Introduction
Deep vein thrombosis (DVT) is a disorder which is
characterized by abnormal blood clotting in deep veins, eventually
leading to venous return obstruction and luminal occlusion. The
incidence of DVT is relatively high in lower limb veins, and
particularly in the femoral vein (1). The prevalence of DVT is relative
higher in men compared with women and it significantly increases
with age (2). It has been reported
that 20–50% of patients develop post-thrombotic syndrome (PTS)
following the initial onset of DVT (3,4). In
severe cases, PTS can be accompanied by persistent symptoms, such
as edema, heaviness, pigmentation, pain and even venous ulcers.
Furthermore, DVT poses a life-threatening risk when the clot
dislodges to promote the development of pulmonary embolism (PE),
thus resulting in sudden heart failure with potentially fatal
outcomes (4). Catheter-directed
thrombolysis is a procedure that involves the use of a catheter to
directly deliver drugs into the blood clot in order to dissolve it.
This treatment is commonly used to treat DVT and PE (5). Therefore, investigating the molecular
mechanisms underlying DVT pathogenesis, searching for novel
biological therapies and precise biomarkers for the early diagnosis
of DVT and establishing reliable prognostic indicators are of great
importance. Such efforts will not only advance the clinical
diagnostics and treatment of DVT, but also hold promise for future
advancements in this field.
Emerging evidence has suggested that thrombosis is
commonly affected by three major factors, namely vascular wall
injury, alterations in blood flow and abnormalities in blood
composition (6). Among these,
vascular wall injury primarily involves the injury of endothelial
cells lining the blood vessels. Vascular endothelial cell damage
encompasses various processes, including apoptosis, which is
recognized as a critical contributor of venous thrombosis.
Extensive research has substantiated the close association between
vascular endothelial cell injury and the onset and progression of
DVT (7). A previous study
indicated that the apoptosis of vascular endothelial cells could
result in reduced levels of vasoactive substances, and impaired
defense mechanisms and stability of endothelial cells (8). These multifaceted consequences could
markedly affect the pathogenesis of DVT.
Murine double minute-2 (MDM2), an E3 ubiquitin
ligase, plays a crucial role in regulating the stability and
activity of p53 (9). In addition
to its role as an oncogene, emerging evidence has indicated that
MDM2 is also involved in the development of cardiovascular diseases
(10). A previous study
demonstrated that MDM2 upregulation promotes susceptibility to
ischemia-induced neuronal apoptosis (11). Furthermore, MDM2 is upregulated in
human atherosclerotic tissue and is associated with vascular cell
proliferation and inflammation (12). Notably, other studies revealed that
MDM2 not only promotes the induction of vascular calcification via
ubiquitinating histone deacetylases, but it can also enhance
mitochondrial injury in endothelial cells and trigger inflammatory
responses elicited by oxidized low-density lipoproteins (ox-LDL)
(13,14). Furthermore, MDM2 can promote
vascular endothelial growth factor expression, thus enhancing
cancer cell survival and angiogenesis in human neuroblastoma cell
lines (15). In terms of DVT, a
previous study revealed that MDM2 is upregulated in patients with
DVT and mouse models, while MDM2 downregulation can inhibit
thrombosis by promoting the migration, invasion and angiogenesis of
endothelial progenitor cells (EPCs) (16). The aforementioned findings
underscore the crucial role of MDM2 in DVT pathogenesis via
modulating the functions of EPCs.
Phosphatase and tensin homolog (PTEN), a tumor
suppressor gene located on chromosome 10q23, acts as a phosphatase
and is involved in regulating several cellular processes, including
cell proliferation, invasion, migration and apoptosis via
dephosphorylation (17). PTEN can
modulate the migration and proliferation of vascular smooth muscle
cells to aggravate atherosclerosis (18). Another study indicates that PTEN
can play a significant role in integrin b3-mediated amelioration of
cardiomyocyte damage due to hypoxia (19). In addition, the expression levels
of PTEN in the blood of patients who have undergone coronary artery
bypass grafting surgery can serve as a significant marker of
coronary heart disease (20).
Additionally, PTEN is found to modulate the activation of several
signaling pathways involved in disease progression, such as the
phosphoinositide 3-kinase (PI3K)/protein kinase B (AKT), Janus
kinase (JAK)/signal transducer and activator of transcription
(STAT), focal adhesion kinase (FAK) and, more recently,
extracellular signal-regulated kinase (ERK)1/2 pathways (21,22).
The JAK/STAT signaling pathway plays a crucial role in regulating
cell development, differentiation, proliferation and apoptosis
(23). Notably, the abnormal
expression of molecules involved in the JAK/STAT signaling pathway
is also involved in the formation of venous thrombosis (24).
The JAK/STAT pathway is a classic intracellular
signaling pathway, which is involved in regulating several
biological processes (25). This
pathway plays a significant role in numerous diseases. In terms of
cardiovascular diseases, the JAK/STAT pathway serves a significant
regulatory role (26). More
specifically, a study demonstrates that small molecule active
substances extracted from Buyang Huanwu Decoction can inhibit
atherosclerotic inflammation through JAK/STAT signaling (27). In addition, baicalin can regulate
macrophage polarization and ameliorate myocardial
ischemia-reperfusion injury via the JAK/STAT pathway (28). The JAK/STAT pathway is involved in
the onset of coronary artery diseases (29). Ma et al (30) demonstrate that diosmin can affect
the JAK/STAT pathway to inhibit vascular endothelial cell
apoptosis, thus improving DVT. The aforementioned studies verified
that the JAK/STAT pathway is one of the most significant pathways
involved in regulating the course of cardiovascular diseases,
including DVT.
Although MDM2 and PTEN exhibit distinct functions
and mechanisms, they interact during tumorigenesis and disease
progression. MDM2 could enhance tumor cell proliferation and
survival via regulating PTEN (31). However, the regulatory association
between MDM2 and PTEN in the context of DVT remains to be
elucidated. Given the respective roles of MDM2 and PTEN in DVT, it
is imperative to explore their regulatory interplay to gain deeper
insights into the pathogenesis of DVT. Therefore, the present study
aimed to investigate the regulatory association between MDM2 and
PTEN and their association with the development of DVT, thus
further enhancing our understanding of DVT pathogenesis. The
results of the current study could expand the current knowledge in
this area and offer a novel research direction for clinical
treatment strategies.
Materials and methods
Samples
Peripheral blood samples were obtained from patients
with DVT (n=5) and healthy subjects (n=5) during physical
examination between January and June 2023, with age ranging from 40
to 60 years. The sex distribution in the DVT group is 3 males and 2
females, while in the healthy control group, the sex ratio is 2
females to 3 males. Briefly, a total of 10 ml of peripheral blood
was isolated from subjects from both groups, and following
centrifugation at 800 g, 4°C for 10 min, the serum was isolated and
stored at −80°C. All patients provided written informed consent for
their enrollment in the present study, which was approved by the
Ethics Committee of the Fengyang County People's Hospital.
Cell culture
Human umbilical vein endothelial cells (HUVECs, cat.
no. CTCC-009-493), as immortalized cells, not primary cells, were
purchased from the Cell Bank of the Chinese Academy of Sciences and
cultured in Endothelial Cell Medium (ECM; cat. no. 1001; ScienCell
Research Laboratories, Inc.) supplemented with 10% FBS (cat. no.
10099; Gibco; Thermo Fisher Scientific, Inc.) and 0.5%
penicillin/streptomycin solution (cat. no. 15640055; Gibco; Thermo
Fisher Scientific, Inc.) at 37°C in an incubator with 5%
CO2. HUVECs were treated with ox-LDL at 37°C for 48 h
(40 µg/ml, cat. no. 20605ES10; YEASEN) to establish an in
vitro model.
Reverse transcription-quantitative
(RT-q) PCR
Total RNA was isolated from 5×105 cells
or 1.5 ml peripheral blood samples using a TRIzol®
reagent (cat. no. 15596018CN; Invitrogen; Thermo Fisher Scientific,
Inc.) according to the protocols. The quality of the isolated RNA
was then verified by UV spectrophotometry and formaldehyde
denaturing electrophoresis. Subsequently, a total of 1 µg RNA was
reverse transcribed into cDNA using AMV reverse transcriptase (cat.
no. 10109118001; Roche Diagnostics, Ltd.) according to the
manufacturer's protocols. The gene expression levels was amplified
by using the SYBR qPCR kit (cat. no. RK21203; ABclonal), and
normalized to GAPDH expression, were calculated using the
2−ΔΔCq method (32).
The PCR reaction consisted of pre-denaturation at 94°C for 5 min,
40 cycles of denaturation at 94°C for 30 sec, annealing at 58°C for
30 sec and extension at 72°C for 1 min. PCR was carried out using a
real-time amplifier (cat. no. ABI PRISM7700, Thermo Fisher). The
assays were performed in triplicate. The primer information was:
MDM2: 5′-ATGAAAGCCTGGCTCTGTGT-3 (Forward),
5′-CACTCTCCCCTGCCTGATAC-3′ (Reverse); PTEN:
5′-AGTTCCCTCAGCCGTTACCT-3 (Forward), 5′-AGGTTTCCTCTGGTCCTGGT-3′
(Reverse); and GAPDH: 5′-CAGCCTCAAGATCATCAGCA-3 (Forward),
5′-TGTGGTCATGAGTCCTTCCA-3′ (Reverse).
Cell transfection
Prior transfection, cells were seeded into 24-well
plates and cultured until they reached ~30% confluence. For short
interfering (si)RNA transfection, 0.67 µg (50 pmol) siRNAs (Sangon
Biotech Co., Ltd.) were diluted in the appropriate serum-free
diluent at a final volume of 25 µl. Subsequently, 1 µl
Entranster-R4000 (cat. no. 4000-3; Engreen Biosystem, Co., Ltd.)
was mixed with 24 µl serum-free diluent to a final volume of 25 µl.
The Entranster-R4000 diluent was left at room temperature for 5
min. Then, the Entranster-R4000 and RNA diluents were thoroughly
mixed by oscillating with an oscillator or blowing with a sampler
for >10 times. The resulting transfection complex (50 µl)
supplemented with 0.45 ml of complete medium was added into each
well. The petri dish was gently moved back and forth to ensure even
distribution. Cell morphology was observed at 6 h after
transfection and when cell viability was unaffected, this indicated
that the transfection reagent did not exhibit toxicity to the cells
and the medium was not changed. Cells were then cultured for 24–96
h at 37°C to obtain the desired results. The interference sequence
were as follows: si-MDM2: SS sequence: GGAACUUGGUAGUAGUCAAUC, AS
sequence: UUGACUACUACCAAGUUCCUG; si-PTEN: SS sequence:
AGAUGUUAGUGACAAUGAACC, AS sequence: UUCAUUGUCACUAACAUCUGG;
si-negative control (NC): SS sequence: UUCUCCGAACGUGUCACGU, AS
sequence: ACGUGACACGUUCGGAGAA.
Clone formation assay
Cells were seeded in a 6-well plate at a density of
700 cells per well in complete medium. The cultures were maintained
until the majority of single colonies reach a cell count of >50
cells/colony. The medium was changed every three days.
Subsequently, cells were washed once with PBS and fixed with 4%
paraformaldehyde (1 ml/well; cat. no. P1110; Beijing Solarbio
Science & Technology Co., Ltd.) for 30 min at room temperature,
followed by staining with crystal violet solution (1 ml/well cat.
no. C0121; Beyotime Institute of Biotechnology) for 10 min at room
temperature. Following washing with PBS (cat. no. 10010023; Gibco;
Thermo Fisher Scientific, Inc.), cells were allowed to air-dry.
Wound healing assay
Cells were inoculated into a 6-well plate at a
density of 5×105 cells/well. The following day, a
scratch was made using a sterile pipette tip (200 µl, cat. no.
BS-200-T; Biosharp). The cells were then washed three times with
PBS and supplemented with serum-free ECM. Finally, cells were
cultured in an incubator at 37°C with 5% CO2 for 0, 6,
12 and 24 h and observed under an optical light microscope (cat.
no. CKX41, Olympus). Observe under 200× magnification and randomly
select 3 fields of view for photography and counting.
Transwell assay
A total of 1×105 cells were re-suspended
in serum-free ECM and were then added onto the upper chamber of the
Transwell insert (cat. no. 14141; Beijing Labselect). Medium
containing 10% FBS was supplemented into the lower chamber and
cells were cultured for 48 h at 37°C. The cells were subsequently
fixed with 70% methanol for 10 min at room temperature (cat. no.
322415; MilliporeSigma) and stained with 1% crystal violet for 5
min at room temperature. The invasive cells were counted at five
randomly selected fields under an optical light microscope (cat.
no. CKX41, Olympus). Observe under 100× magnification and randomly
select 3 fields of view for photography and counting.
Flow cytometry
Cell apoptosis was assessed using an Annexin
V-FITC/PI Kit (cat. no. 40302ES20; Shanghai Yeasen Biotechnology
Co., Ltd.). Cells were collected, mixed with 5 µl Annexin V for 30
min at 37°C, then incubated with propidium iodide in the dark for
20 min at 37°C. Apoptotic cells were counted using flow cytometry
(CytoFLEX LX; Beckman Coulter). Analyze the data using Flowjo
software (Version 10.8; flowjo.com/; BD Biosciences). Combine the
proportion of early apoptotic cells (Annexin V single positive) and
late apoptotic cells were considered apoptotic cell proportion.
Angiogenesis assay
Angiogenesis was evaluated using an Angiogenesis
Assay Kit (In Vitro; cat. no. ab204726; Abcam). A 96-well culture
plate was coated with an extracellular matrix solution and
incubated at 37°C for 1 h to allow gel formation. Subsequently,
70,000 cells were seeded onto the gel and cultured for an
additional 18 h. After the incubation medium was removed, the
cells/gel were washed. The formation of blood vessels was then
evaluated under a light microscope (cat. no. CKX41, Olympus).
Observe under 200× magnification and randomly select 3 fields of
view for photography and counting.
Co-immunoprecipitation assays
5×105 cells in a petri dish were lysed
with the corresponding lysis buffer (cat. no. 20-188; Merck
Millipore) with a protease inhibitor (cat. no. P8340;
MilliporeSigma) on ice for 30 min. After centrifugation at 2,000 g
at 4°C in the maximum rotating speed for 30 min, supernatant was
collected. A small portion of the lysate was subjected to western
blot analysis, while the remaining lysate was mixed with 2 µg of
the corresponding antibody and incubated at 4°C overnight. To
prepare the protein A agarose beads (cat. no. P1925;
MilliporeSigma), 10 µl of the solution/beads was washed three times
with cracking buffer (cat. no. 20-188; Merck Millipore), followed
by centrifugation at 1,000 g for 3 min each time at 4°C. A total of
10 µl pre-treated protein A agarose beads was added to the cell
lysate, which was incubated with 2 µg MDM2 antibody (cat. no.
33-7100; Thermo Fisher) overnight, and the mixture was gently
shaken at 4°C for 2–4 h. The aforementioned procedure allowed the
coupling between the antibody and protein A agarose beads.
Following immunoprecipitation, the agarose beads were centrifuged
at 4°C for 3 min at 1,000 × g. After beads were pelleted, the
supernatant was carefully aspirated and the agarose beads were
washed with 100 µl Elution buffer (cat. no. P2179S; Beyotime
Institute of Biotechnology) for 3–4 times. Lastly, the dilution was
then supplemented with 100 µl 2X SDS loading buffer (cat. no. 9172;
Takara Biotechnology Co., Ltd.) and the mixture was boiled for 5
min prior western blot analysis.
Western blot analysis
Proteins were extracted from cells using RIPA lysis
buffer (cat. no. P0013B; Beyotime Institute of Biotechnology) and
protein concentration was quantified using a BCA kit (cat. no.
P0011; Beyotime Institute of Biotechnology). A total of 30 µg total
protein extracts were separated by 10% SDS-PAGE and were then
transferred to PVDF membranes (cat. no. IPVH00010; MilliporeSigma).
Subsequently, the membranes were blocked with 5% skimmed milk (cat.
no. P0216; Beyotime Institute of Biotechnology) at 4°C for 2 h and
then with primary antibodies at 4°C overnight. Following washing
with PBS-1% Tween-20 (PBST; cat. no. BL314B; Biosharp Life
Sciences) for three times, the membrane was incubated for 2 h with
the corresponding secondary antibody. After washing with PBST for
three times, the protein bands were visualized using ECL
Chemiluminescent buffer (cat. no. 36208ES76; YEASEN) in a dark
room. The grayscale values were calculated using ImageJ software
(Version 1.8.0; National Institutes of Health). The following
primary antibodies were used: Anti-MDM2 (cat. no. ab16895),
anti-PTEN (cat. no. ab32199), anti-phosphorylated (p)-JAK1 (cat.
no. ab138005), anti-JAK1 (cat. no. ab133666), anti-p-STAT3 (cat.
no. ab76315), anti GAPDH (cat. no. ab8245) and anti-STAT (cat. no.
ab68153; all from Abcam). In addition, the HRP anti-rabbit IgG
antibody (cat. no. ab288151; Abcam) served as a secondary
antibody.
Bioinformatics analysis
Search Tool for the Retrieval of Interacting
Genes/Proteins (STRING) database (string-db.org/) was used to
verify the association between MDM2 and PTEN.
Statistical analysis
All statistical analyses were performed using
GraphPad prism 6.0 (Dotmatics). The experiments were independently
repeated at least three times. The results are expressed as the
mean ± standard error of the mean. The differences between two
groups were compared using unpaired Student's t-test, while those
among multiple groups by ANOVA followed by Tukey's post hoc test.
P<0.05 was considered to indicate a statistically significant
difference.
Results
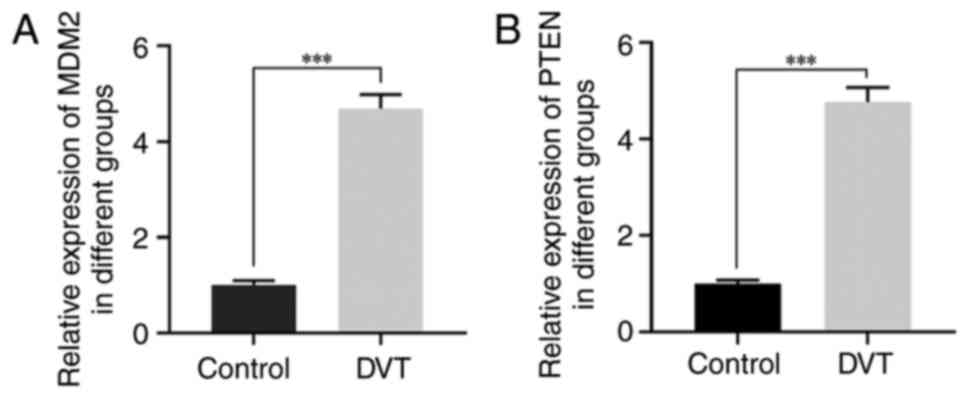
Expression of MDM2 and PTEN in venous
blood samples from patients with DVT
To investigate the involvement of MDM2 and PTEN in
DVT, RT-qPCR analysis was performed to detect their expression
levels in venous blood samples obtained from patients with DVT. The
participants were allocated into two groups, namely the control and
DVT groups. The results revealed that MDM2 and PTEN were markedly
upregulated in the intravenous blood samples of patients with DVT
compared with the control group (Fig.
1A and B). These results strongly supported the potential
significance of MDM2 and PTEN in the pathogenesis of DVT.
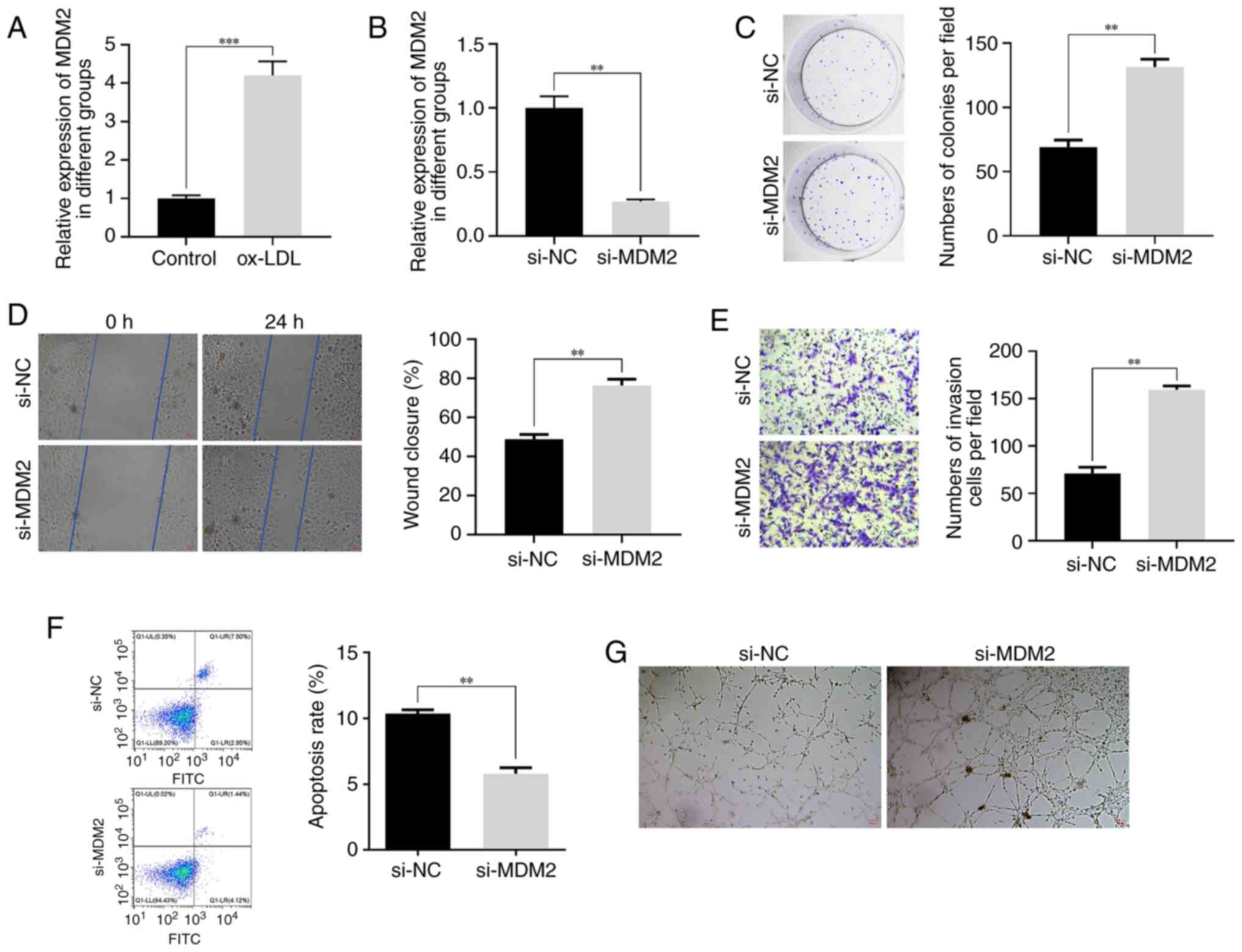
Effect of MDM2 silencing on
ox-LDL-treated HUVECs
To investigate the role of MDM2 in the development
of DVT, an in vitro model was established. The results
demonstrated that HUVECs treatment with ox-LDL significantly
upregulated MDM2 (Fig. 2A). To
further elucidate the functional significance of MDM2 in different
cellular behaviors, the siRNA-mediated knockdown approach was
employed in HUVECs (Fig. 2B).
Notably, MDM2 knockdown not only promoted the proliferation of
ox-LDL-treated HUVECs (Fig. 2C),
but also markedly enhanced their migration and invasion abilities
(Fig. 2D and E). The
aforementioned findings strongly suggested that MDM2 could play a
crucial role in facilitating cell metastasis and invasion during
DVT progression. In addition, the results showed that MDM2
silencing suppressed the apoptosis of ox-LDL-treated HUVECs. More
particularly, cell apoptosis was significantly reduced in the
si-MDM2 group compared with the control group (Fig. 2F). This finding indicated that MDM2
could modulate the delicate balance between cell survival and death
throughout DVT development. Furthermore, MDM2 silencing also
significantly augmented the angiogenic capacity of ox-LDL-treated
HUVECs. Therefore, tube formation assays demonstrated that cells in
the si-MDM2 group displayed a more pronounced vascular lumen
structure (Fig. 2G). Collectively,
these compelling findings underscored the critical involvement of
MDM2 in DVT pathogenesis and highlighted its potential therapeutic
value in this context.
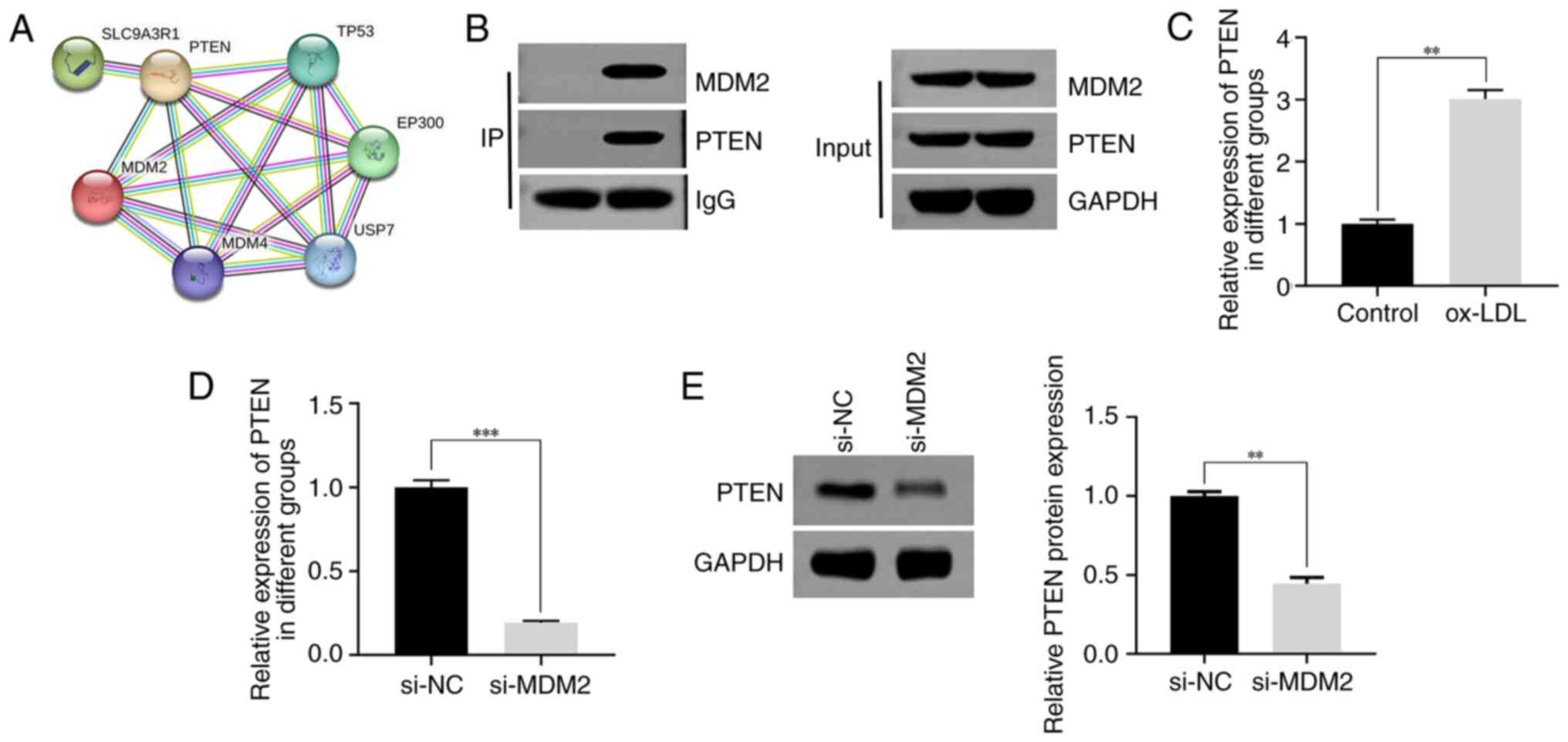
Interaction between MDM2 and PTEN
A previous study revealed that MDM2 interacts with
PTEN (33). In the present study,
bioinformatics analysis verified the association between MDM2 and
PTEN (Fig. 3A). To further
validate this finding, a co-immunoprecipitation assay was
performed, which verified the binding capacity between MDM2 and
PTEN (Fig. 3B). Subsequently, to
determine the expression levels of PTEN in different treatment
groups, RT-qPCR was employed. Therefore, the results demonstrated
that PTEN was notably upregulated in ox-LDL-treated HUVECs compared
with the control group (Fig. 3C).
To further investigate the effect of MDM2 knockdown on the mRNA and
protein expression levels of PTEN, RT-qPCR and western blot
analyses were performed, respectively. The results demonstrated a
significant reduction in the mRNA expression levels of PTEN in the
si-MDM2 group (Fig. 3D).
Consistently, western blot analysis further verified that the
protein expression levels of PTEN were markedly decreased following
MDM2 silencing (Fig. 3E). In
summary, the aforementioned findings provided compelling evidence
supporting the interaction between MDM2 and PTEN and highlighted
the effect of MDM2 knockdown on the mRNA and protein expression
levels of PTEN.
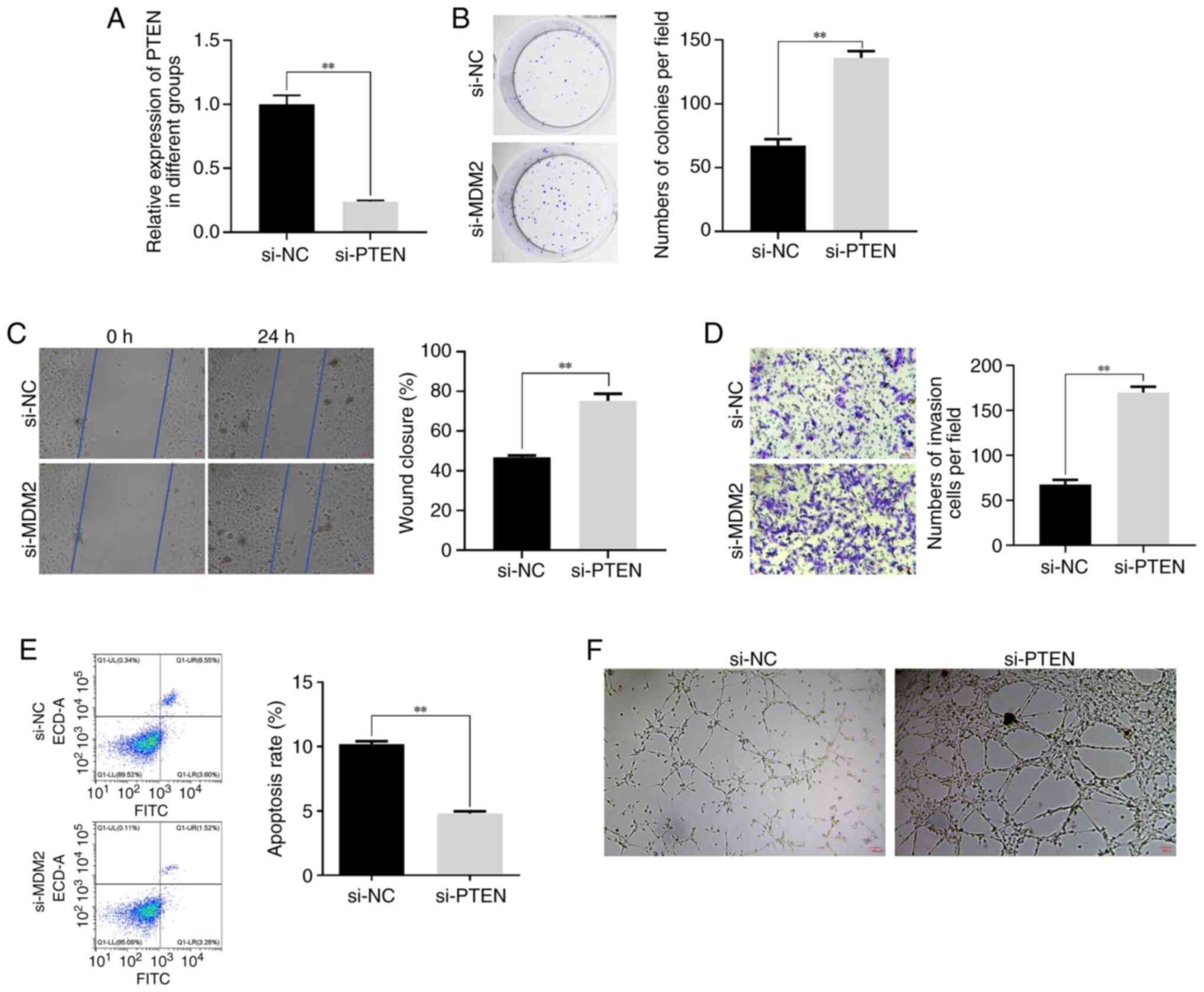
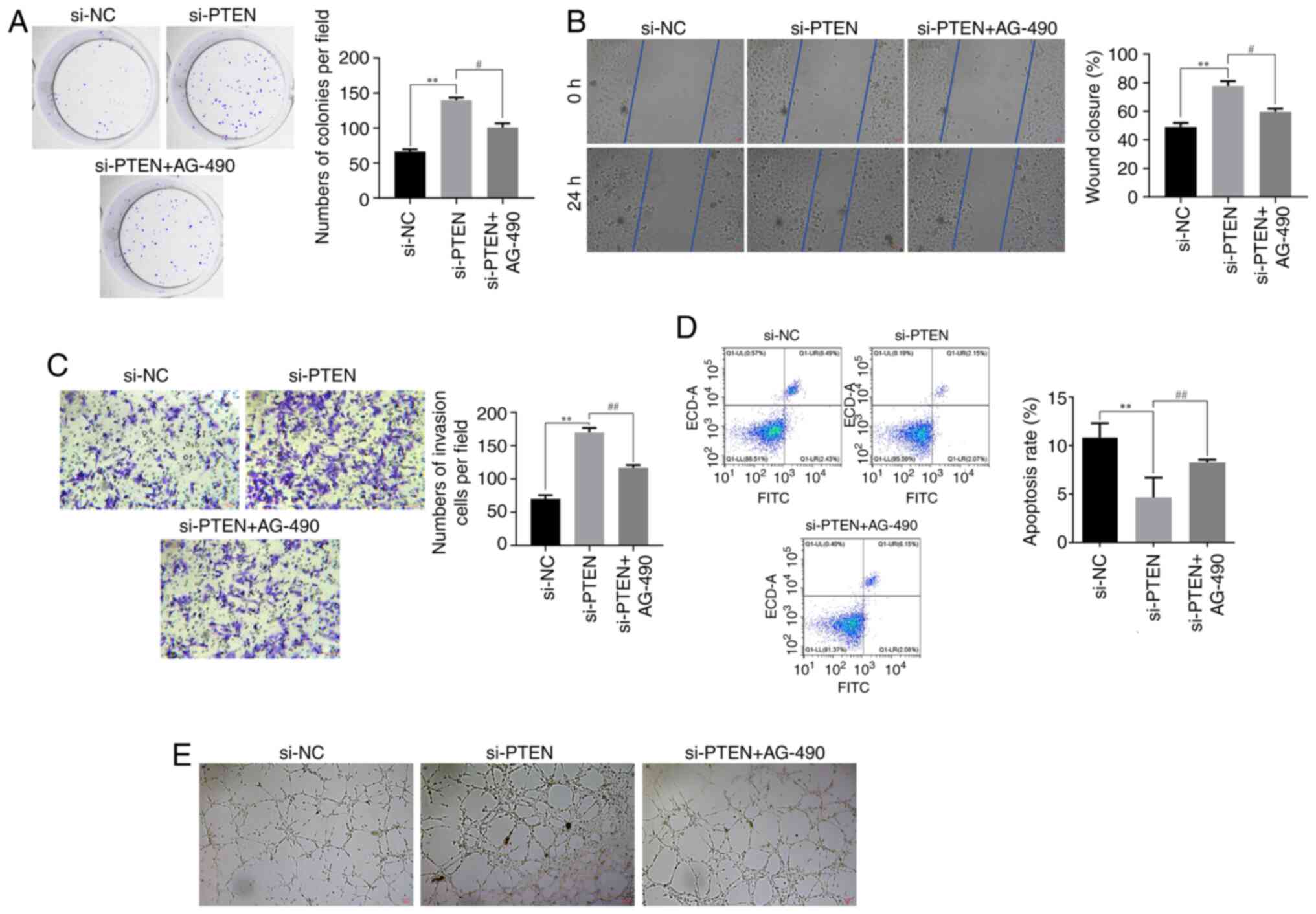
Effect of PTEN silencing on
ox-LDL-treated HUVECs
Subsequently, the current study aimed to investigate
the role of PTEN in DVT. Therefore, PTEN was knocked down in HUVECs
(Fig. 4A). Clone formation assay
revealed that PTEN silencing promoted the proliferation of
ox-LDL-treated HUVECs (Fig. 4B).
Furthermore, the wound healing and Transwell assays further
substantiated the promoting effect of PTEN knockdown on HUVECs
migration and invasion (Fig. 4C and
D). More particularly, the migration and invasion abilities of
HUVECs were markedly enhanced in the PTEN silencing group compared
with the control group. Additionally, flow cytometry demonstrated
that PTEN silencing suppressed the apoptosis of ox-LDL-induced
HUVECs (Fig. 4E). Lastly, tube
formation assays showed that the angiogenic capability of
ox-LDL-treated HUVECs was increased in PTEN-depleted cells
(Fig. 4F). Overall, the
aforementioned results supported the pleiotropic effects of PTEN
silencing on the behavior of HUVECs, including cell proliferation,
migration, invasion, apoptosis and angiogenesis. These findings,
combined with the effect of MDM2 silencing on PTEN expression,
further supported the strong association between PTEN and MDM2.
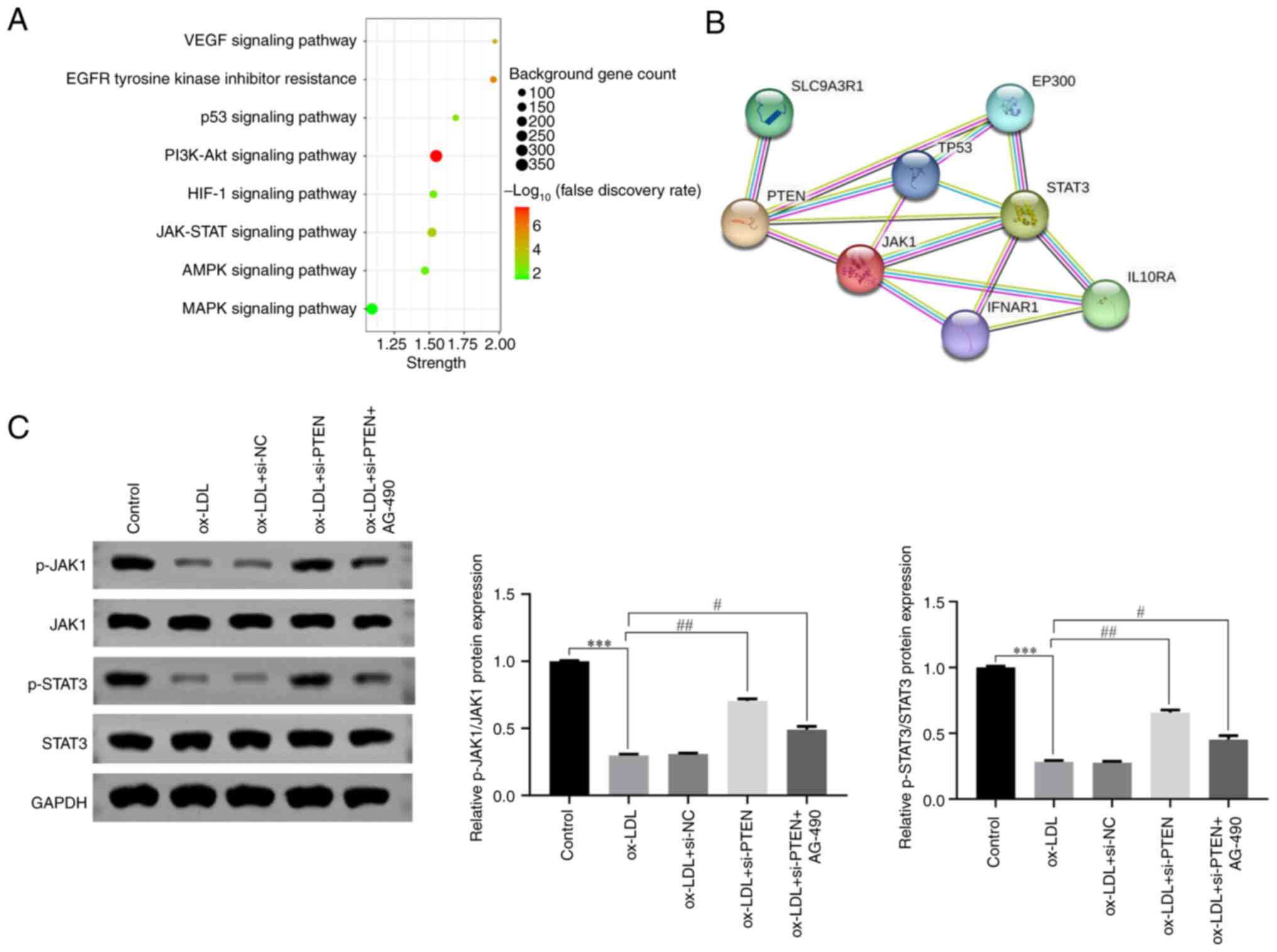
PTEN is involved in the pathogenesis
of DVT via inhibiting JAK/STAT signaling
Based on previous studies, Kyoto Encyclopedia of
Genes and Genomes (KEGG) analysis was performed to identify the
signaling pathways associated with PTEN expression (34). The analysis showed that PTEN could
regulate several crucial signaling pathways, including the JAK/STAT
signaling pathway (Fig. 5A). This
finding was further supported by STRING analysis, which further
revealed the interactions between PTEN and proteins involved in the
JAK/STAT signaling pathway (Fig.
5B). Furthermore, to elucidate the functional involvement of
PTEN in the JAK/STAT pathway, western blot analysis was conducted
to detect the expression levels of key proteins (p-JAK1, JAK1,
p-STAT3, STAT3) in different treatment groups. The results unveiled
that HUVECs treatment with ox-LDL significantly attenuated the
phosphorylation levels of JAK1 and STAT (Fig. 5C), thus suppressing the activity of
JAK/STAT signaling. Intriguingly, the JAK/STAT signaling pathway
was activated following PTEN silencing (Fig. 5C). To further validate the
aforementioned finding, cells were also treated with AG-490, a
specific inhibitor of the JAK/STAT pathway. As expected, HUVECs
treatment with AG-490 effectively inhibited the activation of
JAK/STAT signaling (Fig. 5C).
Collectively, these findings suggested that PTEN could serve a
significant role in DVT via modulating the JAK/STAT signaling
pathway.
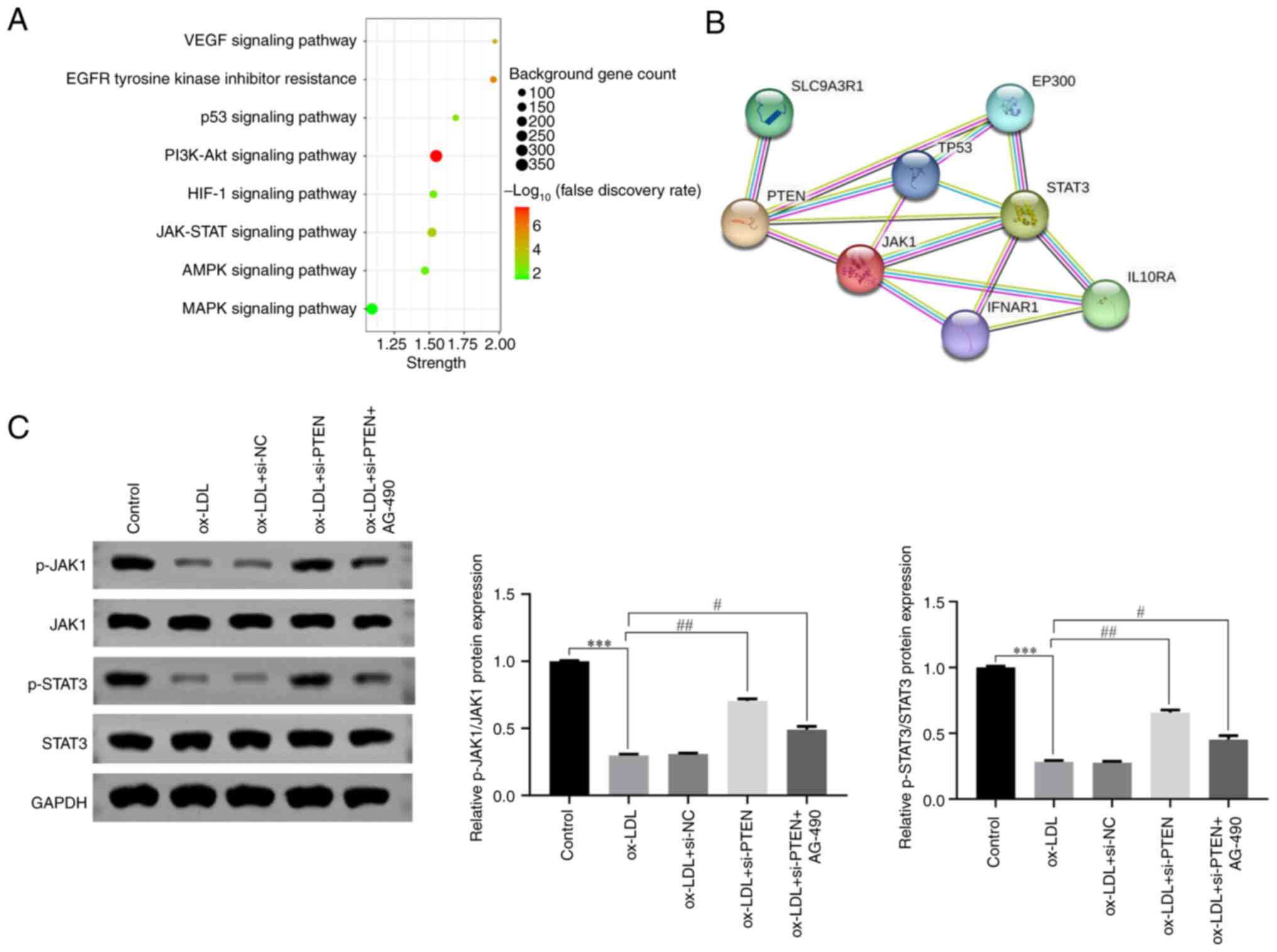 | Figure 5.PTEN participates in DVT by
inhibiting JAK/STAT signaling pathway. (A) PTEN gene-related
signaling pathways analyzed by KEGG. (B) The interaction between
PTEN and JAK/STAT pathways analyzed by STRING. (C) The expression
level of JAK/STAT signaling pathway associated proteins in HUVECs
treated with ox-LDL (40 µg/ml) detected by western blotting.
***P<0.001, #P<0.05, ##P<0.01. PTEN,
phosphatase and tensin homolog; DVT, deep vein thrombosis; JAK,
Janus kinase; STAT, signal transducer and activator of
transcription; STRING, Search Tool for the Retrieval of Interacting
Genes/Proteins; KEGG, Kyoto Encyclopedia of Genes and Genomes;
HUVECs, human umbilical vein endothelial cells; ox-LDL, oxidized
low-density lipoproteins; p-, phosphorylated; NC, negative
control. |
PTEN acts on ox-LDL-treated HUVECs via
by inhibiting the JAK/STAT signaling pathway
The aforementioned findings indicated that PTEN
could inhibit the JAK/STAT signaling pathway, thus affecting HUVECs
proliferation, migration, invasion, apoptosis and angiogenesis. The
results obtained from the clone formation assays revealed that PTEN
silencing could promote proliferation of ox-LDL-treated HUVECs.
However, the stimulatory effect of PTEN silencing was reversed
following cell treatment with AG-490 (Fig. 6A). Furthermore, the results
demonstrated that PTEN silencing enhanced the migratory and
invasive capabilities of HUVECs, as evidenced by the wound healing
and Transwell assays, respectively. Conversely, these effects were
notably diminished in AG-490-treated HUVECs (Fig. 6B and C). Additionally, flow
cytometry analysis further elucidated that PTEN knockdown reduced
the apoptosis of ox-LDL-treated HUVECs, which was also reversed by
AG-490 (Fig. 6D). In addition, the
tube formation assays revealed that PTEN silencing promoted the
vasculogenesis of HUVECs, which was counteracted by the presence of
AG-490 (Fig. 6E). These findings
further supported the role of PTEN in modulating the JAK/STAT
signaling pathway and its subsequent effects on the behavior of
HUVECs.
Discussion
DVT is a serious medical condition that occurs when
a blood clot is formed in one of the deep veins, typically in those
of the leg. If left untreated, DVT can lead to potentially
life-threatening complications (4). Markedly, the treatment approach for
patients with DVT may vary depending on individual factors,
including the extent and location of the clot, the presence of any
underlying genetic factors and the overall health of the patient.
Therefore, consulting with a healthcare professional for an
accurate diagnosis and individualized treatment plan for DVT is of
great importance.
Previous studies reveal that the expression levels
of MDM2 (16) and PTEN (35) were both increased in patients with
DVT. Consistent with this, in the present study, MDM2 and PTEN were
also upregulated in intravenous blood samples of patients with DVT.
HUVECs are commonly used to study the pathogenesis and treatment of
DVT. In the present study, ox-LDL-treated HUVECs were used as an
in vitro model of DVT to explore the effects of MDM2
knockdown on the development of DVT. Therefore, following HUVECs
treatment with ox-LDL, the expression levels of MDM2 were
increased, thus suggesting that the DVT in vitro model was
successfully established. Additionally, MDM2 silencing promoted the
proliferation, migration, invasion and angiogenic capacity of
HUVECs, and reduced apoptosis. These results indicated that MDM2
could display a critical role in the development of DVT via
regulating the delicate balance between cell survival and death
during DVT progression (16).
The STRING database is widely used to assess
protein-protein interactions (PPIs) (36). Therefore, this database is commonly
used to explore and analyze PPI networks, identify potential
interaction partners for a given protein and gain insights into
protein function and cellular processes (37). In the current study, bioinformatics
analysis using the STRING database showed that MDM2 could interact
with PTEN. Furthermore, the expression levels of PTEN were reduced
in MDM2-depleted HUVECs, thus supporting the positive regulatory
effect of MDM2 on PTEN expression. A study also demonstrates that
PTEN, a dual specificity phosphatase that antagonizes PI3K/AKT
signaling, can inhibit the nuclear translocation and destabilize
MDM2 (38).
Subsequently, the role of PTEN in DVT was
investigated. Suppressing PTEN could enhance HUVECs proliferation,
migration, invasion and angiogenic capacity, while inhibiting
apoptosis. These findings suggested that PTEN could serve a crucial
role in maintaining the intricate equilibrium between cell survival
and death during the progression of DVT (39). Furthermore, KEGG pathway analysis
revealed that the JAK/STAT signaling pathway was significantly
associated with PTEN. Additionally, PPI analysis also verified that
both JAK1 and STAT3, which are involved in the JAK/STAT signaling
pathway, could interact with PTEN. A previous study also showed
that JAK/STAT signaling can play a key role in the development of
DVT (40). In the present study,
the results demonstrated that JAK1 and STAT3 were downregulated in
ox-LDL-treated HUVECs. However, their expression levels were
reversed following PTEN silencing. These findings indicated that
PTEN could exert a negative regulatory effect on JAK/STAT
signaling. However, HUVECs treatment with AG-490, an inhibitor of
the JAK/STAT signaling pathway, abrogated the effect of PTEN
knockdown on expression levels of JAK1 and STAT3. Consistently, the
effects of PTEN silencing on cell proliferation, migration,
invasion, angiogenic capacity and apoptosis were also recovered by
AG-490. Altogether, these findings indicated that PTEN could play a
key role in DVT via modulating the JAK/STAT signaling pathway.
However, the aforementioned results are not consistent with those
reported in previous studies: A previous review details how
non-coding RNAs regulate the plasticity of endothelial cells by
modulating the PTEN and Hippo pathways, establishing a new
perspective on intercellular communication in physiological and
pathological angiogenesis processes (41). Non-coding RNAs play a regulatory
role in the process of DVT. A study indicates that miR-513c-5p
reduction-induced VEC pyroptosis is involved in the progression of
DVT and suggests a potential therapeutic strategy targeting the
miR-513c-5p/caspase-1/GSDMD signaling axis for DVT management
(42).
In conclusion, the present study demonstrated that
both MDM2 and PTEN were upregulated in patients with DVT, thus
providing novel insights into their potential collaborative role in
the development of DVT. More specifically, the results indicated
that MDM2 and PTEN can work together to inhibit endothelial cell
growth and promote the occurrence of DVT via suppressing the
JAK/STAT signaling pathway. However, the present study also has
certain limitations. The present research was limited to in
vitro cell levels and did not use animal models. At the same
time, experiments on overexpression systems were not performed,
that is, the present results indicated that inhibiting the JAK/STAT
pathway affected the proliferation of endothelial cells and
promoted DVT. However, the present study did not observe the
effects of activating the JAK/STAT pathway on the effect of PTEN
and MDM2 on DVT. In addition, ox-LDL mainly promotes thrombosis by
upregulating genes involved in the coagulation process and
enhancing the recruitment and adhesion of white blood cells to
endothelial cells (43). However,
these mechanisms were not investigated in the present study, which
is also one of its limitations. Furthermore, blood contains various
types of cells and the present study did not detect the expression
levels of MDM2 and PTEN after sorting out endothelial cells, but
rather directly measured the expression levels of MDM2 and PTEN in
the blood, which has certain limitations. Despite that, the results
were sufficient to verify the diagnostic significance of MDM2 and
PTEN in the management of DVT. The aforementioned results could
provide the theoretical basis for the future development of drugs
targeting both PTEN and MDM2 to significantly improve the condition
of thrombotic patients in the clinic.
Acknowledgements
Not applicable.
Funding
The present study was supported by the Project of Chuzhou County
Science and Technology Bureau (grant no. 2022ZN009).
Availability of data and materials
The data generated in the present study may be
requested from the corresponding author.
Authors' contributions
JJ conceived and designed the present study and
drafted the manuscript. DZ and JP performed the experiments and
data extraction. YL analyzed the data. All authors read and
approved the final manuscript. JJ, DZ, JP and YL confirm the
authenticity of all the raw data.
Ethics approval and consent to
participate
The experimental protocols were approved by the
Ethics Committee of Fengyang County People's Hospital.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
Glossary
Abbreviations
Abbreviations:
|
DVT
|
deep vein thrombosis
|
|
PTS
|
post-thrombotic syndrome
|
|
PE
|
pulmonary embolism
|
|
RT-q-PCR
|
reverse transcription-quantitative
PCR
|
|
JAK
|
Janus kinase
|
|
STAT
|
signal transducer and activator of
transcription
|
References
|
1
|
Bartholomew JR: Update on the management
of venous thromboembolism. Cleve Clin J Med. 84 (Suppl 3):S39–S46.
2017. View Article : Google Scholar
|
|
2
|
Lutsey PL and Zakai NA: Epidemiology and
prevention of venous thromboembolism. Nat Rev Cardiol. 20:248–262.
2023. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Giordano NJ, Jansson PS, Young MN, Hagan
KA and Kabrhel C: Epidemiology, pathophysiology, stratification,
and natural history of pulmonary embolism. Tech Vasc Interv Radiol.
20:135–140. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Boon G, Van Dam LF, Klok FA and Huisman
MV: Management and treatment of deep vein thrombosis in special
populations. Exp Rev Hematol. 11:685–695. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Kim KA, Choi SY and Kim R: Endovascular
treatment for lower extremity deep vein thrombosis: An overview.
Korean J Radiol. 22:931–943. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Goldhaber SZ and Bounameaux H: Pulmonary
embolism and deep vein thrombosis. Lancet. 379:1835–1846. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Ghosh N, Garg I, Srivastava S and Kumar B:
Influence of integrins on thrombus formation: A road leading to the
unravelling of DVT. Mol Cell Biochem. 476:1489–1504. 2021.
View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Jin J, Wang C, Ouyang Y and Zhang D:
Elevated miR-195-5p expression in deep vein thrombosis and
mechanism of action in the regulation of vascular endothelial cell
physiology. Exp Ther Med. 18:4617–4624. 2019.PubMed/NCBI
|
|
9
|
Wang W, Qin JJ, Rajaei M, Li X, Yu X, Hunt
C and Zhang R: Targeting MDM2 for novel molecular therapy: Beyond
oncology. Med Res Rev. 40:856–880. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Lam B and Roudier E: Considering the role
of murine double minute 2 in the cardiovascular system? Front Cell
Dev Biol. 7:3202019. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Rodríguez C, Ramos-Araque ME,
Domínguez-Martínez M, Sobrino T, Sánchez-Morán I, Agulla J,
Delgado-Esteban M, Gómez-Sánchez JC, Bolaños JP, Castillo J and
Almeida A: Single-Nucleotide polymorphism 309T>G in the MDM2
promoter determines functional outcome after stroke. Stroke.
49:2437–2444. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Hashimoto T, Ichiki T, Ikeda J,
Narabayashi E, Matsuura H, Miyazaki R, Inanaga K, Takeda K and
Sunagawa K: Inhibition of MDM2 attenuates neointimal hyperplasia
via suppression of vascular proliferation and inflammation.
Cardiovasc Res. 91:711–719. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Kwon DH, Eom GH, Ko JH, Shin S, Joung H,
Choe N, Nam YS, Min HK, Kook T, Yoon S, et al: MDM2 E3
ligase-mediated ubiquitination and degradation of HDAC1 in vascular
calcification. Nat Commun. 7:104922016. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Zeng Y, Xu J, Hua YQ, Peng Y and Xu XL:
MDM2 contributes to oxidized low-density lipoprotein-induced
inflammation through modulation of mitochondrial damage in
endothelial cells. Atherosclerosis. 305:1–9. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Zhou S, Gu L, He J, Zhang H and Zhou M:
MDM2 regulates vascular endothelial growth factor mRNA
stabilization in hypoxia. Mol Cell Biol. 31:4928–4937. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Lou Z, Ma H, Li X, Zhang F, Du K and Wang
B: Hsa_circ_0001020 accelerates the lower extremity deep vein
thrombosis via sponging miR-29c-3p to promote MDM2 expression.
Thromb Res. 211:38–48. 2022. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Hu WN, Duan ZY, Wang Q and Zhou DH: The
suppression of ox-LDL-induced inflammatory response and apoptosis
of HUVECs by lncRNA XIAT knockdown via regulating miR-30c-5p/PTEN
axis. Eur Rev Med Pharmacol Sci. 23:7628–7638. 2019.PubMed/NCBI
|
|
18
|
Zhu J, Liu B, Wang Z, Wang D, Ni H, Zhang
L and Wang Y: Exosomes from nicotine-stimulated macrophages
accelerate atherosclerosis through miR-21-3p/PTEN-mediated VSMC
migration and proliferation. Theranostics. 9:6901–6919. 2019.
View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Wei L, Zhou Q, Tian H, Su Y, Fu GH and Sun
T: Integrin b3 promotes cardiomyocyte proliferation and attenuates
hypoxia-induced apoptosis via regulating the PTEN/Akt/mTOR and
ERK1/2 pathways. Int J Biol Sci. 16:644–654. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Tahtasakal R, Sener EF, Delibasi N,
Hamurcu Z, Mehmetbeyoglu E, Bayram KK, Gunes I, Goksuluk D and
Emirogullari ON: Overexpression of the PTEN gene in myocardial
tissues of coronary bypass surgery patients. Arq Bras Cardiol.
120:e202201692023.(In English, Portuguese). View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Chetram MA and Hinton CV: PTEN regulation
of ERK1/2 signaling in cancer. J Recept Signal Transduct Res.
32:190–195. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Wang J, Feng Q, Liang D and Shi J:
MiRNA-26a inhibits myocardial infarction-induced apoptosis by
targeting PTEN via JAK/STAT pathways. Cells Dev. 165:2036612021.
View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Roger I, Milara J, Montero P and Cortijo
J: The role of JAK/STAT molecular pathway in vascular remodeling
associated with pulmonary hypertension. Int J Mol Sci. 22:49802021.
View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Yu Y, Shen Y, Li J, Liu J, Liu S and Song
H: Viral infection related venous thromboembolism: Potential
mechanism and therapeutic targets. Ann Palliat Med. 9:1257–1263.
2020. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Pang Q, You L, Meng X, Li Y, Deng T, Li D
and Zhu B: Regulation of the JAK/STAT signaling pathway: The
promising targets for cardiovascular disease. Biochem Pharmacol.
213:1155872023. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Baldini C, Moriconi FR, Galimberti S,
Libby P and De Caterina R: The JAK-STAT pathway: An emerging target
for cardiovascular disease in rheumatoid arthritis and
myeloproliferative neoplasms. Eur Heart J. 42:4389–4400. 2021.
View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Fu X, Sun Z, Long Q, Tan W, Ding H, Liu X,
Wu L, Wang Y and Zhang W: Glycosides from Buyang Huanwu Decoction
inhibit atherosclerotic inflammation via JAK/STAT signaling
pathway. Phytomedicine. 105:1543852022. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Xu M, Li X and Song L: Baicalin regulates
macrophages polarization and alleviates myocardial
ischaemia/reperfusion injury via inhibiting JAK/STAT pathway. Pharm
Biol. 58:655–663. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Xue W and Deng L: EP300 improves
endothelial injury and mitochondrial dysfunction in coronary artery
disease by regulating histone acetylation of SOCS1 promoter via
inhibiting JAK/STAT pathway. Cytokine. 176:1565072024. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Ma Y, Tan F and Yu S: Diosmin inhibits
apoptosis of vascular endothelial cells in rats with traumatic deep
vein thrombosis through JAK-STAT signaling pathway. Panminerva Med.
24:10.23736/S0031–0808.19.03718-2. 2019.
|
|
31
|
Ren G, Yang EJ, Tao S, Mou PK, Pu Y, Chen
LJ and Shim JS: MDM2 inhibition is synthetic lethal with PTEN loss
in colorectal cancer cells via the p53-dependent mechanism. Int J
Biol Sci. 19:3544–3557. 2023. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Livak KJ and Schmittgen TD: Analysis of
relative gene expression data using real-time quantitative PCR and
the 2(−Delta Delta C(T)) method. Methods. 25:402–408. 2001.
View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Szklarczyk D, Gable AL, Nastou KC, Lyon D,
Kirsch R, Pyysalo S, Doncheva NT, Legeay M, Fang T, Bork P, et al:
The STRING database in 2021: Customizable protein-protein networks,
and functional characterization of user-uploaded gene/measurement
sets. Nucleic Acids Res. 49((D1)): D605–D612. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Chen L, Zhang YH, Wang S, Zhang Y, Huang T
and Cai YD: Prediction and analysis of essential genes using the
enrichments of gene ontology and KEGG pathways. PLoS One.
12:e01841292017. View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Sun LL, Xiao L, Du XL, Hong L, Li CL, Jiao
J, Li WD and Li XQ: MiR-205 promotes endothelial progenitor cell
angiogenesis and deep vein thrombosis recanalization and resolution
by targeting PTEN to regulate Akt/autophagy pathway and MMP2
expression. J Cell Mol Med. 23:8493–8504. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
36
|
Zhang Y, Liu J, Jia W, Tian X, Jiang P,
Cheng Z and Li J: AGEs/RAGE blockade downregulates Endothenin-1
(ET-1), mitigating Human Umbilical Vein Endothelial Cells (HUVEC)
injury in deep vein thrombosis (DVT). Bioengineered. 12:1360–1368.
2021. View Article : Google Scholar : PubMed/NCBI
|
|
37
|
Athanasios A, Charalampos V, Vasileios T
and Ashraf GM: Protein-Protein interaction (PPI) network: Recent
advances in drug discovery. Curr Drug Metab. 18:5–10. 2017.
View Article : Google Scholar : PubMed/NCBI
|
|
38
|
Chang CJ, Freeman DJ and Wu H: PTEN
regulates Mdm2 expression through the P1 promoter. J Biol Chem.
279:29841–29848. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
39
|
Wang T, Guan R, Xia F, Du J and Xu L:
Curcumin promotes venous thrombi resolve process in a mouse deep
venous thrombosis model via regulating miR-499. Microvasc Res.
136:1041482021. View Article : Google Scholar : PubMed/NCBI
|
|
40
|
Maeshima T, Aisu S, Ohkura N, Watanabe M
and Itagaki F: The association between deep vein thrombosis,
pulmonary embolism, and janus kinase inhibitors: Reporting status
and signal detection in the Japanese adverse drug event report
database. Drugs Real World Outcomes. 11:369–375. 2024. View Article : Google Scholar : PubMed/NCBI
|
|
41
|
Orozco-García E, van Meurs DJ, Calderón
JC, Narvaez-Sanchez R and Harmsen MC: Endothelial plasticity across
PTEN and Hippo pathways: A complex hormetic rheostat modulated by
extracellular vesicles. Transl Oncol. 31:1016332023. View Article : Google Scholar : PubMed/NCBI
|
|
42
|
Chu C, Wang B, Zhang Z, Liu W, Sun S,
Liang G, Zhang X, An H, Wei R, Zhu X, et al: miR-513c-5p
suppression aggravates pyroptosis of endothelial cell in deep
venous thrombosis by promoting caspase-1. Front Cell Dev Biol.
10:8387852022. View Article : Google Scholar : PubMed/NCBI
|
|
43
|
Obermayer G, Afonyushkin T and Binder CJ:
Oxidized low-density lipoprotein in inflammation-driven thrombosis.
J Thromb Haemost. 16:418–428. 2018. View Article : Google Scholar : PubMed/NCBI
|