Introduction
Epithelioid hemangioendothelioma (EHE) is a rare
tumor of vascular origin (with an incidence of less than one in
1,000,000 worldwide) with low to moderate grade malignant
properties. EHE was initially described in 1982 by Weiss and
Enzinger (1). Hepatic EHE (HEHE)
mainly affects middle-aged females with a variable and
unpredictable clinical course. The survival time ranges between 5
and 28 years to a rapidly progressing disease with a fatal outcome
(2,3). Thus far, no definitive factors for the
development of HEHE have been identified; although, oral
contraceptive pills, exposure to vinyl chloride, liver trauma and
viral hepatitis may be implicated. In addition, the prognostic
factors have not been clearly defined (4).
Relatively fewer cases of HEHE (mainly in Western
countries) have been reported worldwide (4,5).
However, HEHE in China has been reported in small case series.
Therefore, whether HEHE in the Chinese population exhibits
different characteristics than that of Western patients has not
been well summarized or compared, and this may be due to the rarity
of the disease and the small number of previously reported
cases.
The present study compared 50 Chinese patients with
HEHE to 402 Western patients with HEHE [summarized by Mehrabi et
al (5)], in order to describe
the characteristics and identify the prognostic factors of HEHE in
Chinese patients.
Materials and methods
The data of six patients with HEHE that received
consultation at the Beijing Friendship Hospital between 2000 and
2012 were collected. The patients’ medical records were
retrospectively reviewed with regard to clinical manifestations,
laboratory observations, imaging with pathological features,
treatment and clinical outcome. Pathological diagnosis of HEHE was
reconfirmed by a pathologist from the China-Japan Friendship
Hospital (Beijing, China) on the basis of the presence of CD34- or
CD31-positive epithelioid or dendritic endothelial cells
infiltrating the hepatic sinusoids. The study protocol was approved
by the Research Ethics Committee of the Beijing Friendship
Hospital, Capital Medical University (Beijing, China).
Furthermore, literature searches were conducted via
PubMed, Medline and the China National Knowledge Infrastructure
(CNKI) using the terms ‘hepatic epithelioid hemangioendothelioma’
or ‘epithelioid hemangioendothelioma of the liver’ between the
years of 1989 and mid-2012. Chinese patients with HEHE whose cases
were published in English or at least provided an abstract in
English, were included. The six patients diagnosed at the Beijing
Friendship Hospital were evaluated with the 44 published Chinese
cases (a total of 50 cases) and compared with 402 Western patients
with HEHE. The patient data were obtained from an extensive review
by Mehrabi et al (5),
based on the published literature between 1984 and 2005. Patient
information, such as age, gender, clinical manifestation,
diagnostic tools, histopathological aspects, treatments and
outcomes, were documented in the review by Mehrabi et al.
Therefore, this information from the Western HEHE patients could be
compared with that of the Chinese patients.
Among the Chinese patients with HEHE, the final
outcome was available in 25 patients (the remaining patients
succumbed during follow-up), those who remained alive (n=16) were
compared with those who had succumbed to the disease (n=9). This
was in order to identify risk factors of poor prognosis, and the
χ2 test and Cox regression analysis were used.
Statistical analyses
Frequency distribution and differences between the
50 Chinese and 402 Western cases, including the 25 Chinese patients
who survived or who had succumbed to the disease, were determined
by the χ2 test for qualitative results and Student’s
t-test for quantitative results. Log-rank survival analysis was
performed using Kaplan-Meier methods to test differences in
survival (in months) between Chinese patients who underwent surgery
[liver transplantation (LTx) and liver resection (LRx)],
trans-catheter arterial chemoembolization (TACE) and palliative
treatment. P<0.05 was considered to indicate a statistically
significant difference. A backward stepwise Cox regression model
was used to identify risk factors for poor prognosis. The following
criteria were used for inclusion and exclusion: Inclusion,
P<0.05; and exclusion, P>0.10.
Results
Summary of the six Chinese patients
diagnosed with HEHE and the follow-up
Over the past 11 years, six patients with
pathologically confirmed HEHE were identified. The demographic and
clinical characteristics, including treatment and outcome of these
patients, are summarized in Table
I. The biochemical parameters of the six patients included
mildly elevated alkaline phosphatase (ALP), γ glutamyl
transpeptidase (GGT; 3/6), alanine transaminase (ALT) and aspartate
transaminase (AST; 1/6) levels. The viral markers for hepatitis B
virus (HBV) and hepatitis C virus were all negative. Calcification
was found in four patients and capsular retraction in three
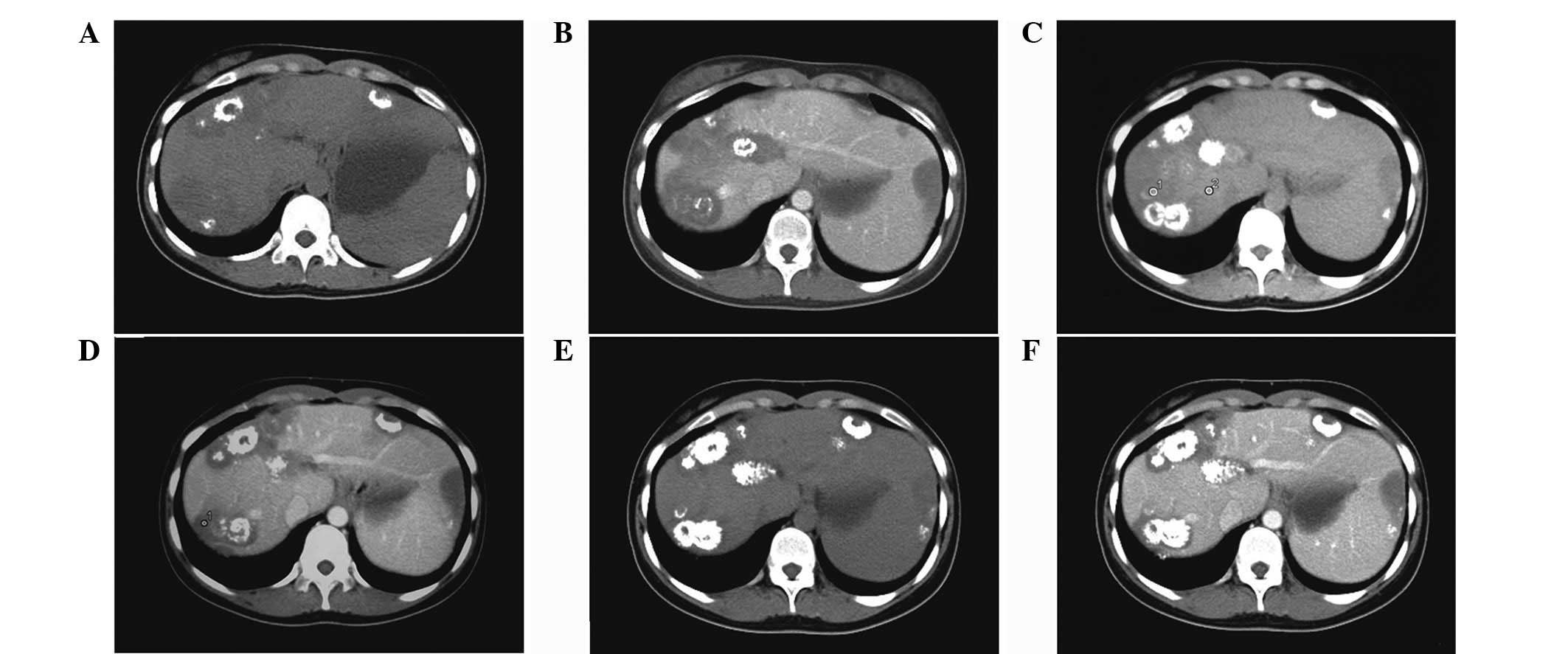
patients (Fig. 1). A total of two
out of the six patients exhibited positive ‘target’ and ‘halo’
signs.
 | Table IGeneral condition, clinical
manifestation, diagnosis, treatment and outcome of six patients
with HEHE. |
Table I
General condition, clinical
manifestation, diagnosis, treatment and outcome of six patients
with HEHE.
| Patient | Gender/age,
years | Presenting
symptoms | Physical examination
observations | Tumor number and
location | Maximum size, cm | Treatment | Outcome (months) |
|---|
| 1 | F/49 | RUQ pain | Pain induced by
percussion on liver region | Multiple, the two
lobes | 4.1×2.7 | None | Loss of
follow-up |
| 2 | F/35 | RUQ pain | Pain induced by
percussion on liver region | Multiple, the two
lobes | 4.0×3.5 | TCM | Survived (16) |
| 3 | F/56 | RUQ discomfort and
fatigue | Dark facial
appearance and palmar erythema | Multiple, the two
lobes | 7.0×4.9 | None | Succumbed to disease
(10) |
| 4 | F/22 | None | None | Multiple, the two
lobes | 3.6×3.1 | None | Survived (17) |
| 5 | M/45 | Abdominal distention
weight loss | Hepatomegaly,
shifting dullness and mild edema | Multiple, the two
lobes | 5.0×4.5 | TCM | Succumbed to disease
(79) |
| 6 | M/61 | None | Hepatomegaly | Diffuse, the two
lobes | 3.0×2.3 | None | Survived (36) |
Diagnosis of HEHE was established in all six Chinese
patients by core liver biopsy, according to the presence of
CD34/CD31-bearing epithelioid or dendritic endothelial cells
(Fig. 2). All six patients received
supportive therapy and one patient (no. 6) was on the waiting list
for LTx. A total of three out of the six patients survived, with
the survival period ranging between 16 and 36 months. One patient
(no. 4; without treatment) exhibited an evident increase in the
quantity of calcification, but the tumor remained stable even
showing self-regression over three years (Fig. 1). In addition, two patients
succumbed to liver failure due to the progression of the tumor and
the remaining patient did not return for follow-up. No identifiable
underlying risk factors were identified.
 | Figure 2Histopathology of hepatic epithelioid
hemangioendothelioma. (A) Percutaneous liver biopsy of one of the
tumor nodules showed liver parenchyma replacement by tumor cells
with mucoid stroma and sparing of portal tract, as indicated by the
arrow. Periodic acid Schiff staining (magnification, ×10). (B)
Scanty tumor cells, in red and indicated by the arrow, embedded in
mucopolysaccharide-rich stroma and excessive extracellular matrix
following Masson staining. Masson’s Trichrome stain (magnification,
×40). (C) Adjacent to the center of the tumor, increased
epithelioid (intracytoplasmic lumina containing erythrocytes, as
indicated by the arrow) or dendritic tumor cells with stroma were
observed. Hematoxylin and eosin staining (magnification, ×40).
Positive CD34 epithelioid cells (D) scattered in the tumor stroma
(CD34 staining; magnification, ×80) and (E) infiltrating the
sinusoids, creating the potential for tumor spread (CD31 staining;
magnification, ×40). |
Summary and analyses of 50 Chinese
patients with HEHE, and their comparison with 402 HEHE patients
from Western populations
A total of 11 studies were retrieved from PubMed,
but two were excluded (mainly for not focusing on HEHE). Therefore,
nine studies (38 patients), including patients with primary HEHE
from mainland China (6–10), Hong Kong (11) and Taiwan (12–14),
were subsequently included in the study. In addition, a Chinese
case report that included eight patients was identified on the CNKI
database and was also included (15). Of these eight patients, two were
diagnosed with HEHE co-existing with hepatocellular carcinoma (HCC)
and, consequently, were excluded from the study. Thus, a total of
44 (previously published) Chinese patients with HEHE and six
Chinese patients diagnosed with HEHE at the Beijing Friendship
Hospital were analyzed as a whole in the current study. Specimens
obtained for pathology were confirmed through liver biopsy (62%),
wedge LRx (34%) and LTx (4%).
Demographic and clinical
manifestation
The male to female ratio of the 50 Chinese patients
was 1:2.1 and the mean age was 44.2 years (ranging between 22 and
86 years; Table II). The
presenting symptoms of HEHE in the 50 Chinese patients were
non-specific and 40.0% of patients were asymptomatic, which is
significantly higher than in the 402 Western cases (40.0 vs. 24.8%;
P=0.026). Among these 50 patients, the serum tumor markers,
including CA-125 (4%), CEA (2%) and CA-199 (2%), were marginally
elevated with the exception of α-fetoprotein. The surface antigen
of the HBV, HBsAg, was positive in 12.2% of patients.
 | Table IIComparison between Chinese and Western
patients with HEHE. |
Table II
Comparison between Chinese and Western
patients with HEHE.
| Variables | Chinese patients
(n=50) | Western patients
(n=434) | P-value |
|---|
| Gender, M, %
(M:F) | 32 (16:34) | 42.4 (154:209) | 0.160 |
| Mean age, years
(range) | 44.2 (22–86) | 41.7 (3–86) | NA |
| Presenting symptoms,
% (n) |
| RUQ pain | 32.0 (16/50) | 48.6 (143/294) | 0.029 |
| Asymptomatic | 40.0 (20/50) | 24.8 (73/294) | 0.026 |
| Weight loss | 10.0 (5/50) | 15.6 (46/294) | 0.299 |
| Anorexia | 6.0 (3/50) | 8.2 (24/294) | 0.599 |
| Abdominal
discomfort | 26.0 (13/50) | 5.4 (16/294) | <0.001 |
| Positive physical
signs, % (n) |
| Hepatomegaly | 18.0 (9/50) | 20.4 (60/294) | 0.694 |
| Shifting
dullness | 8.0 (4/50) | 6.8 (20/294) | 0.759 |
| Jaundice | 6.0 (3/50) | 6.5 (19/294) | 0.902 |
| Splenomegaly | 8.0 (4/50) | 2.4 (7/294) | 0.037 |
| Abdominal
tenderness | 4.0 (2/50) | 1.0 (3/294) | 0.104 |
| Elevated ALP | 27.5 (11/40) | 68.6 (127/185) | <0.001 |
| Elevated GGT | 17.5 (7/40) | 45.4 (84/185) | 0.001 |
| Elevated ALT | 12.5 (5/40) | 28.6 (53/185) | 0.034 |
| Elevated AST | 17.5 (7/40) | 23.2 (43/185) | 0.428 |
| Elevated
Bilirubin | 7.5 (3/40) | 19.5 (36/185) | 0.07 |
| Imaging features, %
(n) |
| Low
consistency | 95.7 (44/46) | 98.1 (102/104) | 0.395 |
| Location of the
tumor, % (n) |
| Two lobes | 55.3 (21/38) | 84.6 (259/306) | <0.001 |
| Left lobe | 5.3 (2/38) | 2.0 (6/306) | 0.203 |
| Right lobe | 39.5 (15/38) | 13.4 (41/306) | <0.001 |
| Capsular
retraction | 59.5 (22/37) | 10.6 (15/142) | <0.001 |
| Halo sign | 37.5 (6/16) | 10.4 (5/48) | 0.005 |
| Calcification | 26.0 (13/50) | 12.7 (18/142) | 0.028 |
| Type of
involvement, % (n) |
| Multiple focal
including diffuse type | 86.0 (43/50) | 87.3 (267/306) | 0.806 |
| Unifocal | 14.0 (7/50) | 12.7 (39/306) | 0.806 |
| Extra hepatic
metastasis | 16.0 (8/50) | 36.6 (90/246) | 0.005 |
|
Immunohistopathological markers, %
(n) |
| CD34 | 93.5 (43/46) | 94.5 (129/137) | 0.799 |
| CD31 | 80.6 (25/31) | 86.1 (118/137) | 0.438 |
Pathological features, extrahepatic
metastasis, treatment and survival time
In terms of pathology, three different patterns of
HEHE were identified, solitary (14.0%), multiple (78.0%) and
diffuse (8.0%) types. The progression of multiple to diffuse type
was recorded in three patients. The characteristic feature of HEHE
was zonal distribution. In the midzone, scanty tumor cells were
distributed within mucopolysaccharide stroma or fibrotic tissue
(Fig. 2A and B). The tumor cells
(epithelioid or dendritic) were present at the periphery, invading
into sinusoids with atrophy or disappearance of the adjacent
hepatic plate was observed (Fig.
2C–E). In addition, tumor cells were observed to infiltrate the
branches of the portal vein and/or hepatic vein (26.9%). Positivity
of CD34 (93.5%) and CD31 (80.6%) were comparable between the 50
Chinese and 402 Western patients.
Metastasis outside of the liver was significantly
lower than in the Western population (16 vs. 36.6%; P=0.005);
although, the lung (3/8) was the most common site of metastasis,
followed by bone (2/8), spleen (1/8) and abdominal wall (1/8). One
patient exhibited multiple site metastasis, including the lung,
pericardium, spleen and bone.
The management for the 50 Chinese patients included
LRx (45.7%), LTx (5.7%) and TACE (14.3%). Patients without specific
treatment were 34.3% and final outcome was available for 25 Chinese
patients. Regardless of treatment, 16 patients survived with the
mean survival time of 31 months (maximal survival time was
approximately eight years). In total, nine patients succumbed to
the disease, with a mean survival time of 27 months. Although,
Kaplan-Meier analysis showed a trend of improvement in survival
time with liver surgery compared with TACE or palliative therapy.
No significant difference was identified in overall survival among
these treatment options (P=0.741). A total of two out of the seven
(28.6%) patients who survived following LRx exhibited recurrence of
the disease.
Identification of factors in Chinese
patients with HEHE as predictors for clinical outcomes
By χ2 analysis (Table III) the percentage of asymptomatic
patients was significantly higher in patients who had survived
(56.3%) compared with the group of patients who had succumbed to
their diseases (11.1%) (P=0.027). Although tumor markers were
non-specific for HEHE, a higher proportion of abnormality of tumor
markers (33.3%) was identified in the patients who had succumbed to
their diseases compared with the patients who had survived (6.2%)
(P=0.076). No significant difference was identified in extrahepatic
metastasis between the two groups.
 | Table IIIComparison between Chinese patients
who survived and succumbed to the disease in terms of demographic,
clinical, laboratory and radiological parameters. |
Table III
Comparison between Chinese patients
who survived and succumbed to the disease in terms of demographic,
clinical, laboratory and radiological parameters.
| Parameters | Survived
(n=16) | Succumbed
(n=9) | P-value |
|---|
| Gender, F, %
(F:M) | 81.2 (13:3) | 66.7 (6:3) | 0.412 |
| Age, years (mean ±
SD) | 43.1±12.7 | 46.8±19.5 | 0.568 |
| Asymptomatic, %
(n) | 56.3 (9/16) | 11.1 (1/9) | 0.027 |
| Tumor markers
(CA199 and CEA), % (n) | 6.2 (1/16) | 33.3 (3/9) | 0.076 |
| Abnormality of
LFTs, % (n) | 31.2 (5/16) | 55.6 (5/9) | 0.234 |
| HBsAg, % (n) | 12.5 (2/16) | 33.3 (3/9) | 0.211 |
| Tumor size, cm
(mean ± SD) | 4.4±1.6 | 5.2±2.2 | 0.342 |
| Target sign, %
(n) | 36.4 (4/11) | 33.3 (2/6) | 0.901 |
| Capsular
retraction, % (n) | 54.5 (6/11) | 66.7 (4/6) | 0.627 |
| Calcification, %
(n) | 18.8 (3/16) | 33.3 (3/6) | 0.412 |
| Multiple and
diffuse type: solitary type, % (ratio) | 87.5 (7:1) | 88.9 (8:1) | 0.918 |
| Extrahepatic
metastasis, % (n) | 18.8 (3/16) | 22.2 (2/9) | 0.835 |
| Life period, months
(mean ± SD) | 31±29.3 | 27±26.6 | 0.726 |
By a backward stepwise COX regression model, the
relative risk (RR) in patients with diffuse type of the disease was
12.17 [95% confidence interval (CI), 1.595–92.979; P=0.016] and
tumor size was 1.58 (95% CI, 1.032–2.422; P=0.035). Again, presence
of extrahepatic metastasis was not an independent risk factor for
poor prognosis (RR, 0.025; 95% CI, 0–13; P=0.247).
Discussion
HEHE is a rare malignant tumor of vascular origin
and an intermediate between hemangioma and angiosarcoma in nature.
EHE was first reported in liver tissue by Ishak et al in
1984 (16). Its vascular origin is
supported by positive staining for factor VIII-related antigen. The
characteristics of HEHE in the Chinese population are not well
known. Therefore, the present study reported six patients diagnosed
in the Beijing Friendship Hospital and retrospectively reviewed 44
patients from the previously published literature, not only from
mainland China but also from Taiwan and Hong Kong. The current
study presents a large-scale summary of HEHE in China.
The present study found that HEHE mainly affects
Chinese adults during their mid-forties, with a higher prevalence
in females; the male to female ratio of the Chinese patients was
1:2.1, consistent with the 402 previously published cases. Notably,
40% of the 50 Chinese patients were diagnosed incidentally, which
is a significantly higher proportion than that in the previously
published studies. At present, increasing awareness of routine
checkup in the Chinese population contributes to the early
detection of this rare disease even at the asymptomatic stage.
Mildly elevated ALP and GGT are the most common types of abnormal
liver function tests (LFTs). However, LFTs revealed a significantly
lower incidence of abnormality than in the 402 Western cases (40
vs. 80%) which may be explained by early detection of HEHE. Of
note, LFTs may be within the normal range in the early stage of the
disease, however, with progression of the disease, HEHE may involve
more liver parenchyma and result in elevated liver enzymes in the
later stages of the disease.
Patients who initially exhibit a solitary lesion may
progress to exhibit multiple separate lesions, followed by multiple
coalescing lesions, which eventually progress to diffuse pattern.
The present study observed this progression in three patients.
During the natural development of this disease, the patient
exhibits an increased number of symptoms, signs and the involvement
of abnormal liver enzymes. The final clinical outcomes include
liver failure caused by loss of parenchyma or portal hypertension
(tumor cells invading and occluding presinusoidal and
postsinusoidal space). On the other hand, multiple lesions may
undergo self-remission manifested by progressive calcification,
even without specific therapy as shown in case no. 4 (Fig. 1).
Currently, LTx is an optimal treatment for
unresectable tumors, even in patients who exhibit extrahepatic
involvement with three- and five-year survival rates of ~80 and
70%, respectively (17–19). However, in China, few HEHE patients
have been previously treated with LTx. LRx remains the most common
choice for disease management where possible (20). Extrahepatic spread at the time of
LRx does not correlate with survival and has not been considered a
contraindication to surgery. Traditional chemotherapy does not
appear to be an acceptable treatment option for this disease due to
the insensitivity of the tumor cells to chemotherapeutic
intervention. However, it has been previously reported that
antiangiogenesis-based chemotherapy, such as thalidomide (21–23),
may effectively prevent the progression of the disease and improve
the clinical outcome.
Occasionally, it is difficult to select the most
appropriate treatment (LRx, LTx or chemotherapy), individually, due
to one or more of the following reasons. Firstly, unpredictable
clinical course ranging between complete remission and rupture of
tumor with a fatal outcome. Secondly, lack of first grade evidence
from well controlled-clinical trials due to the rarity of the
disease. Thirdly, certain insufficient treatments accelerate the
process of the disease leading to an unfavorable outcome, such as
insufficient LRx. Finally, unlike other tumors, such as HCC,
extrahepatic metastasis is not an absolute contraindication of
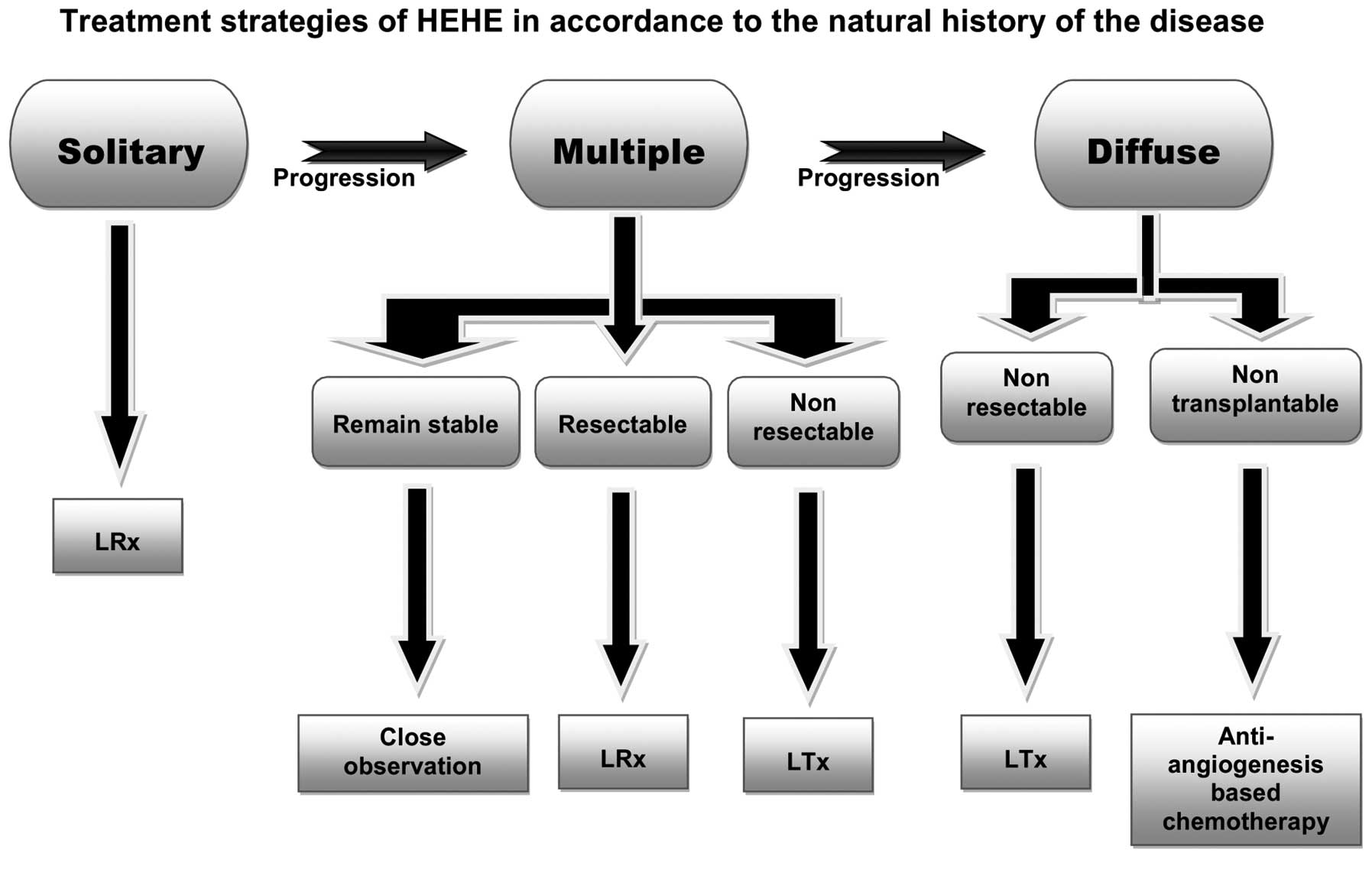
liver surgery. The current study proposes a treatment strategy
based on the course of HEHE, which complies with the principle of
monitoring closely and adapting properly, a strategy to fit each
individual’s demand to optimize the treatment regimen for the most
favorable outcome (Fig. 3).
Nevertheless, even without any treatment, 40% of
patient conditions remain stable for a long period of time.
Therefore, identifying risk factors which predict clinical course
is extremely important to determine treatment-related decisions for
the patients. In the current study, Chinese patients who had
survived were compared with patients who had succumbed to their
diseases. The results showed that patients who exhibited systemic
symptoms, such as larger tumor size and diffuse type, carried an
unfavorable outcome, similar to that in two previous studies by
Grozt et al (24) and Wang
et al (25).
Notably, unlike Western cases, a number of HEHE
patients in China are asymptomatic with normal liver enzymes and
exhibit less extrahepatic metastasis for a considerable part of the
disease course. Furthermore, LRx rather than LTx is a more common
treatment option in China. Finally, treatment of HEHE must be in
accordance with the natural history of the disease and patients
with individualized treatment may exhibit an improved clinical
outcome.
Acknowledgements
The authors would like to thank Professor Ri-sheng
Yu and Dr Ying Chen from the Department of Radiology, Second
Affiliated Hospital, Zhejiang University School of Medicine,
Professor Xiang-hong Li and Dr Ai-lian Zhao from the Department of
Pathology, Peking University School of Oncology and Dr Min-shu
Hsieh from Department of Pathology, National Taiwan University
Hospital. They each provided invaluable information concerning
additional data for their patients that were not included in their
studies. In addition, the authors would like to thank Dr Yuan-yuan
Kong from the Department of Research, Beijing Friendship Hospital
for reviewing the statistical analyses and Professor Henry W.
Strobel from the University of Texas medical school (Houston, TX,
USA) for proofreading the current study. The study was supported by
the Beijing Nova program of China (grant no. 2009 B45).
Abbreviations:
|
HEHE
|
hepatic epithelioid
hemangioendothelioma
|
|
EHE
|
epithelioid hemangioendothelioma
|
|
LTx
|
liver transplantation
|
|
CNKI
|
China national knowledge
infrastructure
|
|
RR
|
relative risk
|
|
ALP
|
alkaline phosphatase
|
|
GGT
|
γ-glutamyl transferase
|
|
TCM
|
traditional Chinese medicine
|
|
HCC
|
hepatocellular carcinoma
|
|
RUQ
|
right upper quadrant
|
|
ALT
|
alanine transaminase
|
|
LFTs
|
liver function tests
|
|
LRx
|
liver resection
|
References
|
1
|
Weiss SW and Enzinger FM: Epithelioid
hemangioendothelioma: a vascular tumor often mistaken for a
carcinoma. Cancer. 50:970–981. 1982. View Article : Google Scholar
|
|
2
|
Komatsu Y, Koizumi T, Yasuo M, et al:
Malignant hepatic epithelioid hemangioendothelioma with rapid
progression and fatal outcome. Intern Med. 49:1149–1153. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Makhlouf HR, Ishak KG and Goodman ZD:
Epithelioid hemangioendothelioma of the liver: a clinicopathologic
study of 137 cases. Cancer. 85:562–582. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Thin LW, Wong DD, De Boer BW, et al:
Hepatic epithelioid haemangioendothelioma: challenges in diagnosis
and management. Intern Med J. 40:710–715. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Mehrabi A, Kashfi A, Fonouni H, Schemmer
P, Schmied BM and Hallscheidt P: Primary malignant hepatic
epithelioid hemangioendothelioma: a comprehensive review of the
literature with emphasis on the surgical therapy. Cancer.
107:2108–2121. 2006. View Article : Google Scholar
|
|
6
|
Zhao AL, Zhou LX and Li XH: Hepatic
epithelioid hemangioendothelioma in needle biopsy specimens: report
of 5 cases with review of literature. Zhonghua Bing Li Xue Za Zhi.
40:23–26. 2011.(In Chinese).
|
|
7
|
Chen Y, Yu RS, Qiu LL, Jiang DY, Tan YB
and Fu YB: Contrast-enhanced multiple-phase imaging features in
hepatic epithelioid hemangioendothelioma. World J Gastroenterol.
17:3544–3553. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Shi Y and Hou YY: Hepatic epithelioid
hemangioendothelioma: a case report. Zhonghua Bing Li Xue Za Zhi.
34:3832005.(In Chinese).
|
|
9
|
Lin J and Ji Y: CT and MRI diagnosis of
hepatic epithelioid hemangioendothelioma. Hepatobiliary Pancreat
Dis Int. 9:154–158. 2010.PubMed/NCBI
|
|
10
|
Ji ZF, Shen XZ, Zhang DY, Liu HY, Zhou Y,
Guo MY and Dong L: Hepatic epithelioid hemangioendothelioma: a
report of six patients. J Dig Dis. 11:254–258. 2010.PubMed/NCBI
|
|
11
|
Lau WY, Dewar GA and Li AK: Spontaneous
rupture of hepatic epithelioid haemangio-endothelioma. Aust N Z J
Surg. 59:972–9744. 1989. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Hsieh MS, Liang PC, Kao YC and Shun CT:
Hepatic epithelioid hemangioendothelioma in Taiwan: a
clinicopathologic study of six cases in a single institution over a
15-year period. J Formos Med Assoc. 109:219–227. 2010.
|
|
13
|
Lee HF, Lu CL and Chang FY: Electronic
clinical challenges and images in GI. Multiple hepatic tumors with
hemoperitoneum. Gastroenterology. 138:e3–e4. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Shen CH, Tsai MH, Chen TC, Liu NJ and
Sheen IS: Primary hepatic epithelioid hemangioendothelioma: case
report. Changgeng Yi Xue Za Zhi. 22:486–491. 1999.PubMed/NCBI
|
|
15
|
Zang SH, Cong WM and Wu MC: Epithelioid
hemangioendothelioma of the liver : a clinicopathological study on
8 cases and review of literature. Zhonghua Gan Dan Wai Ke Za Zhi.
6:327–330. 2003.
|
|
16
|
Ishak KG, Sesterhenn IA, Goodman ZD, Rabin
L and Stromeyer FW: Epithelioid hemangioendothelioma of the liver:
a clinicopathologic and follow-up study of 32 cases. Hum Pathol.
15:839–852. 1984. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Rodriguez JA, Becker NS, O’Mahony CA, Goss
JA and Aloia TA: Long-term outcomes following liver transplantation
for hepatic hemangioendothelioma: the UNOS experience from 1987 to
2005. J Gastrointest Surg. 12:110–116. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Lerut JP, Orlando G, Adam R, et al: The
place of liver transplantation in the treatment of hepatic
epitheloid hemangioendothelioma: report of the European liver
transplant registry. Ann Surg. 246:949–957; discussion 57. 2007.
View Article : Google Scholar
|
|
19
|
Madariaga JR, Marino IR, Karavias DD, et
al: Long-term results after liver transplantation for primary
hepatic epithelioid hemangioendothelioma. Ann Surg Oncol.
2:483–487. 1995. View Article : Google Scholar
|
|
20
|
Nudo CG, Yoshida EM, Bain VG, et al: Liver
transplantation for hepatic epithelioid hemangioendothelioma: the
Canadian multicentre experience. Can J Gastroenterol. 22:821–824.
2008.PubMed/NCBI
|
|
21
|
Salech F, Valderrama S, Nervi B, et al:
Thalidomide for the treatment of metastatic hepatic epithelioid
hemangioendothelioma: a case report with a long term follow-up. Ann
Hepatol. 10:99–102. 2011.
|
|
22
|
Raphael C, Hudson E, Williams L, Lester JF
and Savage PM: Successful treatment of metastatic hepatic
epithelioid hemangioendothelioma with thalidomide: a case report. J
Med Case Rep. 4:4132010. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Mascarenhas RC, Sanghvi AN, Friedlander L,
Geyer SJ, Beasley HS and Van Thiel DH: Thalidomide inhibits the
growth and progression of hepatic epithelioid hemangioendothelioma.
Oncology. 67:471–475. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Grotz TE, Nagorney D, Donohue J, et al:
Hepatic epithelioid haemangioendothelioma: is transplantation the
only treatment option? HPB (Oxford). 12:546–553. 2010. View Article : Google Scholar
|
|
25
|
Wang LR, Zhou JM, Zhao YM, et al: Clinical
experience with primary hepatic epithelioid hemangioendothelioma:
retrospective study of 33 patients. World J Surg. 36:2677–2683.
2012. View Article : Google Scholar
|