|
1
|
Leigh PN, Al-Sarraj S and DiMauro S:
Impact commentaries. Subacute necrotising encephalomyelopathy
(Leigh's disease; Leigh syndrome). J Neurol Neurosurg Psychiatry.
86:363–365. 2015. View Article : Google Scholar : PubMed/NCBI
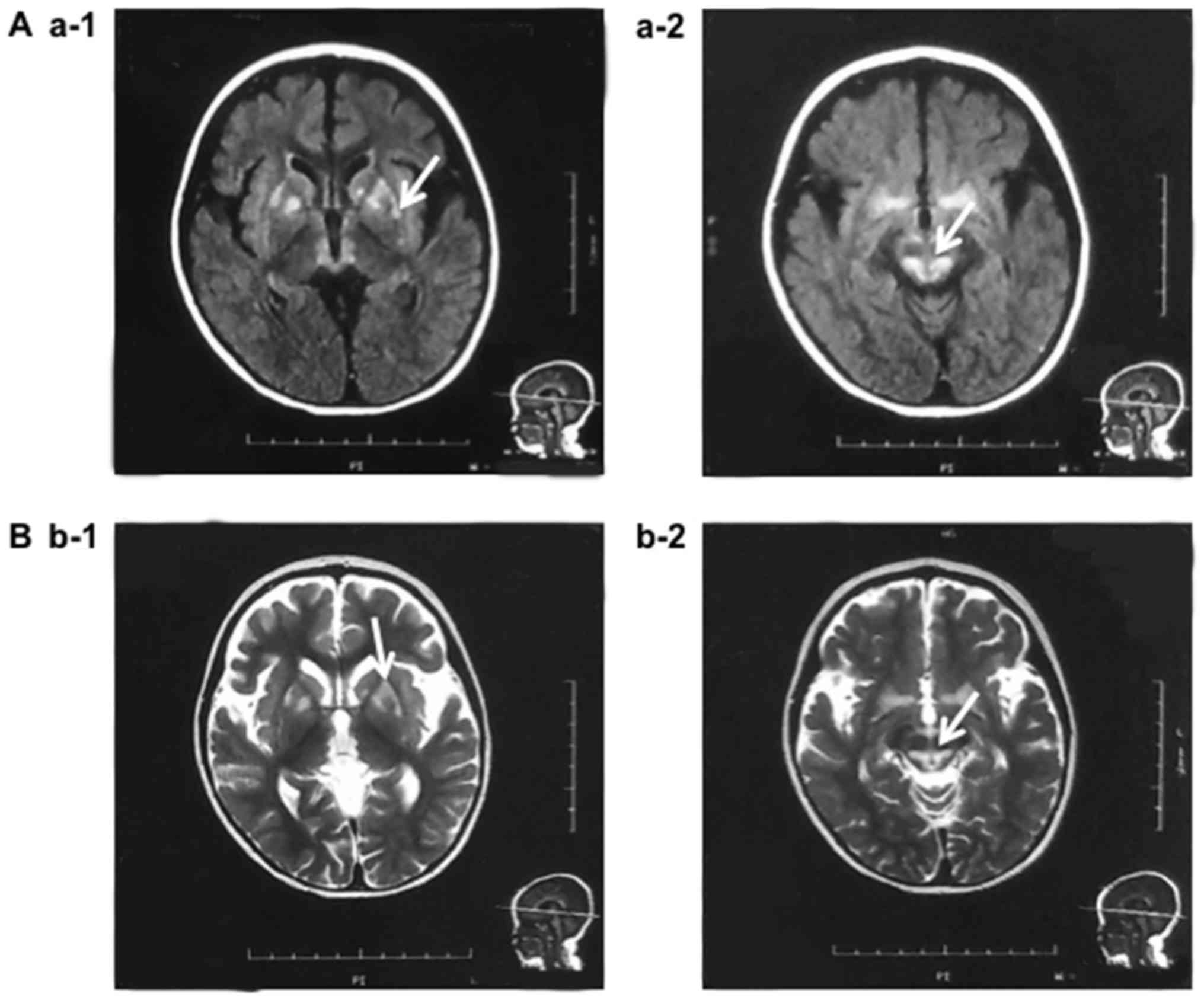
|
|
2
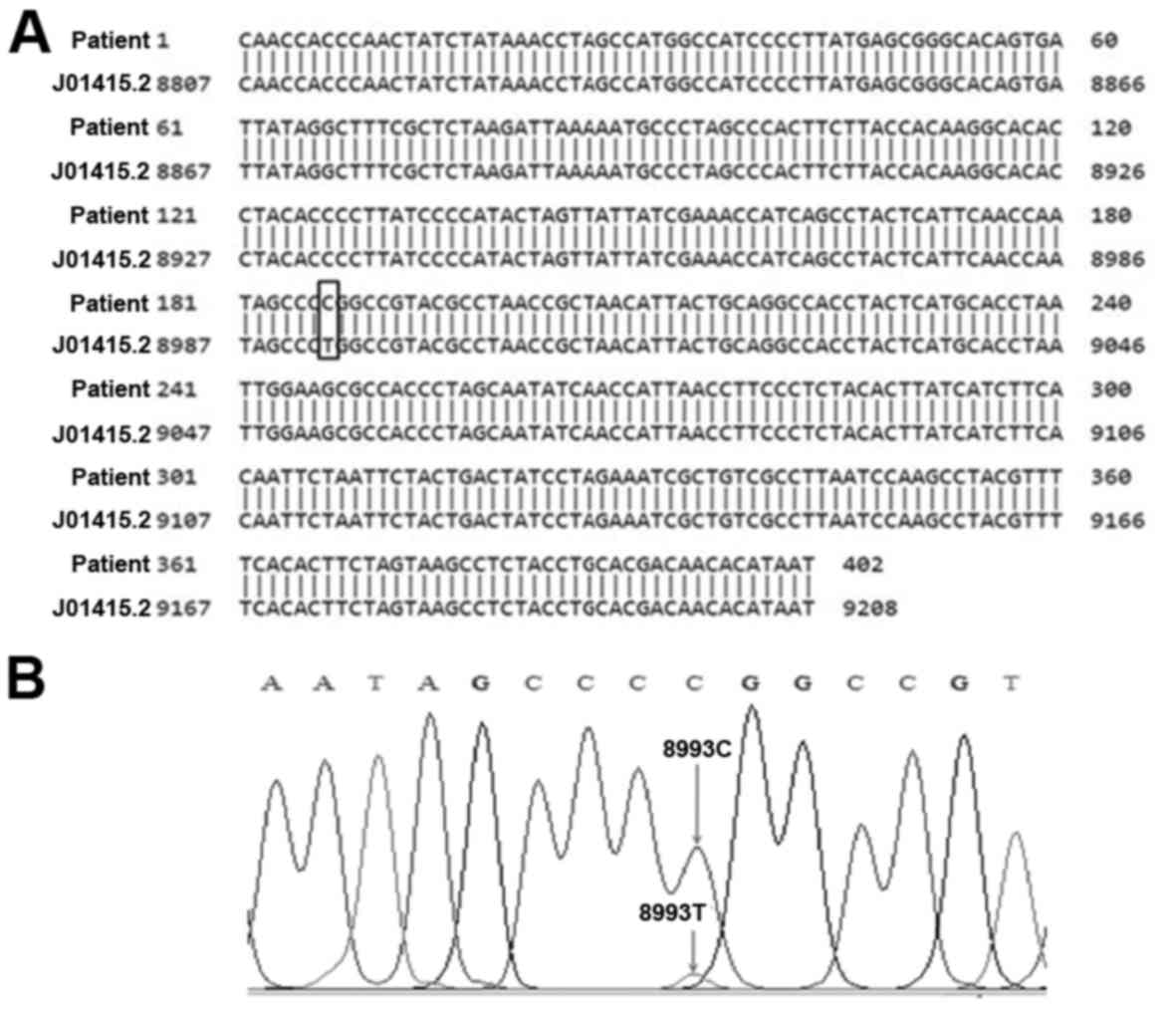
|
Piao YS, Tang GC, Yang H and Lu DH:
Clinico-neuropathological study of a Chinese case of familial adult
Leigh syndrome. Neuropathology. 26:218–221. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
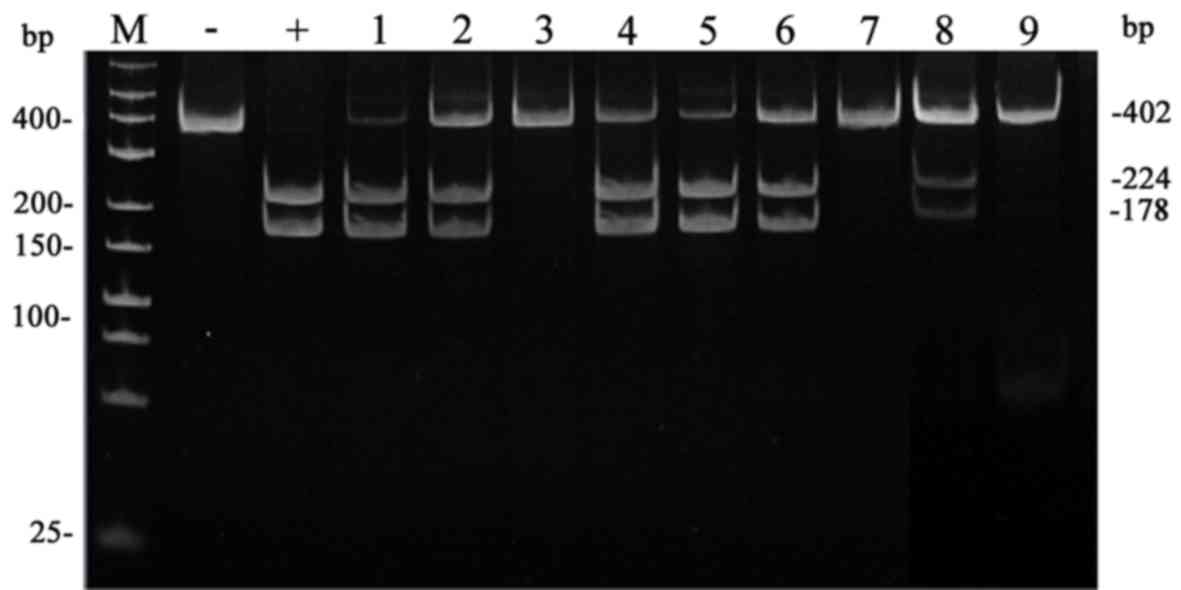
3
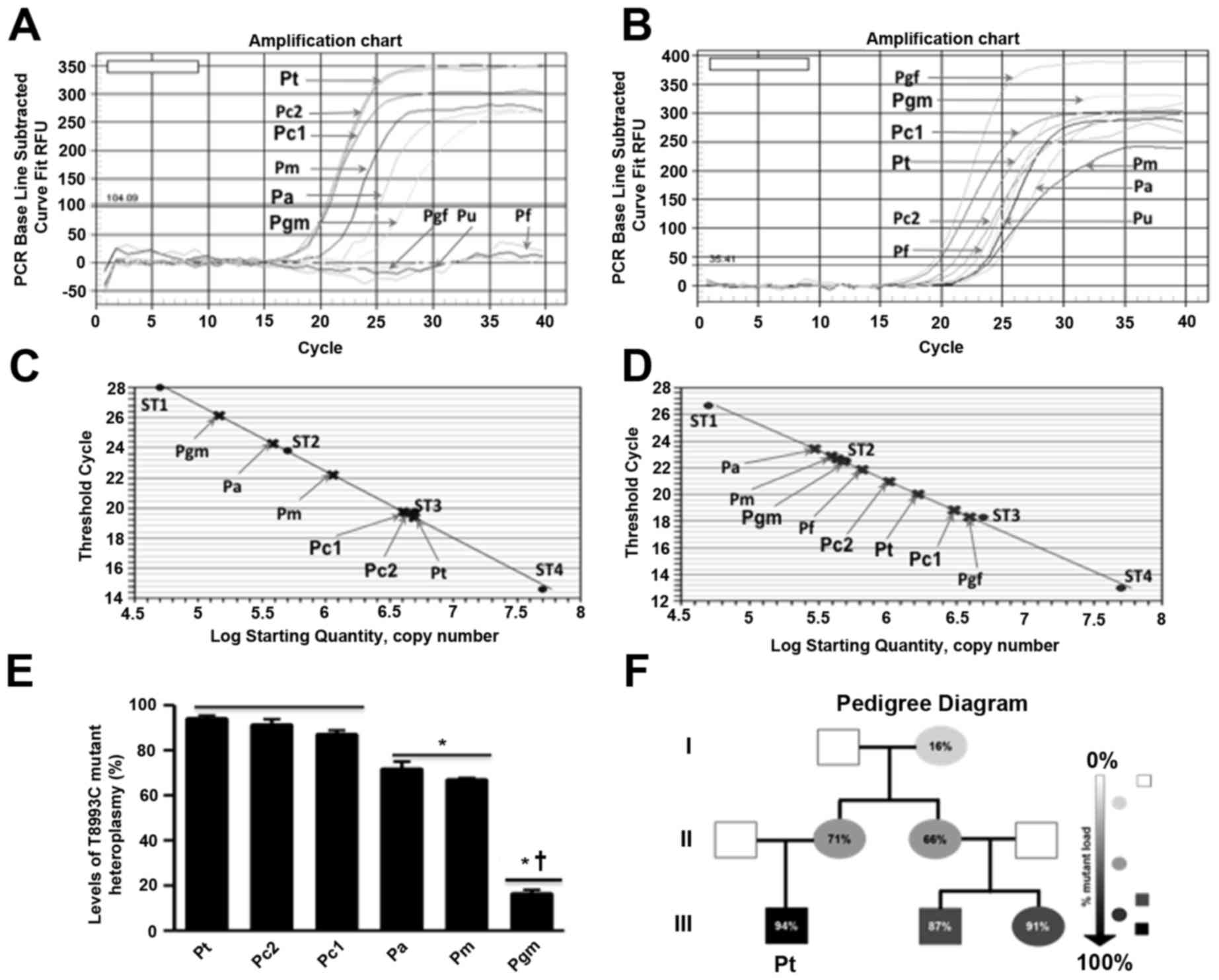
|
Finsterer J: Leigh and leigh-like syndrome
in children and adults. Pediatr Neurol. 39:223–235. 2008.
View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Thorburn DR, Rahman J and Rahman S:
Mitochondrial DNA-associated Leigh syndrome and NARPAdam MP,
Ardinger HH, Pagon RA, Wallace SE, Bean LJH, Stephens K and Amemiya
A: Source GeneReviews® [Internet]. University of
Washington; Seattle, WA: pp. 1993–2018
|
|
5
|
Piekutowska-Abramczuk D: The molecular
background of Leigh syndrome. Neurol Neurochir Pol. 42:238–250.
2008.(In Polish). PubMed/NCBI
|
|
6
|
White SL, Shanske S, McGill JJ, Mountain
H, Geraghty MT, DiMauro S, Dahl HH and Thorburn DR: Mitochondrial
DNA mutations at nucleotide 8993 show a lack of tissue- or
age-related variation. J Inherit Metab Dis. 22:899–914. 1999.
View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Bonfante E, Koenig MK, Adejumo RB,
Perinjelil V and Riascos RF: The neuroimaging of Leigh syndrome:
Case series and review of the literature. Pediatr Radiol.
46:443–451. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Santorelli FM, Shanske S, Macaya A, DeVivo
DC and DiMauro S: The mutation at nt 8993 of mitochondrial DNA is a
common cause of Leigh's syndrome. Ann Neurol. 34:827–834. 1993.
View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Makino M, Horai S, Goto Y and Nonaka I:
Mitochondrial DNA mutations in Leigh syndrome and their
phylogenetic implications. J Hum Genet. 45:69–75. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Santorelli FM, Shanske S, Jain KD, Tick D,
Schon EA and DiMauro S: A T->C mutation at nt 8993 of
mitochondrial DNA in a child with Leigh syndrome. Neurology.
44:972–974. 1994. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Morava E, Rodenburg RJ, Hol F, de Vries M,
Janssen A, van den Heuvel L, Nijtmans L and Smeitink J: Clinical
and biochemical characteristics in patients with a high mutant load
of the mitochondrial T8993G/C mutations. Am J Med Genet A.
140A:863–868. 2006. View Article : Google Scholar
|
|
12
|
Tatuch Y, Pagon RA, Vlcek B, Roberts R,
Korson M and Robinson BH: The 8993 mtDNA mutation: Heteroplasmy and
clinical presentation in three families. Eur J Hum Genet. 2:35–43.
1994. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Baracca A, Sgarbi G, Mattiazzi M, Casalena
G, Pagnotta E, Valentino ML, Moggio M, Lenaz G, Carelli V and
Solaini G: Biochemical phenotypes associated with the mitochondrial
ATP6 gene mutations at nt8993. Biochim Biophys Acta. 1767:913–919.
2007. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Huntsman RJ, Sinclair DB, Bhargava R and
Chan A: Atypical presentations of Leigh syndrome: A case series and
review. Pediatr Radiol. 32:334–340. 2004.
|
|
15
|
Bakshi R, Ariyaratana S, Benedict RH and
Jacobs L: Fluid-attenuated inversion recovery magnetic resonance
imaging detects cortical and juxtacortical multiple sclerosis
lesions. Arch Neurol. 58:742–748. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Truong HT, Nguyen TVA, Nguyen LV, Pham VA
and Phan TN: Screening of common point-mutations and discovery of
new T14727C change in mitochondrial genome of Vietnamese
encephalomyopathy patients. Mitochondrial DNA A DNA Mapp Seq Anal.
27:441–448. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Truong HT, Nguyen TVA, Nguyen THL, Pham VA
and Phan TN: Sensitive quantification of mitochondrial mutation
using new Taqman probes. Cent Eur J Med. 9:839–848. 2014.
|
|
18
|
Kumagai R, Ichikawa K, Yasui T, Kageyama Y
and Miyabayashi S: Adult Leigh syndrome: Treatment with intravenous
soybean oil for acute central respiratory failure. Eur J Neurol.
6:613–615. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Ruhoy IS and Saneto RP: The genetics of
Leigh syndrome and its implications for clinical practice and risk
management. Appl Clin Genet. 7:221–234. 2014.PubMed/NCBI
|
|
20
|
Makino M, Horai S, Goto Y and Nonaka I:
Confirmation that a T-to-C mutation at 9176 in mitochondrial DNA is
an additional candidate mutation for Leigh's syndrome. Neuromuscul
Disord. 8:149–151. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Enns GM, Bai RK, Beck AE and Wong LJ:
Clinical correlations in a family with variable tissue
mitochondrial DNA T8993G mutant load. Mol Genet Metab. 88:364–371.
2006. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Debray FG, Lambert M, Lortie A, Vanasse M
and Mitchell GA: Long-term outcome of Leigh syndrome caused by the
NARP-T8993C mtDNA mutation. Am J Med Genet A. 143A:2046–2051. 2007.
View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Fujii T, Hattori H, Higuchi Y and Tsuji M:
Phenotypic differences between T->C and T->G mutations at nt
8993 of mitochondrial DNA in Leigh syndrome. Pediatr Neurol.
18:275–277. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Pallotti F, Baracca A, Hernandez-Rosa E,
Walker WF, Solaini G, Lenaz G, Melzi D'Eril GV, Dimauro S, Schon EA
and Davidson MM: Biochemical analysis of respiratory function in
cybrid cell lines harbouring mitochondrial DNA mutations. Biochem
J. 384:287–293. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Baracca A, Barogi S, Carelli V, Lenaz G
and Solaini G: Catalytic activities of mitochondrial ATP synthase
in patients with mitochondrial DNA T8993G mutation in the ATPase 6
gene encoding subunit a. J Biol Chem. 275:4177–4182. 2000.
View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Dahl HH, Thorburn DR and White SL: Towards
reliable prenatal diagnosis of mtDNA point mutations: Studies of
nt8993 mutations in oocytes, fetal tissues, children and adults.
Hum Reprod. 15 Suppl 2:S246–S255. 2000. View Article : Google Scholar
|
|
27
|
St John JC, Facucho-Oliveira J, Jiang Y,
Kelly R and Salah R: Mitochondrial DNA transmission, replication
and inheritance: A journey from the gamete through the embryo and
into offspring and embryonic stem cells. Hum Reprod Update.
16:488–509. 2010. View Article : Google Scholar : PubMed/NCBI
|