Introduction
Extranodal nasal-type natural killer (NK)/T-cell
lymphoma is a rare malignancy, exhibiting a high prevalence among
Asians, including Chinese, Japanese and North Korean, as well as
native South American populations, but is uncommon among European
and North American individuals (1).
NK/T-cell lymphoma is characterised by an angiodestructive growth
pattern and usually diagnosed in adult, middle-aged individuals,
with a male:female ratio of 2-4:1. This disease has been found to
be significantly associated with Epstein-Barr virus (EBV)
infection. The most common site of involvement is the nasal cavity
and/or upper aerodigestive tract, and other midline facial
structures. The most frequent sites of recurrence are the soft
tissues, skin, gastrointestinal tract and testis (2,3), whereas
metastatic esophageal lymphoma is extremely rare. The prognosis of
EN-NK/T-NT varies, mostly depending on clinical factors, including
International Prognostic Index, clinical stage, applied treatment,
proliferation rate and primary tumour location. Although extranodal
NK/T-NT is sensitive to radiotherapy, it is inherently resistant to
chemotherapy due to the expression of P-glycoprotein, and
consequently, it is associated with a poorer prognosis compared
with other types of lymphoma (4,5). We herein
report a case of extranodal nasal-type NK/T-cell lymphoma in a
patient presenting with an esophageal mass.
Case report
Clinical history
A 21-year-old man, who had been diagnosed in 2011
with nasal NK/T-cell lymphoma, was admitted to the Department of
Oncology at Tai-He Hospital (Hubei, China). The patient was treated
with 4 cycles of cyclophosphamide, vincristine, daunorubicin and
dexamethasone (CHOP regimen), followed by local radiotherapy with
56 Gy in 26 fractions (2.15 Gy/fraction) of gross tumor volume. The
patient remained in remission until April, 2014, when he was
admitted with a 2-month history of discontinuous fever peaking to
39°C without an obvious cause, and difficulty in swallowing. The
patient underwent an emergent esophagogastroduodenoscopy, which
revealed an irregular mucosal elevation at a distance of 30–36 cm
from the incisors. The mucosal surface was eroded and mildly
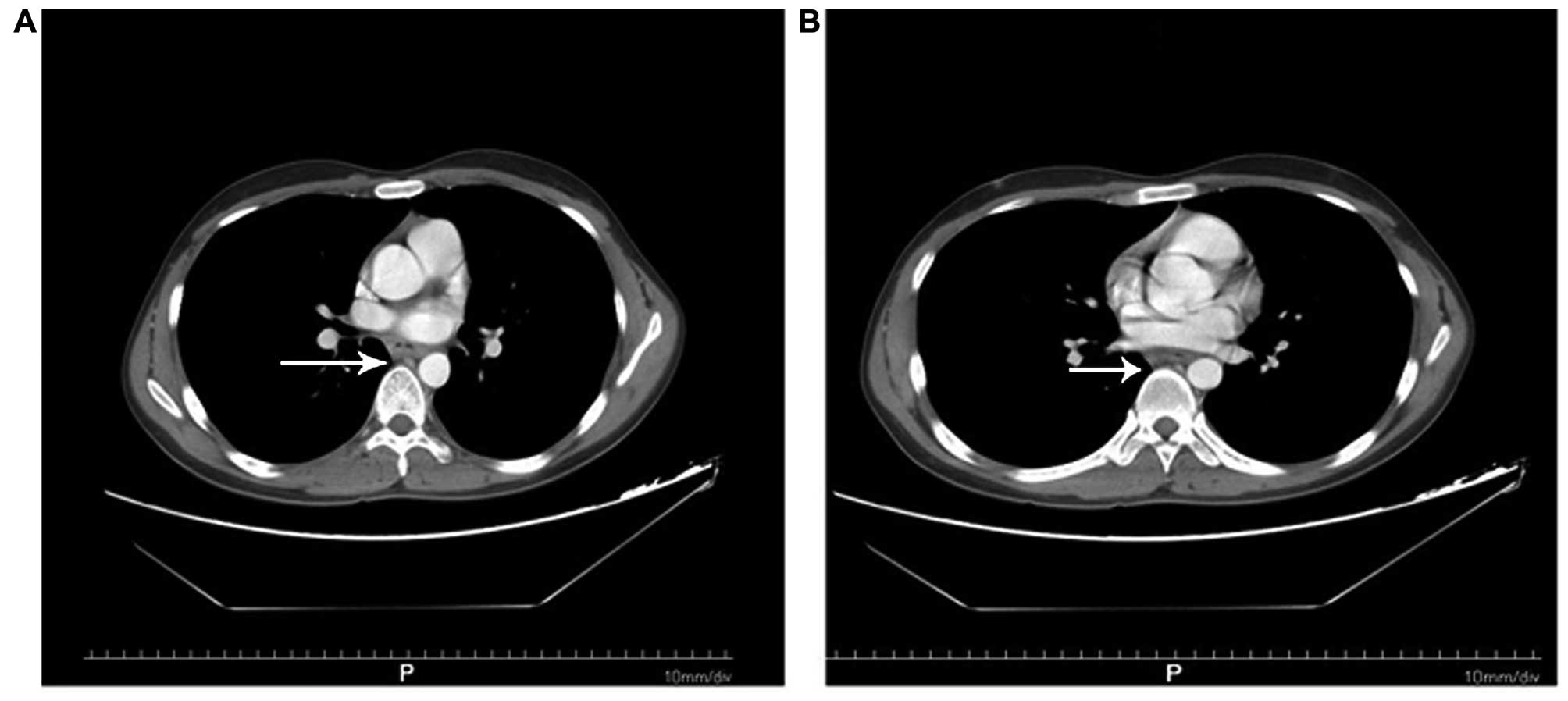
indurated. A computed tomography scan revealed a mild thickening of
the wall of the lower esophagus (Fig.
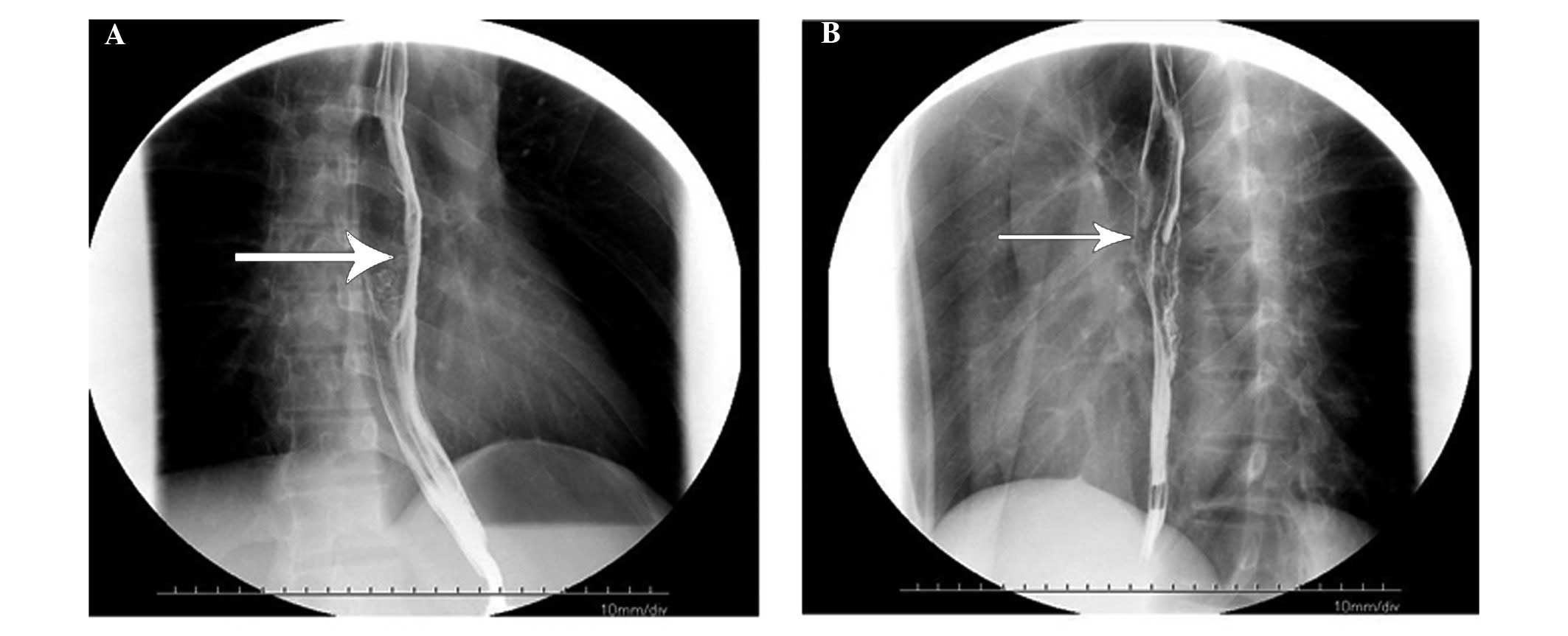
1). The barium swallow indicated slow passing of the barium
through the lower esophagus (equivalent to the level of the
thoracic vertebrae 7–9), with esophageal wall stiffness, mildly
limited expansion and mucosal damage; the length of lesion was ~8.1
cm (Fig. 2). The patient reported no
symptoms of cough, expectoration, hemoptysis or abdominal pain.
Pathological findings
The tumor cells exhibited a notable
angioinfiltrative growth pattern, with homocentric arrangement
around small arteries. The lymphoma cells were densely assembled
and displayed abundant cytoplasm, enlarged nuclei and several large
nucleoli. Mitotic figures were infrequent. Immunohistochemically,
the neoplastic cells were leukocyte common antigen
(LCA)+, B-cell lymphoma 6 protein+, T-cell
intracytoplasmic antigen 1 (TIA-1)+, CD68+,
Ki-67+ (30%), EBV+, P63−,
CD56−, CD3−, CD20− and cytokeratin
5/6−. Based on the endoscopic, computed tomography and
immunophenotypical findings, the diagnosis of esophageal metastasis
from extranodal nasal-type NK/T-cell lymphoma was established.
The patient declined further treatment following
diagnosis, due to financial difficulties, and there have been no
follow-up visits or other communication following his discharge
from the hospital.
Discussion
NK cells are cytotoxic lymphocytes critical to the
innate immune system, which mediate lysis of tumor cells and other
infected cells (6). NK cell-derived
neoplasms are classified into two types, namely aggressive NK-cell
leukemia and extranodal nasal-type NK/T-cell lymphoma, according to
the World Health Organization (WHO) criteria (1,7). Nasal
NK/T-cell lymphoma is consistently associated with EBV infection
(8).
According to the WHO criteria, the diagnosis of
nasal-type NK/T-cell lymphoma requires EBV positivity and the
presence of cytotoxic granules (2).
EBV-positive NK/T-cell lymphoma exhibiting typical clinical and
morphological characteristics may be classified even if they
deviate from the classical immunophenotype, e.g., CD8 positivity or
CD56 negativity (9). The present case
exhibited the immunophenotype of tumor cells typical of nasal-type
NK/T-cell lymphoma, i.e., LCA+, TIA-1+,
CD68+, CD56− and CD3−. As a
hallmark of nasal-type NK/T-cell lymphoma, TIA-1 and EBV-encoded
RNA were the most sensitive markers of the disease. Nasal NK/T-cell
lymphoma is usually associated with EBV infection, as in the
present case. A high level of circulating plasma EBV has been
correlated with high tumor load and poorer response to treatment
(10). In this case, EBV may have
also been an etiological factor in the development of the nasal
lymphoma.
NK/T-cell lymphoma often occurs in the nose or the
upper aerodigestive tract and is associated with a worse prognosis.
Other sites, including the skin, spleen, salivary glands,
gastrointestinal tract, lungs and testes, may also be affected
(11). It has been reported that
muscle tissue, the adrenal glands and the female genital tract are
unusual sites of involvement (9).
Bone marrow involement occurs in <10% of patients and distant
metastasis is rare. The present case was associated with a highly
aggressive clinical course, with distant metastasis to the
esophagus. Extranodal NK/T-cell lymphoma metastasizing to the
esophagus is extremely rare and the available data on optimal
treatment strategies are currently limited. Distant dissemination
of nasal NK/T-cell lymphoma occurs early in the clinical course of
the disease. It is crucial to distinguish nasal-type NK/T-cell
lymphoma from others types, as the prognosis and treatment of
secondary metastases differ significantly.
In conclusion, the present case demonstrated that
primary NK/T-cell lymphoma with a poor prognosis may metastasize to
the esophagus. This may represent a diagnostic pitfall that the
doctor should be aware of and further consider the spectrum of
differential diagnosis of esophageal tumors. Due to the clinical
aggressiveness and poor prognosis of this malignancy, more
effective therapeutic regiments are required for its
management.
Informed consent was obtained from the family of the
patient for publication of this case report and any accompanying
images.
Acknowledgements
We acknowledge funds provided for outstanding young
scientific and technological innovation team projects by Hubei
University of Medicine (2014 CXG02).
References
|
1
|
Chan JKC, Quintanilla-Martinez L, Ferry JA
and Peh SC: Extranodal NK/T-cell lymphoma, nasal type. World Health
Organization Classification of Tumours of Haematopoietic and
Lymphoid Tissues. Swerdlow SH, Campo E, Harris NK, et al: IARC
Press. (Lyon). 285–288. 2008.
|
|
2
|
Au WY, Weisenburger DD, Intragumtornchai
T, Nakamura S, Kim WS, Sng I, Vose J, Armitage JO and Liang R:
International Peripheral T-Cell Lymphoma Project: Clinical
differences between nasal and extranasal natural killer/T-cell
lymphoma: A study of 136 cases from the International Peripheral
T-Cell Lymphoma Project. Blood. 113:3931–3937. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Barrionuevo C, Zaharia M, Martinez MT,
Taxa L, Misad O, Moscol A, Sarria G, Guerrero I, Casanova L, Flores
C, et al: Extranodal NK/T-cell lymphoma, nasal type: Study of
clinicopathologic and prognosis factors in a series of 78 cases
from Peru. Appl Immunohistochem Mol Morphol. 15:38–44. 2007.
View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Suzuki R, Takeuchi K, Ohshima K and
Nakamura S: Extranodal NK/T-cell lymphoma: diagnosis and treatment
cues. Hematol Oncol. 26:66–72. 2008. View
Article : Google Scholar : PubMed/NCBI
|
|
5
|
Liang L, Nong L, Zhang S, Zhao J, Ti H,
Dong Y, et al: The downregulation of PRDM1/Blimp-1 is associated
with aberrant expression of miR-223 in extranodal NK/T-cell
lymphoma, nasal type. J Exp Clin Cancer Res. 33:72014. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Spits H, Lanier LL and Phillips JH:
Development of human T and natural killer cells. Blood.
85:2654–2670. 1995.PubMed/NCBI
|
|
7
|
Chan JKC, Jaffe ES, Ralfkiaer E and Ko YH:
Aggressive NK-cell leukaemia. WHO Classification of Tumours of
Haematopoietic and Lymphoid Tissues. International Agency for
Research on Cancer. (Lyon, France). 276–277. 2008.
|
|
8
|
Chan JKC, Jaffe ES and Ralfkiaer E:
Extranodal NK/T-cell lymphoma, nasal type. World Health
Organization Classification of Tumors. Pathology & genetics:
Tumors of hematopoietic and lymphoid tissues. Jaffe ES, Harris NL,
Stein H, et al: IARC Press. (Lyon, France). 204–207. 2001.
|
|
9
|
Hasserjian RP and Harris NL: NK-cell
lymphomas and leukemias: A spectrum of tumors with variable
manifestations and immunophenotype. Am J Clin Pathol. 127:860–868.
2007. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Au WY, Pang A, Choy C, Chim CS and Kwong
YL: Quantification of circulating Epstein-Barr virus (EBV) DNA in
the diagnosis and monitoring of natural killer cell and
EBV-positive lymphomas in immunocompetent patients. Blood.
104:243–249. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Cheung MMC, Chan JKC, Lau WH, Foo W, Chan
PT, Ng CS and Ngan RK: Primary non-Hodgkin's lymphoma of the nose
and nasopharynx: Clinical features, tumor immunophenotype, and
treatment outcome in 113 patients. J Clin Oncol. 16:70–77.
1998.PubMed/NCBI
|