival (DFS)
ratio was significantly lower in Sox4-positive group (P=0.0154)
(Fig. 4A) and overall survival
(OS) ratio tended to be lower in Sox4-positive group (P=0.0623)
(data not shown). It might suggest that Sox4 was more deeply
associated with invasion and metastasis which were relative to DFS
than the refractoriness against several types of therapies such as
gemcitabine and S-1.
The clinical significance of Ezh2
expression in clinical tissue samples
The immunohistochemical staining for Ezh2 was also
performed in the 36 selected samples. In the cancer sections, we
classified the staining pattern into 4 different types (Fig. 3). We defined as Ezh2-positive cases
those in which the cells showed diffused nuclear pattern and
nuclear and cytoplasm pattern (Fig. 3C
and D), and as Ezh2-negative cases those in which the cells
showed cytoplasm pattern (Fig. 3B)
or a negative pattern (not stained in nucleus or cytoplasm)
(Fig. 3A) in the pancreatic cancer
lesions. Among the 36 samples examined, only 6 (16.7%) samples were
positive for Ezh2, whereas 30 (83.3%) samples were negative. Most
of the patients were in the Ezh2-negative group.
Secondly, we assessed the relationship between Ezh2
expression and clinical outcome. OS ratio was significantly lower
in Ezh2 positive group (P=0.0347) (Fig. 4B), whereas DFS ratio was not
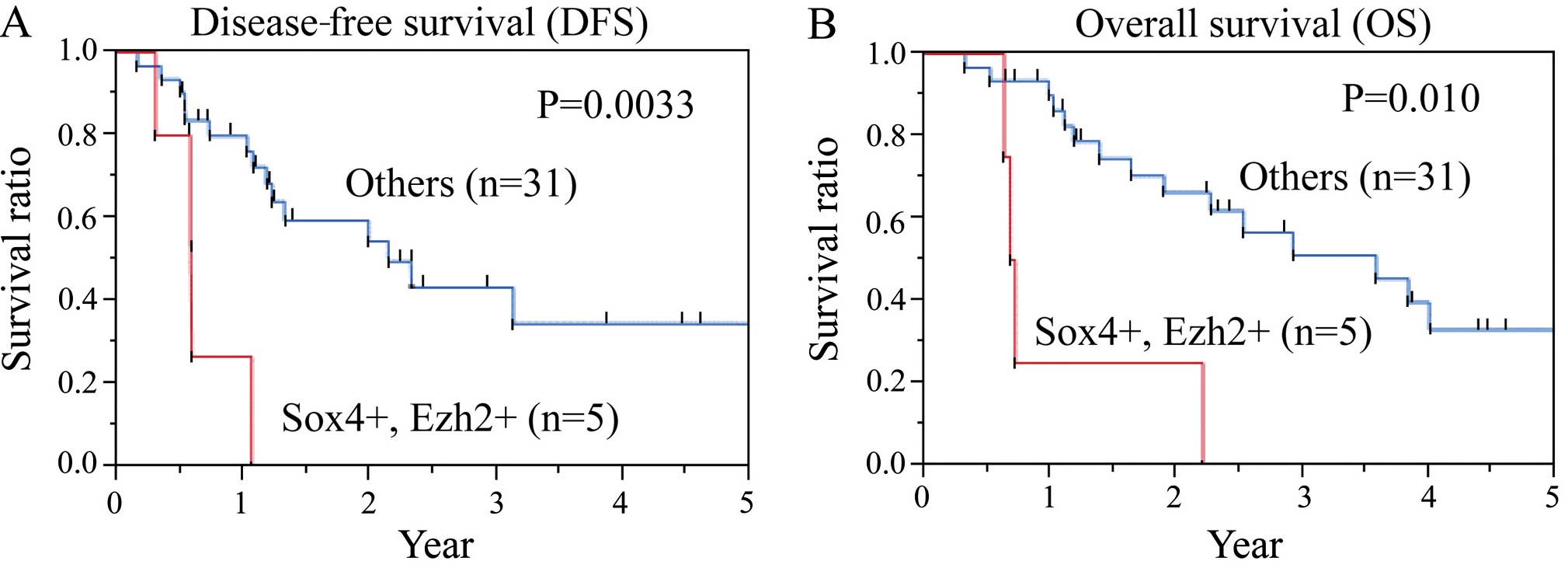
(P=0.138) (data not shown). Therefore, we combined Sox4 expression
with Ezh2 expression and evaluated the relationship between their
expression and prognosis. In Sox4- and Ezh2-positive groups, DFS
and OS were significantly lower than in the other group (Fig. 5). We were able to identify the
patients who had worse prognosis, using these factors.
miR-335 expression of the cancer section
in clinical tissue samples
As pancreatic cancer tissues included substantial
stromal sections, we performed LCM to collect only cancer sections
from tumor tissues with the advice of the pathologists. qRT-PCR was
performed to quantify miR-335 expression in the 36 patients
(Fig. 6A). The expression level of
miR-335 in each sample is shown in Fig. 6B. Of the 36 patients, the mean
expression level of miR-335 is 0.28 (/RNU48). We divided the
patients into two groups by the mean value of miR-335 expression
(high or low). Among the 36 samples examined, 7 (19.4%) samples
were classified into the high group, whereas 29 (80.6%) were
classified into the low group (Fig.
6B).
We evaluated the influence of miR-335 to the
prognosis, however, we did not find any significant difference
between the expression level of miR-335 and DFS or OS (data not
shown).
Sox4 expression and clinicopathological
characteristics
We focused on Sox4 expression and evaluated the
clinical and histopathological factors between Sox4-positive and
-negative groups in order to study the correlation between Sox4
expression and cancer progression, such as lymphatic invasion,
venous invasion, intrapancreatic perineural invasion, and pN (lymph
node metastasis) (Table II). The
histopathological analysis revealed that these factors were not
significantly different between Sox4-positive and -negative groups.
The pathological stage was not significantly different either. In
brief, Sox4 expression did not correlate with existing cancer
progression factors in pancreatic cancer. However, the expression
level of miR-335 which targeted Sox4 was inversely correlated with
Sox4 expression (P=0.0365) and 5 out of 6 Ezh2-positive patients
(83.3%) were in Sox4-positive group. It might suggest that miR-335
regulated Sox4 expression and Sox4 promoted Ezh2 expression as a
transcription factor.
 | Table IIThe comparison of clinicopathological
factors between the Sox4-positive and -negative groups. |
Table II
The comparison of clinicopathological
factors between the Sox4-positive and -negative groups.
| Sox4
expression | |
|---|
|
| |
|---|
| Positive
(n=19) | Negative
(n=17) | P-value |
|---|
| Age (years) | 66.9±10.2 | 70.3±8.5 | 0.366 |
| Gender
(Male/female) | 12/7 | 9/8 | 0.736 |
| Location
(Ph/Pb/Pt) | 10/7/2 | 11/3/3 | 0.465 |
| Maximal diameter
(mm) | 29.6±17.3 | 21.8±9.6 | 0.142 |
| Histology
(well/mod/por) | 0/15/4 | 2/15/0 | 0.0523 |
| Lymphatic invasion
(+/−) | 15/4 | 11/6 | 0.463 |
| Venous invasion
(+/−) | 9/10 | 6/11 | 0.516 |
| Intrapancreatic
perineural invasion (+/−) | 17/2 | 12/5 | 0.219 |
| pT
(T1,T2/T3,T4) | 4/15 | 4/13 | 0.882 |
| pN (+/−) | 11/8 | 5/12 | 0.106 |
| pStage (IA, IB/IIA,
IIB) | 4/15 | 4/13 | 0.882 |
| Ezh2 expression
(+/−) | 5/14 | 1/16 | 0.182 |
| miR-335 expression
(High/low) | 1/18 | 6/11 | 0.0365 |
| Adjuvant therapy
(+/−) | 12/7 | 9/8 | 0.736 |
| Recurrence
(+/−) | 13/6 | 6/11 | 0.0933 |
Relationship between Sox4 expression and
prognosis
We assessed the predictive markers for DFS in the
clinicopathological information. Upon univariate analysis, pT
(tumor invasion depth), pN, venous invasion, and Sox4 expression
were significantly associated with DFS while other prognostic
markers were not (Table III).
Multivariate analysis identified Sox4 expression as a significant
and independent prognostic factor (P=0.0096).
 | Table IIIThe predictive markers for
disease-free survival in the clinicopathological information. |
Table III
The predictive markers for
disease-free survival in the clinicopathological information.
| Univariate
analysis | Mutivariate
analysis |
|---|
|
|
|
|---|
| HR (95% CI) | P-value | HR (95% CI) | P-value |
|---|
| Age (years)
(≥69/<69) | 2.57
(0.97–8.12) | 0.0585 | | |
| Gender
(Male/female) | 0.55
(0.22–1.36) | 0.193 | | |
| Maximal diameter
(mm) (≤26/>26) | 1.11
(0.39–2.85) | 0.837 | | |
| Histology (well,
mod/por) | 0.77
(0.21–4.76) | 0.746 | | |
| pT (T1, T2/T3,
T4) | 0.24
(0.054–0.78) | 0.0150 | 4.97
(0.83–37.00) | 0.0794 |
| pN (+/−) | 5.65
(2.04–17.24) | 0.0009 | 2.79
(0.88–10.47) | 0.0813 |
| Lymphatic invasion
(+/−) | 2.23
(0.80–7.89) | 0.132 | | |
| Venous invasion
(+/−) | 3.14
(1.24–8.33) | 0.0160 | 1.00
(0.33–3.41) | 0.994 |
| Intrapancreatic
perineural invasion (+/−) | 2.66
(0.76–16.87) | 0.140 | | |
| Sox4 expression
(+/−) | 3.22
(1.24–9.37) | 0.0158 | 4.65
(1.42–19.42) | 0.0096 |
| Ezh2 expression
(+/−) | 2.29
(0.64–6.52) | 0.182 | | |
| miR-335 expression
(High/low) | 1.80
(0.58–4.79) | 0.287 | | |
Discussion
In the present study we assessed the expressions of
Sox4, Ezh2 and miR-335 in the identical clinical specimens and
evaluated the relationship between the markers and several
histopathological factors related to clinical outcome. Among them,
Sox4 reflected the cancer progression most sensitively. Probably it
is related to the biological features of Sox4 molecule and
increased Sox4 expression might be the trigger of the EMT
phenomenon.
Sox4 is included in the SRY-related HMG-box (Sox)
family of transcriptional factors, which have a crucial role in
embryonic development and cell fate during organogenesis including
the pancreas (23,24). Sox4 expression is also increased in
many types of cancer, and contributes to cell survival (25), cellular transformation (26) and cancer metastasis (27). In addition, Sox4 directly regulates
important molecules, such as epidermal growth factor receptor
(EGFR), Patched-1 (Ptch1), Delta-like 1 (Dll1), tenascin-C, heat
shock protein 70 (Hsp70), Foxa1, Dicer and RNA helicase A (28). Moreover, Sox4 regulates Wnt pathway
by directly binding to β-catenin (29). Most recently, Sox4 has been
reported to induce EMT in cholangiocarcinoma (30), prostate (31) and breast cancer (32). However, there is no report on Sox4
and pancreatic cancer prognosis.
In the present study, 52.8% of the samples expressed
Sox4 highly at the nuclei. This finding will not contradict the
previous results that pancreatic cancer cells induce EMT at a very
early stage. The ratio of the patients who had lymph node
metastasis was obviously high in Sox4-positive group (57.9%)
compared with the negative group (29.4%) (Table II). Moreover, Sox4-positive
patients had significantly poor DFS and tended to have worse OS.
The results clarify the significance of Sox4 molecule in pancreatic
cancer progression. However, few patients expressed Ezh2 highly at
the nuclei (16.7%). It was due to multiple targets of Sox4 or there
might be a time lag during Sox4 and Ezh2 protein production.
Approximately 80% of Ezh2-positive patients expressed Sox4
strongly. The data showed the importance of the correlation between
Sox4 and Ezh2 in pancreatic cancer (Fig. 1).
The histone methyltransferase, enhancer of Zeste
homolog 2 (Ezh2) is a component of the polycomb repressive complex
2 (PRC2), which epigenetically regulates genes involved in cell
fate determination (33). Ezh2
specifically trimethylates nucleosomal histone H3 at lysine 27
(H3K27me3), and inhibits gene expression with an epigenetic
modification (34). Ezh2 is
expressed highly in a variety of cancers, resulting in malignant
transformation and cancer progression (35–37).
Furthermore, Ezh2 can induce EMT, and increases the metastatic
ability in prostate cancer cells (36,38).
In the present study, Sox4 and Ezh2 double-positive
group had a worse prognosis in DFS and OS ratios; we were able to
predict clinical outcomes from the expression levels. In the lethal
cancer, pancreatic adenocarcinoma, it could link to the improvement
of the clinical outcomes that multimodal therapies were performed
on patients predicted to have poor prognosis. On the other hand,
miR-335 was not associated with the prognosis, but it related to
Sox4 expression inversely, which might suggest that miR-335
targeted the Sox4 gene.
In conclusion, Sox4/Ezh2 axis is associated with
cancer progression and Sox4 is a novel, independent prognostic
factor in pancreatic cancer.
Acknowledgements
We thank the members of our laboratories for their
contribution. The present study was supported in part by a
Grant-in-Aid for Scientific Research and a grant from the Platform
for Drug Discovery, Informatics, and Structural Life Science, from
the Ministry of Education, Culture, Sports, Science and Technology;
a Grant-in-Aid from the Third Comprehensive 10-year Strategy for
Cancer Control, Ministry of Health, Labor and Welfare; a grant from
the Kobayashi Cancer Research Foundation; a grant from the Princess
Takamatsu Cancer Research Fund, Japan; and a grant from the
National Institute of Biomedical Innovation, Japan.
References
|
1
|
Hoyert DL, Heron MP, Murphy SL and Kung
HC: Deaths: Final data for 2003. Natl Vital Stat Rep. 54:1–120.
2006.PubMed/NCBI
|
|
2
|
Hidalgo M: Pancreatic cancer. N Engl J
Med. 362:1605–1617. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Shrikhande SV, Kleeff J, Reiser C, Weitz
J, Hinz U, Esposito I, Schmidt J, Friess H and Büchler MW:
Pancreatic resection for M1 pancreatic ductal adenocarcinoma. Ann
Surg Oncol. 14:118–127. 2007. View Article : Google Scholar
|
|
4
|
Bilimoria KY, Bentrem DJ, Ko CY, Stewart
AK, Winchester DP and Talamonti MS: National failure to operate on
early stage pancreatic cancer. Ann Surg. 246:173–180. 2007.
View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Oettle H, Neuhaus P, Hochhaus A, Hartmann
JT, Gellert K, Ridwelski K, Niedergethmann M, Zülke C, Fahlke J,
Arning MB, et al: Adjuvant chemotherapy with gemcitabine and
long-term outcomes among patients with resected pancreatic cancer:
The CONKO-001 randomized trial. JAMA. 310:1473–1481. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Thiery JP, Acloque H, Huang RY and Nieto
MA: Epithelial-mesenchymal transitions in development and disease.
Cell. 139:871–890. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Hay ED: An overview of
epithelio-mesenchymal transformation. Acta Anat (Basel). 154:8–20.
1995. View Article : Google Scholar
|
|
8
|
Thiery JP: Epithelial-mesenchymal
transitions in development and pathologies. Curr Opin Cell Biol.
15:740–746. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Grünert S, Jechlinger M and Beug H:
Diverse cellular and molecular mechanisms contribute to epithelial
plasticity and metastasis. Nat Rev Mol Cell Biol. 4:657–665. 2003.
View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Huber MA, Kraut N and Beug H: Molecular
requirements for epithelial-mesenchymal transition during tumor
progression. Curr Opin Cell Biol. 17:548–558. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Satoh K, Hamada S and Shimosegawa T:
Involvement of epithelial to mesenchymal transition in the
development of pancreatic ductal adenocarcinoma. J Gastroenterol.
50:140–146. 2015. View Article : Google Scholar
|
|
12
|
Thiery JP: Epithelial-mesenchymal
transitions in tumour progression. Nat Rev Cancer. 2:442–454. 2002.
View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Rhim AD, Mirek ET, Aiello NM, Maitra A,
Bailey JM, McAllister F, Reichert M, Beatty GL, Rustgi AK,
Vonderheide RH, et al: EMT and dissemination precede pancreatic
tumor formation. Cell. 148:349–361. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Polyak K and Weinberg RA: Transitions
between epithelial and mesenchymal states: Acquisition of malignant
and stem cell traits. Nat Rev Cancer. 9:265–273. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Cano CE, Motoo Y and Iovanna JL:
Epithelial-to-mesenchymal transition in pancreatic adenocarcinoma.
Sci World J. 10:1947–1957. 2010. View Article : Google Scholar
|
|
16
|
Browne G, Sayan AE and Tulchinsky E: ZEB
proteins link cell motility with cell cycle control and cell
survival in cancer. Cell Cycle. 9:886–891. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Gunasinghe NP, Wells A, Thompson EW and
Hugo HJ: Mesenchymal-epithelial transition (MET) as a mechanism for
metastatic colonisation in breast cancer. Cancer Metastasis Rev.
31:469–478. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Tiwari N, Tiwari VK, Waldmeier L, Balwierz
PJ, Arnold P, Pachkov M, Meyer-Schaller N, Schübeler D, van
Nimwegen E and Christofori G: Sox4 is a master regulator of
epithelial-mesenchymal transition by controlling Ezh2 expression
and epigenetic reprogramming. Cancer Cell. 23:768–783. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Tavazoie SF, Alarcón C, Oskarsson T, Padua
D, Wang Q, Bos PD, Gerald WL and Massagué J: Endogenous human
microRNAs that suppress breast cancer metastasis. Nature.
451:147–152. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Kondo M, Yamamoto H, Nagano H, Okami J,
Ito Y, Shimizu J, Eguchi H, Miyamoto A, Dono K, Umeshita K, et al:
Increased expression of COX-2 in nontumor liver tissue is
associated with shorter disease-free survival in patients with
hepatocellular carcinoma. Clin Cancer Res. 5:4005–4012. 1999.
|
|
21
|
Nishida N, Nagahara M, Sato T, Mimori K,
Sudo T, Tanaka F, Shibata K, Ishii H, Sugihara K, Doki Y, et al:
Microarray analysis of colorectal cancer stromal tissue reveals
upregulation of two oncogenic miRNA clusters. Clin Cancer Res.
18:3054–3070. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Schmittgen TD, Jiang J, Liu Q and Yang L:
A high-throughput method to monitor the expression of microRNA
precursors. Nucleic Acids Res. 32:e432004. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Restivo A, Piacentini G, Placidi S,
Saffirio C and Marino B: Cardiac outflow tract: A review of some
embryogenetic aspects of the conotruncal region of the heart. Anat
Rec A Discov Mol Cell Evol Biol. 288:936–943. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Lioubinski O, Müller M, Wegner M and
Sander M: Expression of Sox transcription factors in the developing
mouse pancreas. Dev Dyn. 227:402–408. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Aaboe M, Birkenkamp-Demtroder K, Wiuf C,
Sørensen FB, Thykjaer T, Sauter G, Jensen KM, Dyrskjøt L and
Ørntoft T: SOX4 expression in bladder carcinoma: Clinical aspects
and in vitro functional characterization. Cancer Res. 66:3434–3442.
2006. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Liu P, Ramachandran S, Ali Seyed M,
Scharer CD, Laycock N, Dalton WB, Williams H, Karanam S, Datta MW,
Jaye DL, et al: Sex-determining region Y box 4 is a transforming
oncogene in human prostate cancer cells. Cancer Res. 66:4011–4019.
2006. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Liao YL, Sun YM, Chau GY, Chau YP, Lai TC,
Wang JL, Horng JT, Hsiao M and Tsou AP: Identification of SOX4
target genes using phylogenetic footprinting-based prediction from
expression microarrays suggests that overexpression of SOX4
potentiates metastasis in hepatocellular carcinoma. Oncogene.
27:5578–5589. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Scharer CD, McCabe CD, Ali-Seyed M, Berger
MF, Bulyk ML and Moreno CS: Genome-wide promoter analysis of the
SOX4 transcriptional network in prostate cancer cells. Cancer Res.
69:709–717. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Sinner D, Kordich JJ, Spence JR, Opoka R,
Rankin S, Lin SC, Jonatan D, Zorn AM and Wells JM: Sox17 and Sox4
differentially regulate beta-catenin/T-cell factor activity and
proliferation of colon carcinoma cells. Mol Cell Biol.
27:7802–7815. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Wang W, Zhang J, Zhan X, Lin T, Yang M, Hu
J, Han B and Hu S: SOX4 is associated with poor prognosis in
cholangiocarcinoma. Biochem Biophys Res Commun. 452:614–621. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Wang L, Li Y, Yang X, Yuan H, Li X, Qi M,
Chang YW, Wang C, Fu W, Yang M, et al: ERG-SOX4 interaction
promotes epithelial-mesenchymal transition in prostate cancer
cells. Prostate. 74:647–658. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Parvani JG and Schiemann WP: Sox4, EMT
programs, and the metastatic progression of breast cancers:
Mastering the masters of EMT. Breast Cancer Res. 15:R722013.
View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Marchesi I, Giordano A and Bagella L:
Roles of enhancer of zeste homolog 2: From skeletal muscle
differentiation to rhabdomyosarcoma carcinogenesis. Cell Cycle.
13:516–527. 2014. View
Article : Google Scholar : PubMed/NCBI
|
|
34
|
Sparmann A and van Lohuizen M: Polycomb
silencers control cell fate, development and cancer. Nat Rev
Cancer. 6:846–856. 2006. View
Article : Google Scholar : PubMed/NCBI
|
|
35
|
Varambally S, Cao Q, Mani RS, Shankar S,
Wang X, Ateeq B, Laxman B, Cao X, Jing X, Ramnarayanan K, et al:
Genomic loss of microRNA-101 leads to overexpression of histone
methyltransferase EZH2 in cancer. Science. 322:1695–1699. 2008.
View Article : Google Scholar : PubMed/NCBI
|
|
36
|
Chen H, Tu SW and Hsieh JT:
Down-regulation of human DAB2IP gene expression mediated by
polycomb Ezh2 complex and histone deacetylase in prostate cancer. J
Biol Chem. 280:22437–22444. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
37
|
Cao Q, Yu J, Dhanasekaran SM, Kim JH, Mani
RS, Tomlins SA, Mehra R, Laxman B, Cao X, Yu J, et al: Repression
of E-cadherin by the polycomb group protein EZH2 in cancer.
Oncogene. 27:7274–7284. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
38
|
Min J, Zaslavsky A, Fedele G, McLaughlin
SK, Reczek EE, De Raedt T, Guney I, Strochlic DE, Macconaill LE,
Beroukhim R, et al: An oncogene-tumor suppressor cascade drives
metastatic prostate cancer by coordinately activating Ras and
nuclear factor-kappaB. Nat Med. 16:286–294. 2010. View Article : Google Scholar : PubMed/NCBI
|