Introduction
Ganglia, caused by mucinous transformation of
periarticular connective tissue, are the most common cystic lesions
found around the joints, usually occurring near joints, tendons and
tendon sheaths. Intraosseous ganglia are less common, but are
macroscopically and histologically identical to soft tissue
ganglia, consisting of a multilocular, thick, fibrous walled
cyst-like structure filled with mucin-rich fluid. The clinical
characteristics and pathogenesis of these ganglia are diverse
(1–3).
Intraosseous ganglia occur in the mature skeleton in
patients of all ages, with a peak incidence in the fourth and fifth
decades of life (4). The femoral
head and tibia are commonly affected. However, to the best of our
knowledge, there has been no report of a juxta-articular ganglion
in the diaphysis of the fibula.
This study presents a case of juxta-articular
ganglion in the fibula of a 65-year-old male patient treated in The
Second Affiliated Hospital, Zhejiang University (Hangzhou,
China).
Case report
A 65-year-old male patient presented in November
2015 with left lower limb pain after spraining his left ankle 2
months prior. An X-ray film of the left lower limb revealed a wide
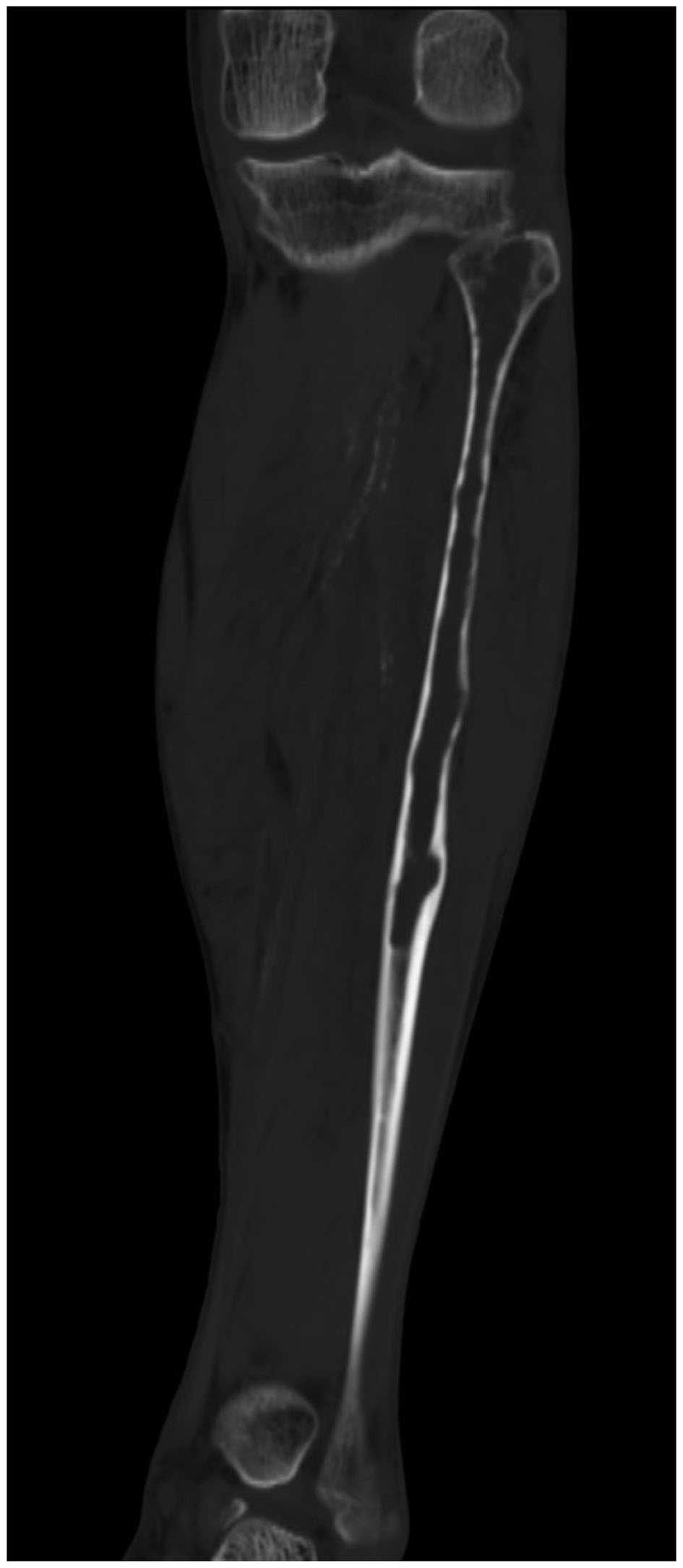
area of destruction of the fibula. A computed tomography (CT)
examination revealed a 18-cm lesion in the proximal fibula, with
breakthrough of the cortical of the fibula in places (Fig. 1). On magnetic resonance imaging (MRI)
examination, the lesion presented as a well-defined fluid
collection with low intensity on T1-weighted images and very high
intensity on T2-weighted images (Fig.
2). On certain slices, a soft tissue mass growing out of the
fibula was observed (Fig. 3). The
patient was a non-smoker and the chest CT excluded lung cancer. The
initial suspected diagnosis was a fibular invasive tumor, and
metastasis could not be excluded. An open biopsy was scheduled and
a transparent, jelly-like material oozed out of the cavity when the
bone cortex was drilled. In addition, white lime-like material was
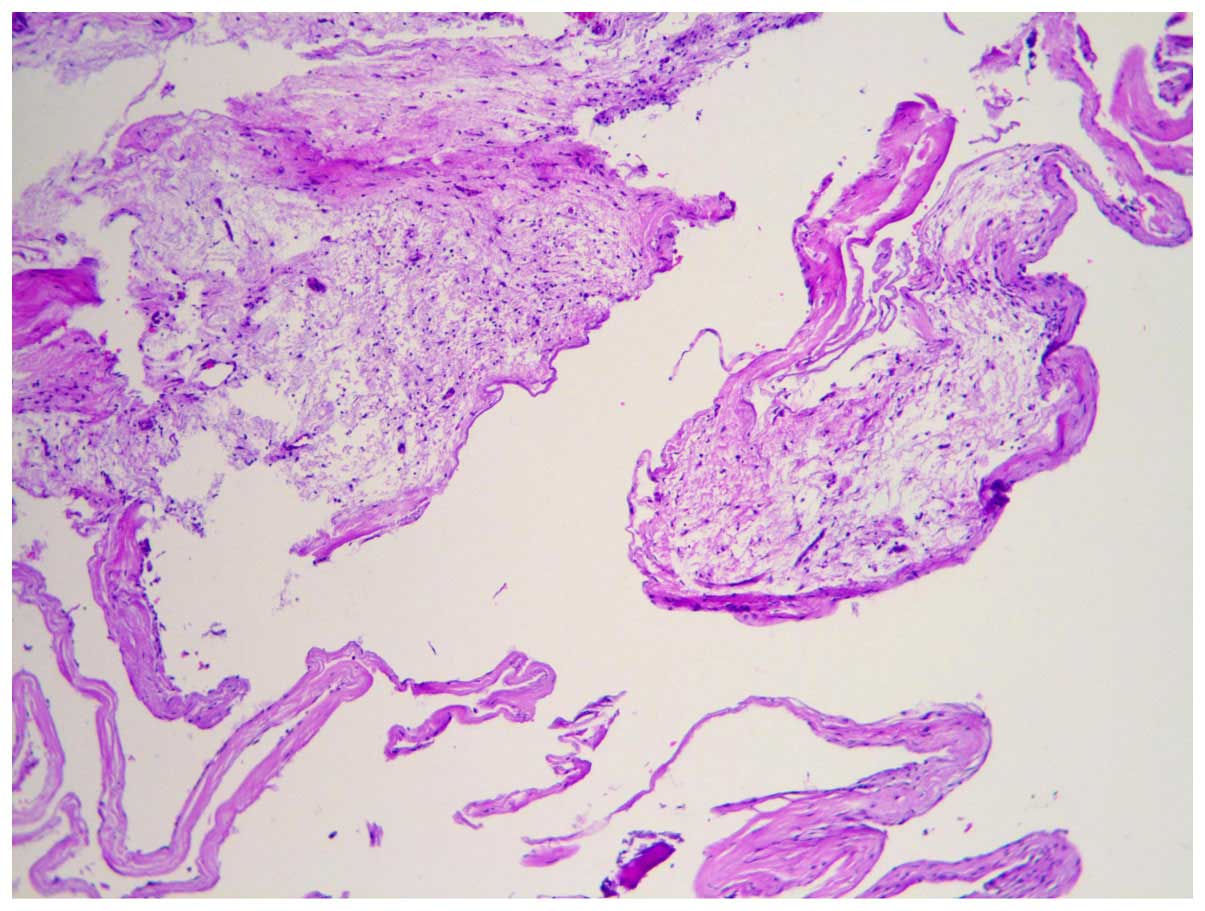
observed on the cavity wall. The frozen section biopsy revealed a
wall consisting of a fibrous capsule and bone tissue, and the
lesion was considered to be benign (Fig.
4). As the lesion was extensive, wide resection was performed.
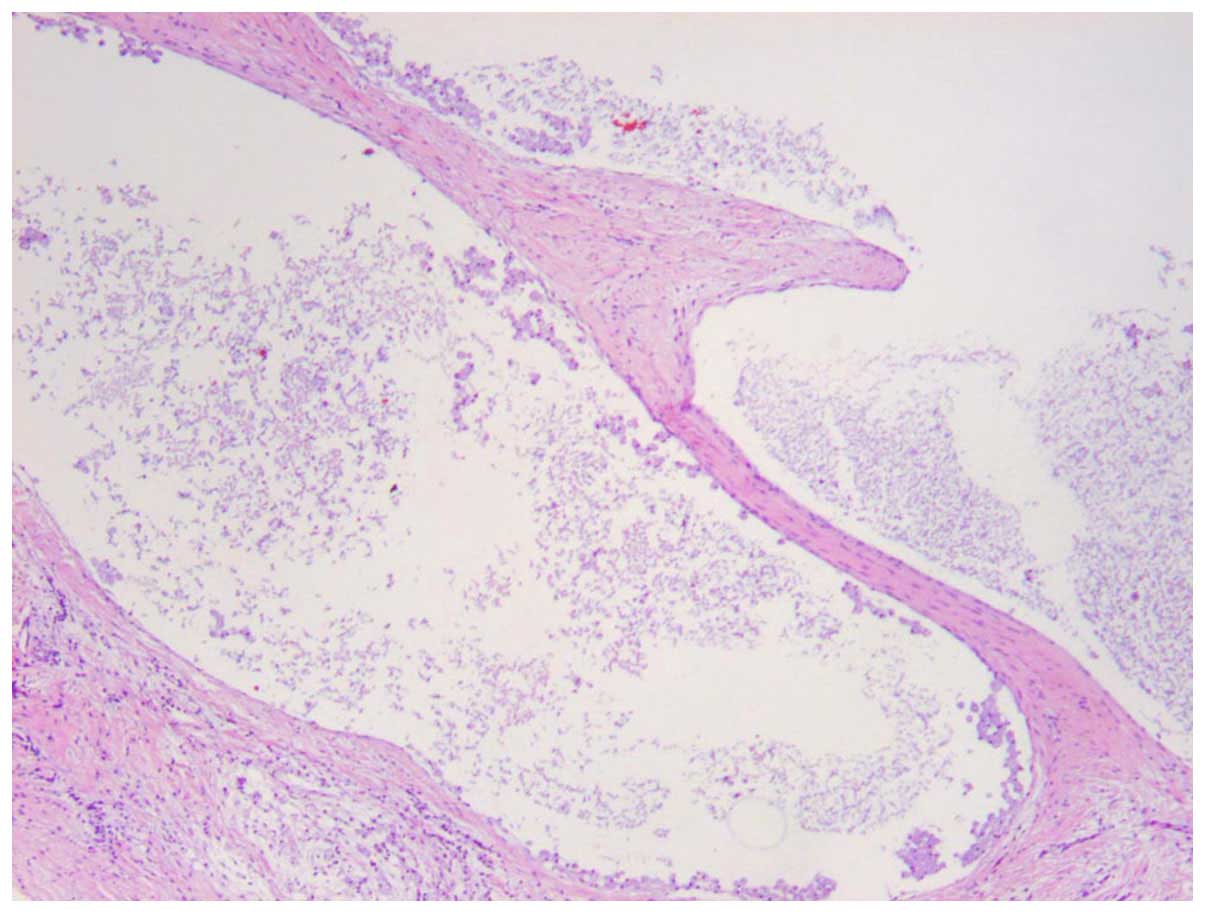
The histological examination later confirmed that the lesion was an
intraosseous ganglion (Fig. 5). At 3
months after surgery, the patient was able to walk normally and had
no complaints of pain. The patient attended the clinic every 3
months. At the 3-month follow-up, the patient was able to walk
normally and had no complains of pain. After 6 months, an X-ray of
the fibula was performed and the patient remained
recurrence-free.
Discussion
An intraosseous ganglion cyst is an uncommon, benign
cystic bone lesion occurring in close association with an articular
surface (5). However, intraosseous
ganglion cysts of the fibula are very uncommon.
Male patients have a minor preponderance for this
disease. The age distribution is very wide (18–86 years according
to the literature) and the majority of the patients are middle-aged
(6). The aetiology and pathogenesis
of intraosseous ganglions remain unknown, although there are
several theories on the pathogenesis of the cyst (7,8).
Wei et al reported several cases supporting
this type of theory (8). Schajowicz
et al (7) hypothesized it may
be caused by intramedullary metaplasia followed by mucoid
degeneration with intraosseous cyst formation. Altered mechanical
stress may also lead to intramedullary vascular disturbance and
aseptic necrosis. Subsequently, the revitalization of these
necrotic areas leads to fibroblastic proliferation and mucoid
degeneration. Crane hypothesized the lesion may be caused by
leakage of synovial fluid following injury of the cartilaginous
surface (9). The majority of the
authors presently support these two previously mentioned theories,
although these theories cannot fully explain all the cases. Thus,
further investigation is required.
Schajowicz et al (7) suggested there are two types of
intraosseous ganglion: The first is a primary or idiopathic type
that arises de novo within the bone; the second type of
intraosseous ganglion is considered to occur when there is
penetration of an extraosseous lesion into the underlying bone.
The diagnosis of intraosseous ganglion is not
difficult, but it must be differentially diagnosed from a
unicameral bone cyst, aneurysmal bone cyst, chondromyxoid fibroma,
Brodie's abscess, giant-cell tumor, fibrous dysplasia and pigmented
villonodular synovitis. These patients may present with persistent
pain that worsens when using the affected region. Physical
examination may reveal edema with tenderness; however, there are
usually no abnormal findings. On radiographs, the intraosseous
ganglia appear as well-defined, lytic, oval, or round lesions
located in the juxta-articular (subchondral) region, with or
without cortical expansion and soft tissue extension. The majority
of the lesions are small (1–2 cm). Communication between the cyst
and the joint space has been reported. However, as in the present
case, the cyst may occasionally be larger than usual, without an
obvious communication with the joint, or may even be located
outside the joint.
Macroscopically, the intact cyst is usually smooth
or slightly lobulated and bulging, with a white, fibrous outer
surface. The external surface may appear gray-blue if the wall is
thinned. The microscopic examination of the intraosseous ganglion
is identical to its soft tissue counterpart, revealing a cyst wall
of fibrous tissue and fibrocytes, with areas of collagenous
material (5).
The differential diagnosis of intraosseous ganglion
includes unicameral bone cyst, chondromyxoid fibroma, Brodie's
abscess, giant-cell tumor, fibrous dysplasia and pigmented
villonodular synovitis. Our patient underwent an open biopsy, and
the pathological examination revealed a benign tumor. The optimal
treatment of symptomatic intraosseous ganglia is surgical excision
by curettage followed by bone grafting to prevent recurrence and
the risk of collapsing fracture (9).
As the lesion was wide and there was a high risk of pathological
fracture after curettage, wide resection of the fibula was
performed. At 3 months after surgery, the patient was able to walk
normally and had no complaints of pain.
Intraosseous ganglia are uncommon and, to the best
of our knowledge, there are no reported cases in the fibula.
However, this type of lesion must be included in the differential
diagnosis of calf pain. Imaging in the form of an MRI is crucial
for diagnosis and operative planning, accompanied with
histopathology to confirm the diagnosis. Surgical curettage
followed by bone grafting is the treatment of choice. However, if
the lesion is extensive, resection must be considered.
References
|
1
|
Aoki Y, Miyamoto K and Harada Y: A case of
ganglion in acetabulum. Kanto Soc Orthop Traumatol. 29:257–261.
1998.
|
|
2
|
Arao M, Otani T, Funasaki H, Ono N, Katou
T and Serizawa Y: Intraosseous ganglion of the scapula: a case
report. Kanto Soc Orthop Traumatol. 34:239–242. 2003.
|
|
3
|
Aritomi K, Kusunose K, Kayaoka M, Tomita
Y, Miyazaki H and Hayashi R: Intraosseous ganglion of the scaphoid:
A case report. Orthop Surg. 55:1185–1187. 2004.
|
|
4
|
Williams HJ, Davies AM, Allen G, Evans N
and Mangham DC: Imaging features of intraosseous ganglia: A report
of 45 cases. Eur Radiol. 14:1761–1769. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Ferkel RD, Field J, Scherer WP, Bernstein
ML and Kasimian D: Intraosseous ganglion cysts of the ankle: A
report of three cases with long-term follow-up. Foot Ankle Int.
20:384–388. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Sedeek SM, Choudry Q and Garg S:
Intraosseous ganglion of the distal tibia: Clinical, radiological,
and operative management. Case Rep Orthop.
2015:7592572015.PubMed/NCBI
|
|
7
|
Schajowicz F, Sainz M Clavel and Slullitel
JA: Juxta-articular bone cysts (intra-osseous ganglia): a
clinicopathological study of eighty-eight cases. J Bone Joint Surg
Br. 61:107–116. 1979.PubMed/NCBI
|
|
8
|
Wei XJ, Wang XF, Wang XG, et al:
Juxta-articular bone cyst(intra-osseous ganglion)-report of one
rare multiple case in femur. Orthop J Chin. 10:1048–1050. 2002.
|
|
9
|
Crane AR and Scarano JJ: Synovial cysts
(ganglia) of bone. Report of two cases. J Bone Joint Surg Am.
49:355–361. 1967.PubMed/NCBI
|