Introduction
Primary malignant pericardial mesothelioma (PMPM) is
an extremely rare tumor that develops in mesothelial cells of the
pericardium (1). Malignant
mesothelioma typically arises from the pleura (65–70%) and
peritoneum (30%) (2). Those tumors
arising from the pericardium account for only 1–2% of all
mesotheliomas (3). The incidence of
PMPM is extremely low, with <0.0022% of cases reported in a
large-scale autopsy study (1). PMPM
has been reported predominantly in men compared with women, with
2:1 and 3:1 ratios (2,4). The disease presents with non-specific
symptoms, including dyspnea or chest pain (4,5). Initial
manifestations, including pericardial effusion or pericardial
thickening, frequently result in confusion with pericarditis or
heart failure and delay diagnosis (4,6,7). Therefore, multi-modal imaging methods,
including echocardiography, computed tomography (CT), magnetic
resonance imaging (MRI) and
18F-fluorodeoxyglucose-positron emission tomography, are
often required for the diagnosis (8,9). Tumors
are located in a poorly resectable area and tend to infiltrate
adjacent structures such as the great vessels, therefore, complete
surgical removal is often not possible (5,10). As a
result, surgical resection combined with radiotherapy or
chemotherapy is required in cases of localized tumors (11,12). In
addition, numerous patients diagnosed with PMPM have accompanying
distant metastasis (13,14). For such cases, systemic chemotherapy
is important (11,14). However, there are currently no
existing standard chemotherapeutic drugs or treatment strategies,
and as a result overall prognosis remains poor at ~6 months
(2,4,5,11,13). The
present study reports the case of a patient diagnosed with PMPM
with accompanying lung metastasis. The patient demonstrated a
positive response to pemetrexed plus cisplatin followed by
pemetrexed monotherapy, leading to prolonged progression-free
survival for 21 months.
Case report
A 53-year-old woman presented to Korea University
Medical Center, Guro Hospital (Seoul, South Korea) with peripheral
edema, dyspnea on exertion, coughing and intermittent fever in May
2013. In February 2007, the patient had presented to the hospital
with massive pericardial effusion. An extensive investigation,
including pericardial biopsy, was performed to identify the cause.
However, there was no evidence linking the symptoms to viruses,
bacteria or malignancy. Chronic inflammation with fibrosis was
observed in a pericardial biopsy. Following pericardiocentesis and
treatment with diuretics, pericardial effusion resolved and did not
recur. The patient had maintained good health for 6 years until the
current presentation.
The patient was a non-smoker, occasionally drank
alcohol and had a history of working in a small factory making
electrical units. The patient had no other occupational or
environmental exposure to asbestos. Vital signs were stable upon
admission to Korea University Medical Center, Guro Hospital in
2013. The patient's jugular venous pressure was elevated and she
was positive for the Kussmaul's sign (15). No additional information, except for
mild cardiomegaly, was revealed by chest radiography. Transthoracic
echocardiography revealed a newly developed pericardial thickening
and mass-like lesion encircling the ascending aorta. However, the
ejection fraction was within the normal range. CT of the chest
revealed diffuse pericardial thickening and pericardial masses
surrounding the entire pericardium (Fig.
1A). Cardiac MRI revealed enhancement of the mass with internal
necrosis. Pericardiectomy for histological confirmation and biopsy
of the periaortic lymph node near the mass were performed. Upon
examination for distant metastasis, multiple tiny nodules, which
appeared to be metastatic, were observed in both lung fields on a
chest CT (Fig. 1B). No other distant
metastases were identified. Therefore, palliative chemotherapy was
initiated with pemetrexed (500 mg/m2) and cisplatin (75
mg/m2) via intravenous administration in a 3-week
schedule. Following the second cycle of treatment, the pericardial
thickening began to regress. The patient continued to receive
chemotherapy and the tumor size and number of lung metastases
reduced continuously (Fig. 1C and D).
From the tenth cycle, the dose of cisplatin was reduced to 50% of
the full dose (35 g/m2) due to grade 2 peripheral
neuropathy. Following the fourteenth cycle, only pemetrexed was
infused every 3 weeks. The tumor size reduced further and
maintained this reduced status (Fig. 1E
and F).
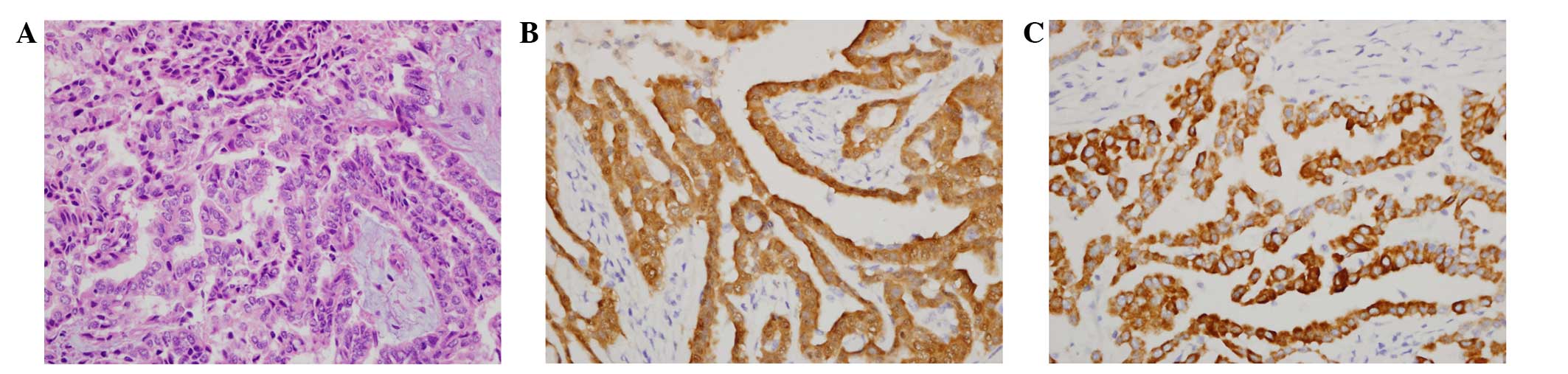
Using a light microscope, the excised pericardial
soft tissue confirmed the diagnosis of malignant pericardial
mesothelioma. Tumor tissue was fixed in 10%-formalin and embedded
in paraffin. Paraffin sections were routinely processed and stained
with hematoxylin and eosin. The specimens showed neoplastic cells
with epithelioid and papillary patterns (Fig. 2A). Immunohistochemistry was performed
using the BOND MAX system (Leica Biosystems, Newcastle, UK) with
the following antibodies: Monoclonal mouse anti-human calretinin
(dilution, 1:1,200; catalog no. NCL-L-CALRET-566; Leica
Biosystems), monoclonal mouse anti-human cytokeratin 5/6 (dilution,
1:1,200; catalog no. M7237; Dako, Glostrup, Denmark), monoclonal
mouse anti-human carcinoembryonic antigen (dilution, 1:200; catalog
no. M7072; Dako), monoclonal mouse anti-human thyroid transcription
factor-1 (TTF-1; dilution, 1:200; catalog no. M3675; Dako) and
monoclonal mouse anti-human Wilms' Tumor-1 (WT-1; dilution, 1:100;
catalog no. NCL-L-WT1-562; Leica Biosystems). Immunohistochemistry
revealed that the specimens were positive for calretinin and
cytokeratin 5/6 (Fig. 2B and C), but
negative for carcinoembryonic antigen, TTF-1 and WT-1 protein.
These findings were consistent with those from the excised
periaortic lymph node.
Following treatment, the patient developed
intermittent grade 3 neutropenia but recovered with no other
complications. The patient has been treated with pemetrexed with
regular CT scans every 3 months. The patient remains in good
medical condition 21 months after treatment initiation.
Informed consent was obtained from the patient for
publication of this study, and the study was approved by the Ethics
Committee of the Korea University Guro Hospital.
Discussion
PMPM is an extremely rare tumor accounting for 2–3%
of all cardiac and pericardial tumors (10). The association between asbestos
exposure and malignant pleural mesothelioma is well documented, but
the etiology of PMPM remains to be elucidated (16). Previous cases have rarely reported
obvious exposure to asbestos (4,17).
However, in the Lombardy Mesothelioma Registry, taken from a highly
industrialized region of northern Italy, 5/7 patients (71.4%) with
PMPM reported occupational asbestos exposure (18). In the present case, the patient had a
history of working in soldering in the 1990s. However, it is
difficult to connect this history with asbestos, as the patient's
work was not associated with construction, automobile repair or
asbestos textiles, which are the occupations most highly associated
with asbestos exposure.
Owing to its atypical and non-specific symptoms,
including dyspnea, coughing or chest pain, physicians are likely to
misdiagnose PMPM on initial examination of the patient. Numerous
patients with PMPM have presented with pericarditis with
pericardial effusion (6,19,20).
Furthermore, these patients suffered from recurrent pericardial
effusion and were diagnosed with PMPM following repetitive
investigation using additional imaging tools such as CT and MRI, as
well as tissue biopsy of the pericardium, to determine the cause of
the pericardial effusion. In the present case, the patient had a
history of massive pericardial effusion due to an unidentified
cause 6 years prior to the current study. Compared with other
cases, the time interval between the previous pericardial effusion
and the current presentation were too long for a diagnosis of
recurrent pericardial effusion in the present case, making it
difficult to connect with PMPM. However, PMPM should be considered
as a cause of unexplained recurrent pericardial effusion,
considering previous cases (6,7,21,22).
For the treatment of PMPM, surgical resection is the
treatment of choice for localized disease (12). However, numerous cases are locally
advanced, with invasion or infiltration of the myocardium, atria,
coronary arteries and the conduction system of the heart. In those
cases, complete surgical resection is not possible. In addition,
distant metastases in the lung or liver are observed in 25–45% of
cases (13,14). Patients with distant metastasis, such
as the present case, and patients who are not candidates for
surgery should be administered chemotherapy (11,14). Owing
to the rarity of PMPM, a standard chemotherapeutic regimen has not
yet been established and older chemotherapeutic drugs have
demonstrated little benefit in previous years (2). However, the introduction of pemetrexed,
a third-generation antifolate drug, demonstrated a survival benefit
when combined with cisplatin in patients with pleural mesothelioma
(23), leading to longer survival
times for patients with PMPM. In previous cases, several patients
who were treated with pemetrexed plus carboplatin or pemetrexed
plus cisplatin demonstrated positive responses after receiving only
two or three cycles of pemetrexed plus platinum (14,24,25).
Following 6–8 cycles of treatment, chemotherapy was stopped or
consolidation radiotherapy was added in these cases. Positive
responses continued for 6–26 months. Doval et al (14) described a patient who remained alive
26 months subsequent to the conclusion of 6 cycles of pemetrexed
plus cisplatin. However, other patients exhibited 6–10 months of
durable response, followed by an accelerated deterioration
subsequent to disease progression (24,25). In
patients in whom the response to chemotherapy is positive, it is
difficult to determine the appropriate duration of chemotherapy.
However, considering the aggressiveness and poor prognosis of PMPM,
continuation of pemetrexed monotherapy after several cycles of
pemetrexed plus cisplatin may be an appropriate treatment strategy
if the patient is able to tolerate the treatment. The number of
cycles of pemetrexed plus cisplatin treatment required for maximal
response and minimal toxicity remains to be elucidated. With
pemetrexed plus cisplatin treatment, physicians should be aware of
hematological and non-hematological toxicities, for example
peripheral neuropathy, as well as response (26). A treatment schedule of pemetrexed
maintenance chemotherapy following four cycles of pemetrexed plus
cisplatin is actively used for the treatment of lung cancer. The
application of a maximum of 44 cycles of pemetrexed for maintenance
chemotherapy was reported without significant toxicities in a phase
III study in lung cancer patients (27).
In conclusion, pemetrexed maintenance following
pemetrexed plus cisplatin combination therapy is an optimal choice
for the chemotherapy of inoperable or metastatic PMPM. Physicians
should consider the chemotherapy strategy applied within the
present study as a priority for the systemic treatment of PMPM,
which is typically associated with a poor prognosis. Further
investigation is required to determine the appropriate duration of
platinum combination therapy, and research on the efficacy of
combined therapy with other treatment strategies, such as
radiotherapy or surgery, is warranted.
References
|
1
|
De Rosa AF, Cecchin GV, Kujaruk MR, Gayet
EG, Grasso LE and Rigou DG: Malignant mesothelioma of the
pericardium. Medicina (B Aires). 54:49–52. 1994.(In Spanish).
PubMed/NCBI
|
|
2
|
Thomason R, Schlegel W, Lucca M, Cummings
S and Lee S: Primary malignant mesothelioma of the pericardium.
Case report and literature review. Tex Heart Inst J. 21:170–174.
1994.PubMed/NCBI
|
|
3
|
Falkenstern-Ge RF, Kimmich M, Bode-Erdmann
S, Friedel G, Ott G and Kohlhäufl M: Pleural mesothelioma
presenting as periumbilical metastasis: The first clinical
documentation. Case Rep Oncol Med. 2013:1987292013.PubMed/NCBI
|
|
4
|
Nilsson A and Rasmuson T: Primary
Pericardial mesothelioma: Report of a patient and literature
review. Case Rep Oncol. 2:125–132. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Eren NT and Akar AR: Primary pericardial
mesothelioma. Curr Treat Options Oncol. 3:369–373. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Makarawate P, Chaosuwannakit N,
Chindaprasirt J, Ungarreevittaya P, Chaiwiriyakul S, Wirasorn K,
Kuptarnond C and Sawanyawisuth K: Malignant mesothelioma of the
pericardium: A report of two different presentations. Case Rep
Oncol Med. 2013:3569012013.PubMed/NCBI
|
|
7
|
Choi WS, Im MS, Kang JH, Kim YG, Hwang IC,
Lee JM, Lee S, Shin HS, Lee SP and Cho GY: Primary malignant
pericardial mesothelioma presenting as acute pericarditis. J
Cardiovasc Ultrasound. 20:57–59. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Nana A, Vorilhon C, Adjtoutah D, Azarnoush
K, Kissel V, Chabin X, Chailloux A, Belhakem A, Tixier V, Ferrier
N, et al: Contribution of magnetic resonance imaging in diagnosis
of pericardial mesothelioma: A case report. Ann Cardiol Angeiol
(Paris). 61:370–374. 2012.(In French). View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Ost P, Rottey S, Smeets P, Boterberg T,
Stragier B and Goethals I: F-18 fluorodeoxyglucose PET/CT scanning
in the diagnostic work-up of a primary pericardial mesothelioma: A
case report. J Thorac Imaging. 23:35–38. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Kaul TK, Fields BL and Kahn DR: Primary
malignant pericardial mesothelioma: A case report and review. J
Cardiovasc Surg (Torino). 35:261–267. 1994.PubMed/NCBI
|
|
11
|
Maruyama R, Sakai M, Nakamura T, Suemitsu
R, Okamoto T, Wataya H, Nishiyama K, Kamei T and Ichinose Y:
Triplet chemotherapy for malignant pericardial mesothelioma: A case
report. Jpn J Clin Oncol. 36:245–248. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Fujita K, Hata M, Sezai A and Minami K:
Three-year survival after surgery for primary malignant pericardial
mesothelioma: Report of a case. Surg Today. 44:948–951. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Papi M, Genestreti G, Tassinari D,
Lorenzini P, Serra S, Ricci M, Pasquini E, Nicolini M, Pasini G,
Tamburini E, et al: Malignant pericardial mesothelioma. Report of
two cases, review of the literature and differential diagnosis.
Tumori. 91:276–279. 2005.PubMed/NCBI
|
|
14
|
Doval DC, Pande SB, Sharma JB, Rao SA,
Prakash N and Vaid AK: Report of a case of pericardial mesothelioma
with liver metastases responding well to pemetrexed and
platinum-based chemotherapy. J Thorac Oncol. 2:780–781. 2007.
View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Bilchick KC and Wise RA: Paradoxical
physical findings described by Kussmaul: Pulsus paradoxus and
Kussmaul's sign. Lancet. 359:1940–1942. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Attanoos RL: Asbestos-related lung
disease. Surg Pathol Clin. 3:109–127. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Fujiwara H, Kamimori T, Morinaga K, Takeda
Y, Kohyama N, Miki Y, Inai K and Yamamoto S: An autopsy case of
primary pericardial mesothelioma in arc cutter exposed to asbestos
through talc pencils. Ind Health. 43:346–350. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Mensi C, Giacomini S, Sieno C, Consonni D
and Riboldi L: Pericardial mesothelioma and asbestos exposure. Int
J Hyg Environ Health. 214:276–279. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Kayatta MO, Dineen SP, Sica G, Puskas JD
and Pickens A: Primary pericardial mesothelioma in a 19-year-old
presenting as pericarditis. Ann Thorac Surg. 96:680–681. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Gong W, Ye X, Shi K and Zhao Q: Primary
malignant pericardial mesothelioma - a rare cause of superior vena
cava thrombosis and constrictive pericarditis. J Thorac Dis.
6:E272–E275. 2014.PubMed/NCBI
|
|
21
|
Molina Garrido MJ, Mora Rufete A,
Rodriguez-Lescure A, Cascon Perez JD, Ardoy F, Guillen Ponce C and
Carrato Mena A: Recurrent pericardial effusion as initial
manifestation of primary diffuse pericardial malignant
mesothelioma. Clin Transl Oncol. 8:694–696. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Butz T, Faber L, Langer C, Korfer J,
Lindner O, Tannapfel A, Muller KM, Meissner A, Plehn G, Trappe HJ,
et al: Primary malignant pericardial mesothelioma - a rare cause of
pericardial effusion and consecutive constrictive pericarditis: A
case report. J Med Case Rep. 3:92562009. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Vogelzang NJ, Rusthoven JJ, Symanowski J,
Denham C, Kaukel E, Ruffie P, Gatzemeier U, Boyer M, Emri S,
Manegold C, et al: Phase III study of pemetrexed in combination
with cisplatin versus cisplatin alone in patients with malignant
pleural mesothelioma. J Clin Oncol. 21:2636–2644. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Santos C, Montesinos J, Castañer E, Sole
JM and Baga R: Primary pericardial mesothelioma. Lung Cancer.
60:291–293. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Fujimoto N, Gemba K, Wada S, Ono K, Fujii
Y, Ozaki S, Ikeda T, Taguchi K, Kunitomo T and Kishimoto T:
Malignant pericardial mesothelioma with response to chemotherapy. J
Thorac Oncol. 4:1440–1441. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Niyikiza C, Hanauske AR, Rusthoven JJ,
Calvert AH, Allen R, Paoletti P and Bunn PA: Pemetrexed safety and
dosing strategy. Semin Oncol. 29(Suppl 18): 24–29. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Paz-Ares LG, de Marinis F, De diu M,
Thomas M, Pujol JL, Bidoli P, Molinier O, Sahoo TP, Laack E, Reck
M, et al: PARAMOUNT: Final overall survival results of the phase
III study of maintenance pemetrexed versus placebo immediately
after induction treatment with pemetrexed plus cisplatin for
advanced nonsquamous non-small-cell lung cancer. J Clin Oncol.
31:2895–2902. 2013. View Article : Google Scholar : PubMed/NCBI
|