Introduction
Reninomas, or renal juxtaglomerular cell tumors,
develop within the juxtaglomerular apparatus through the evolution
of small artery smooth muscle cells. These tumor cells produce
excessive amounts of renin that results in severe hypertension with
hypokalemia and hyperaldosteronism, through the activity of the
renin-angiotensin aldosterone system (1). It is a rare form of secondary
hypertension. Removing the reninoma results in the conversion of
increased blood pressure to normal blood pressure (2). Therefore, perioperative hemodynamic
management is important in patients who undergo surgery for the
removal of a reninoma.
Adrenal adenoma is a benign neoplasm, which is
derived from cells of the adrenal cortex, and may be functionally
active or nonfunctional (3).
Functional adrenal adenoma is able to cause aldosteronism or
Cushing's syndrome. Primary aldosteronism (PA) is characterized by
autonomous aldosterone production, which is a cause of secondary
hypertension (4). Evidence has
developed over the past decades and led to the recognition that
autonomous adrenal aldosterone production, termed primary
aldosteronism, is common in hypertensive patients. Between 5 and
13% of patients with hypertension have primary aldosteronism
(5).
The present study reported a rare case of reninoma
coexisting with an adrenal adenoma in a young female with secondary
hypertension during pregnancy.
Case report
A 2.5-cm mass was detected on the right adrenal
gland of a 31-year-old pregnant female with hypertension in her
33rd gestational week by an ultrasound scan. The patient presented
with a personal history of elevated blood pressure (BP) for several
months prior to conception, and exhibited a family history of
hypertension. There were no other abnormalities found by the
ultrasounds of the adrenal gland and the renal artery, therefore
the patient was diagnosed with primary hypertension. The BP levels
of the patient were uncontrolled during pregnancy. In the 35th+6
gestational week, the patient underwent surgical termination of the
pregnancy due to uncontrolled hypertension, with delivery of a
viable fetus. The BP of the patient fluctuated between 140 and
177/90 and 115 mmHg subsequent to the termination of the pregnancy.
An abdominal magnetic resonance imaging (MRI) scan and an
ultrasound were performed 1 month subsequent to the termination of
the pregnancy.
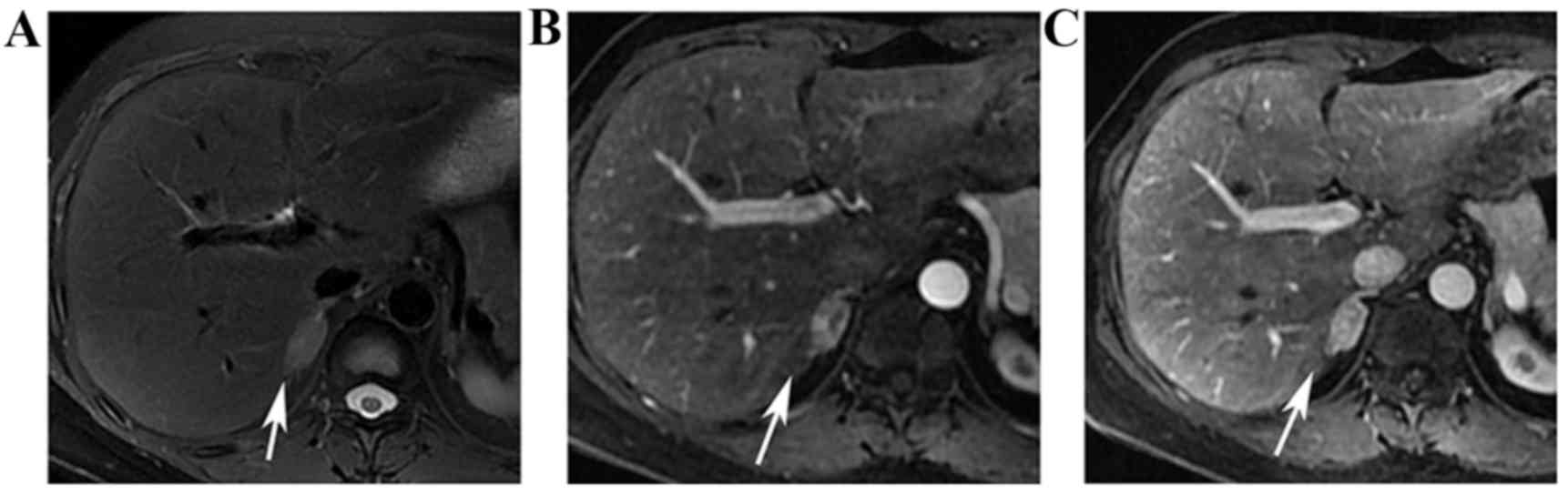
The MRI was performed and showed an oval-shaped mass
on the right adrenal gland, as exhibited in Fig. 1. The mass was recorded as a
hyperintensity region on the T2 weighted-image (T2WI), and showed a
marked heterogeneous enhancement during the arterial phase and a
homogeneous enhancement during the venous phase, which was
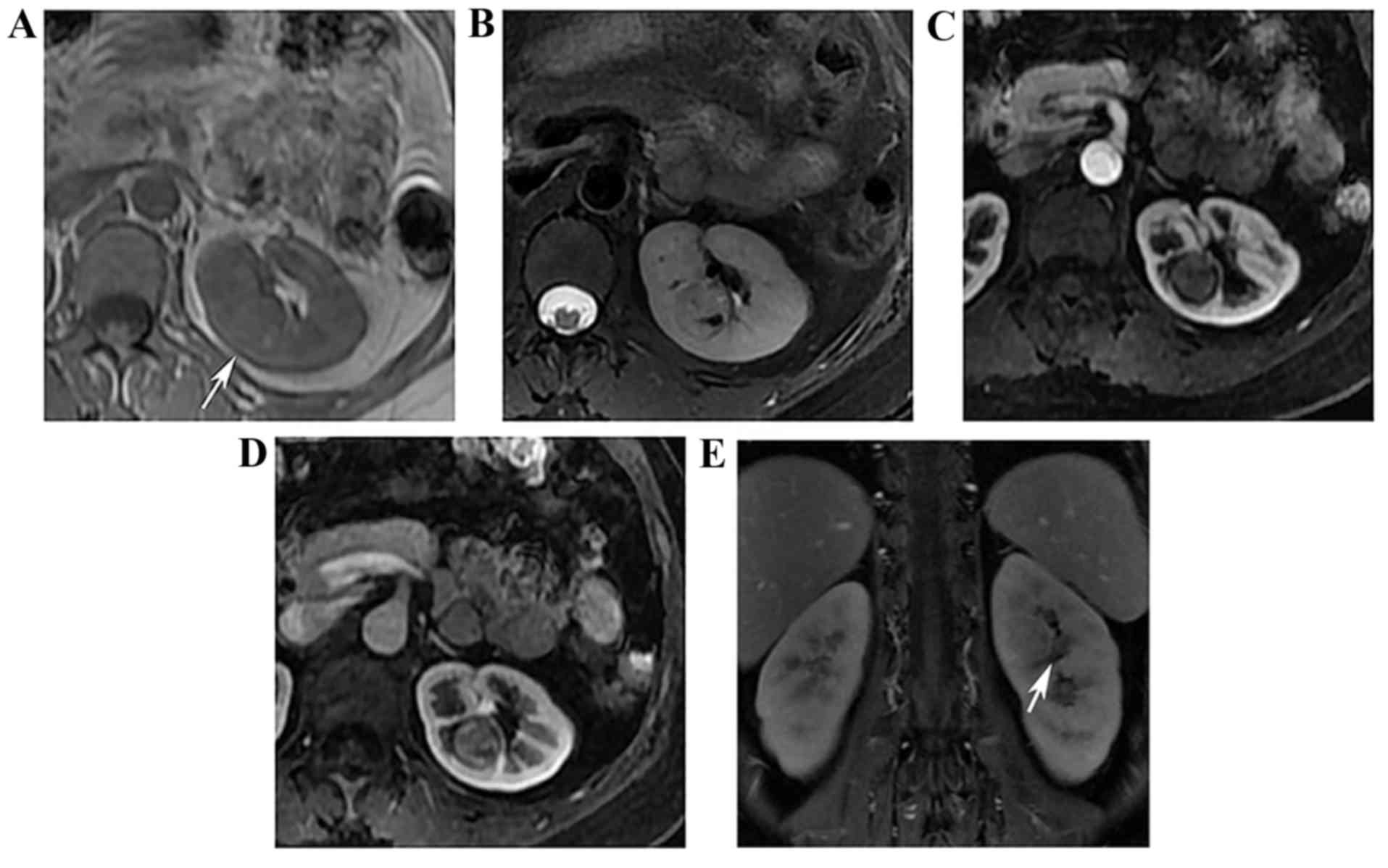
considered typical of an adrenal adenoma. In addition, a small
well-defined solid mass was found on the left kidney, which is
demonstrated in Fig. 2. The lesion
was recorded as isointense on the T1 weighted-image (T1WI) with a
spot hyperintensity area, and was hyperintense on T2WI. The mass
was not markedly enhanced during the arterial phase, and was
slightly enhanced during the venous phase. The mass was observed to
be isointense during the delay phase.
An ultrasound scan detected a clear hypoechoic mass
on the right adrenal gland. However, a diagnosis of the lesion on
the left kidney was not reached. The clinical diagnosis was
functional adrenocortical adenoma, primary aldosteronism (PA), and
a potentially malignant left renal tumor. The surgical team removed
the right adrenal neoplasm first, and removed the left renal tumor
subsequent to two months. The patient underwent a laparoscopic
right adrenalectomy to remove the right adrenal neoplasm.
Pathological analysis revealed that the neoplasm was an
adrenocortical adenoma. However, the BP levels of the patient did
not return to normal subsequent to the operation.
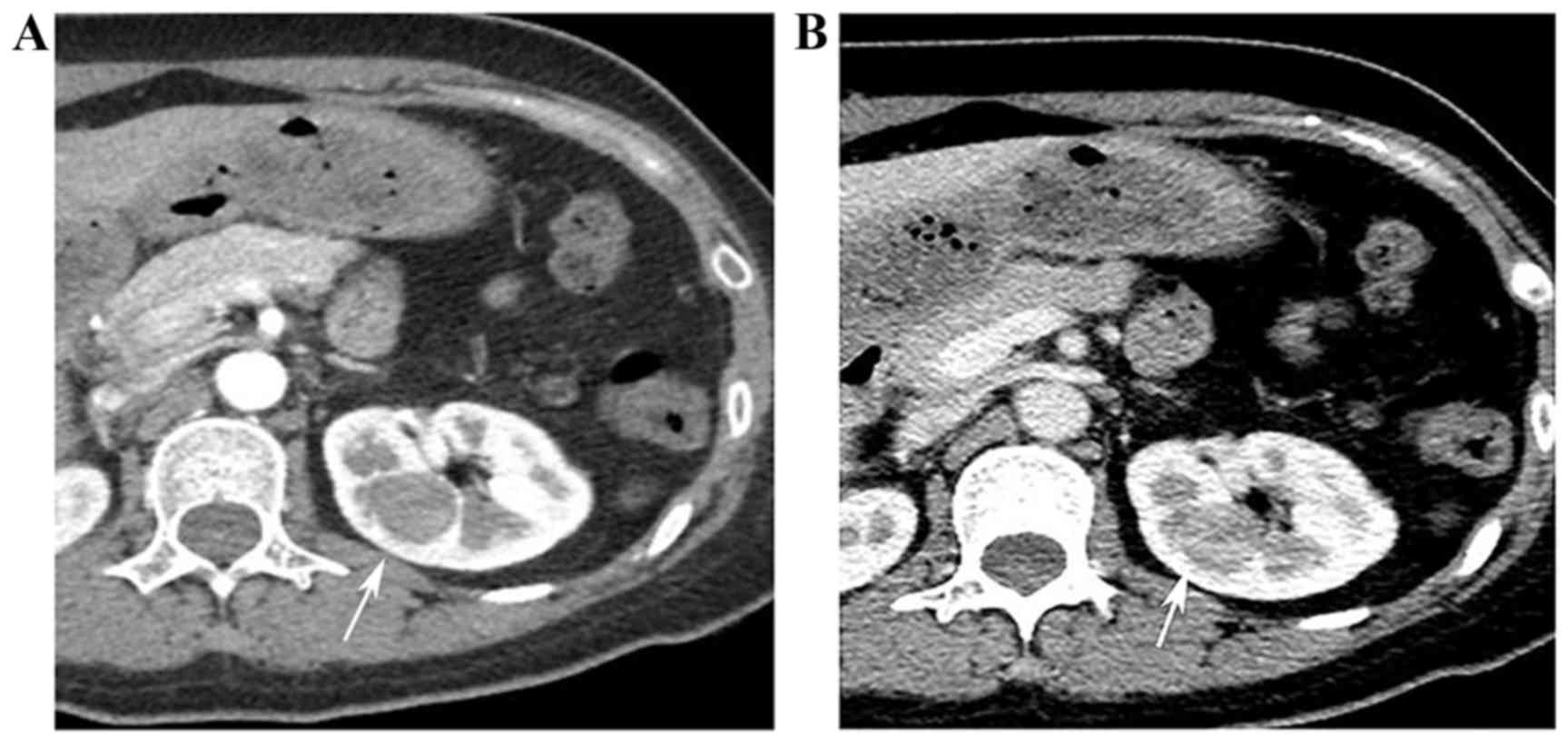
A total of 2 months later, a follow-up computed
tomography (CT) angiography scan revealed normal renal arteries,
but confirmed the presence of a 2.2-cm mass in the left kidney, as
exhibited in Fig. 3. The mass showed
no marked enhancement during the arterial phase, and a slight
enhancement during the portal venous phase. There was no change in
the size of the lesion. The patient underwent a laparoscopic left
partial nephrectomy to remove the lesion on the left kidney. The
surgical procedure was successful, with no intraoperative or
postoperative complications. The BP of the patient showed a
substantial reduction from 177/115 to 125/80 mmHg on the day
subsequent to surgery, and stabilized to be within the normal
range. As a result, all antihypertensive therapies were
discontinued 1 week later. The BP of the patient remained in the
normal range subsequent to a 6-month follow-up.
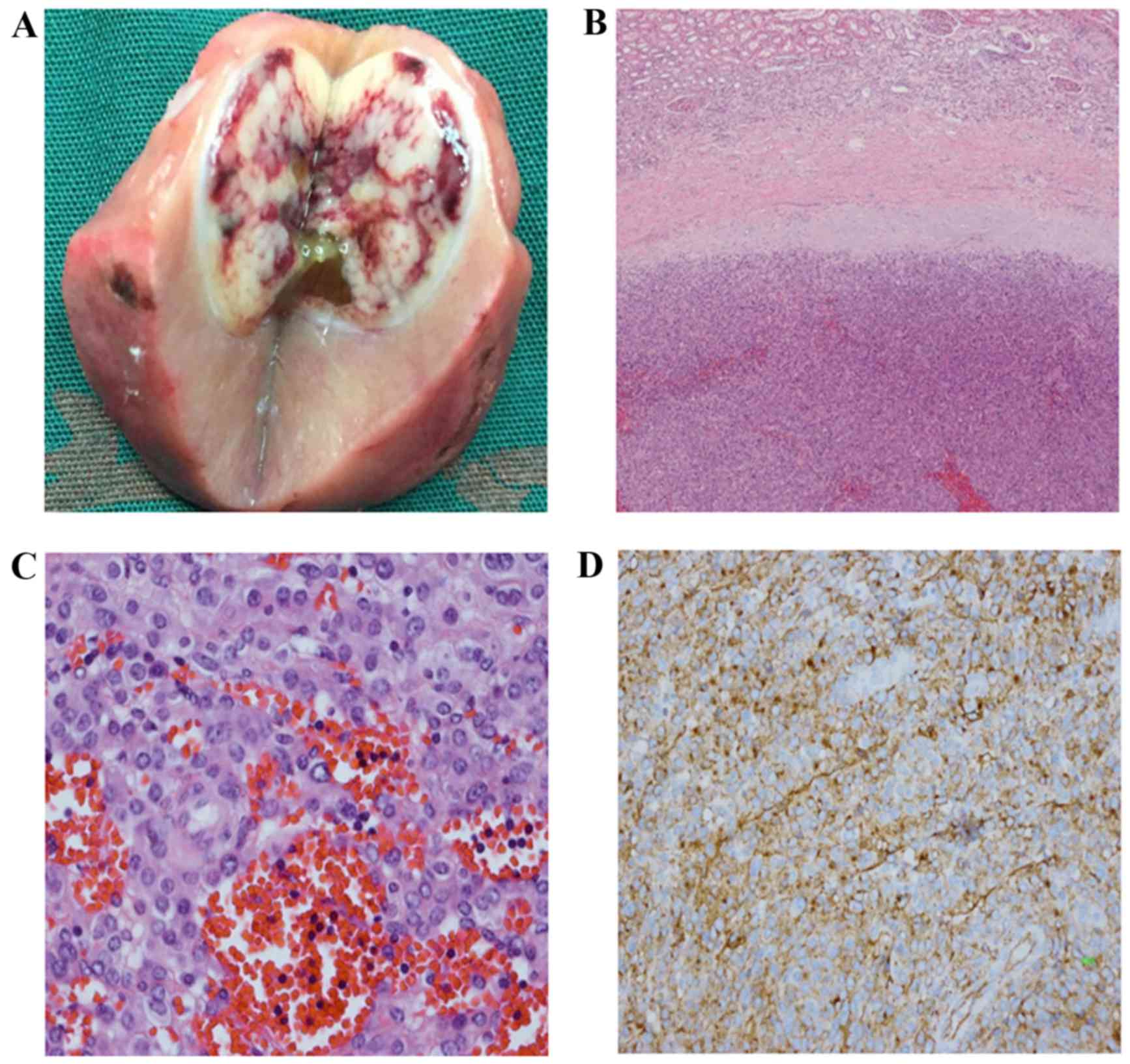
Gross examination of the left partial nephrectomy
sample showed a solitary, well-circumscribed tumor measuring 2 cm,
with a grey-white colored section and some areas of hemorrhage, as
demonstrated in Fig. 4A. The
histological analysis revealed that the tumor cells were arranged
solidly, or as amorphous plaques, exhibiting clear borderlines with
the renal cortex (Fig. 4B). The tumor
was composed of round and polygonal cells with eosinophilic
cytoplasm, and regular cell nuclei and perinuclear halos were
observed (Fig. 4C). During
immunohistochemical analysis, the round uniform cells were stained
and produced a strong positive result for the presence of the
vascular marker cluster of differentiation (CD)34 (Fig. 4D), and a negative result for the
presence of keratin AE1 andAE3, smooth muscle actin, chromogranin
A, Syn, RCC, HMB45, S100, CD31 and Ki-67 markers. In conjunction
with the clinical history, the histological findings and
immunohistochemical analysis supported a diagnosis of reninoma.
Discussion
Reninoma is a benign neoplasm that produces renin
and results in secondary hypertension with hyperaldosteronism and
hypokalemia. Occasionally, the tumors exhibit malignant behavior
(6–9).
The incidence of reninoma is low: Since the first description in
1967 by Robertson et al (10),
~100 cases have been reported, the majority of which occur in young
adult females with a mean age of 27 years (11).
Among the number of reninoma cases reported
(12–17), the patient of the present study case
is the 7th study reporting a patient with reninoma during
pregnancy. According to previous studies, the majority of reninomas
present in the form of solitary tumor (11,18). The
coexistence of reninoma and bilateral pheochromocytoma has been
previously reported (19), whereas
the present study is the first case report of reninoma coexisting
with an adrenal adenoma.
There are many data suggesting that secondary
hypertension may be caused by several conditions, affecting the
kidneys, heart, arteries or endocrine system. Common causes include
renovascular hypertension, PA and pheochromocytoma (20). PA is considered to be the major common
cause of secondary hypertension (21), which results from the inappropriate
endogenous production of the mineralocorticoid aldosterone by the
adrenal glands. The condition is also caused by solitary or
multifocal aldosterone-producing adenomas, or less commonly by
adrenal gland hyperplasias (22). As
the patient in the present study exhibited neoplasms in the right
adrenal gland and in the left kidney, the hypertension was presumed
a result of PA, which was incorrect.
It is difficult to accurately diagnose the pathogeny
of hypertension based solely on radiology imaging; lab examination
is effective in achieving a correct diagnosis. Reninoma and PA are
associated with hypokalemia, hyperaldosteronism and hypertension.
Reninoma produce excessive amounts of renin, which results in
secondary hyperaldosteronism, with the plasma renin levels
remaining normal in PA patients (23). The level of hypertension of the
patient was mistakenly linked to the right adrenal tumor when the
patient was referred to the Chinese Academy of Medical Sciences
Cancer Institute and Hospital (Beijing, China) prior to testing the
level of renin. Retrospective analyses of the medical examinations
of the patient were carried out by the Beijing Shijitan Hospital
(Beijing, China), where the patient gave birth, and demonstrated
that the renin level of the patient of the present study was
clearly higher than the normal range, which provides additional
evidence to support the hypothesis that the neoplasm in the left
kidney of this patient was a reninoma. The laboratory examinations
demonstrated hypokalemia, with levels of serum potassium measuring
3.48 mmol/l, whereas the normal range is 3.5–5.3 mmol/l. Plasma
renin, angiotensin II and aldosterone levels were elevated in the
supine and upright positions (renin: 19.40 and 24.30 ng/ml/h;
angiotensin II: 370.20 and 425.30 pg/ml; aldosterone: 19.22 and
27.18 ng/dl), demonstrating that laboratory tests are useful for
differential diagnosis.
Reninomas are difficult to identify with ultrasound
technology, even in cases of known renal lesion. Therefore, if a
reninoma is suspected, particularly in females with severe
hypertension, CT or MRI scans may be considered as the primary
diagnostic tool for screening renal tumors, in comparison with
ultrasound scans. Small isodense lesions may not be detected by
unenhanced CT scans: Therefore, enhanced CT scans may be performed
for all suspected cases (18). Rosei
et al (24) reported that CT
scans are particularly sensitive at detecting this kind of tumor
compared with MRI scans, as MRI scans may produce misleading
results.
The radiological features of reninoma have been
documented, presenting as hypo- or isodense solid masses with
well-defined borders on an unenhanced CT scan, and remaining
hypovascular on arterial phase images due to the vasoconstriction
caused by the renin excreted from the tumor. Results from the MRI
T1-weighted images demonstrate tumors in iso- or hypointense areas,
whilst on the T2-weighted images they appear as hyperintense
(25).
In conclusion, the present study described a rare
case of reninoma coexisting with an adrenal adenoma during
pregnancy. Reninoma should be included in the differential
diagnoses of incidences of solitary regular renal masses with a
slight enhancement in patients with hypertension, particularly in
young females. Enhanced CT and MRI scans should be performed when
reninoma is suspected. In addition, laboratory tests are highly
recommended in differentiating reninoma.
Glossary
Abbreviations
Abbreviations:
|
T2WI
|
T2 weighted-image
|
|
T1WI
|
T1 weighted-image
|
|
PA
|
primary aldosteronism
|
References
|
1
|
Corvol P, Pinet F, Plouin PF, Bruneval P
and Menard J: Renin-secreting tumors. Endocrinol Metab Clin North
Am. 23:255–270. 1994.PubMed/NCBI
|
|
2
|
Dong D, Li H, Yan W, Xu W, Lu L and Zeng
Z: The diagnosis and surgical anagement of juxtaglomerular cell
tumor of the kidney. J Hypertens. 28:628–632. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Szejnfeld D, Nunes TF, Giordano EE, Freire
F, Ajzen SA, Kater CE and Goldman SM: Radiofrequency ablation of
functioning adrenal adenomas: Preliminary clinical and laboratory
findings. J Vasc Interv Radiol. 26:1459–1464. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Rayner B: Primary aldosteronism and
aldosterone-associated hypertension. J Clin Pathol. 61:825–831.
2008. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Rossi GP, Bernini G, Caliumi C, Desideri
G, Fabris B, Ferri C, Ganzaroli C, Giacchetti G, Letizia C,
Maccario M, et al: A Prospective study of the prevalence of primary
aldosteronism in 1,125 hypertensive patients. J Am Coll Cardiol.
48:2293–2300. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Shera AH, Baba AA, Bakshi IH and Lone IA:
Recurrent malignant juxtaglomerular cell tumor: A rare cause of
malignant hypertension in a child. J Indian Assoc Pediatr Surg.
16:152–154. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Duan X, Bruneval P, Hammadeh R, Fresco R,
Eble JN, Clark JI, Vigneswaran WT, Flanigan RC and Picken MM:
Metastatic juxtaglomerular cell tumor in a 52-year-old man. Am J
Surg Pathol. 28:1098–1102. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Beaudoin J, Périgny M, Têtu B and Lebel M:
A patient with a juxtaglomerular cell tumor with histological
vascular invasion. Nat Clin Pract Nephrol. 4:458–462. 2008.
View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Dong D, Li H, Yan W and Xu W:
Juxtaglomerular cell tumor of the kidney-a new classification
scheme. Urol Oncol. 28:34–38. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Robertson PW, Klidjian A, Harding LK,
Walters G, Lee MR and Robb-Smith AH: Hypertension due to a
renin-secreting renal tumour. Am J Med. 43:963–976. 1967.
View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Wong L, Hsu TH, Perlroth MG, Hofmann LV,
Haynes CM and Katznelson L: Reninoma: Case report and literature
review. J Hypertens. 26:368–373. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Henderson NL and Mason RC: Juxtaglomerular
cell tumor in pregnancy. Obstet Gynecol. 98:943–945. 2001.
View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Kim HJ, Kim CH, Choi YJ, Ayala AG,
Amirikachi M and Ro JY: Juxtaglomerular cell tumor of kidney with
CD34 and CD117 immunoreactivity: Report of 5 cases. Arch Pathol Lab
Med. 130:707–711. 2006.PubMed/NCBI
|
|
14
|
Lachvac L, Svajdler M, Valansky L, Nagy V,
Benicky M, Frohlichova L and Nyitrayova O: Juxtaglomerular cell
tumor, causing fetal demise. Int Urol Nephrol. 43:365–370. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Shin YS, Cha JS, Kang MJ, Park JK, Kim HJ
and Kim MK: Newly developed hypertension due to juxtaglomerular
cell tumor in pregnancy. Clin Nephrol. 78:325–327. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Ohashi Y, Kobayashi S, Arai T, Nemoto T,
Aoki C, Nagata M and Sakai K: Focal segmental glomerulosclerosis
secondary to juxtaglomerular cell tumor during pregnancy: A case
report. Case Rep Nephrol Urol. 4:88–94. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Diker-Cohen T, Abraham SB, Rauschecker M,
Papadakis GZ, Munir KM, Brown E, Lyssikatos C, Belyavskaya E,
Merino M and Stratakis CA: Reninoma presenting in pregnancy. J Clin
Endocrinol Metab. 99:2625–2626. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Gottardo F, Cesari M, Morra A, Gardiman M,
Fassina A and Dal Bianco M: A kidney tumor in an adolescent with
severe hypertension and hypokalemia: An uncommon case-case report
and review of the literature on reninoma. Urol Int. 85:121–124.
2010. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Paragliola RM, Capoluongo E, Torino F,
Minucci A, Canu G, Prete A, Pontecorvi A and Corsello SM: A rare
case of juvenile hypertension: Coexistence of type 2 multiple
endocrine neoplasia-related bilateral pheochromocytoma and reninoma
in a young patient with ACE gene polymorphism. BMC Endocr Disord.
15:302015. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Baglivo HP and Sánchez RA: Secondary
arterial hypertension: Improvements in diagnosis and management in
the last 10 years. Am J Ther. 18:403–415. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Young WF: Primary aldosteronism:
Renaissance of a syndrome. Clin Endocrinol (Oxf). 66:607–618. 2007.
View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Layden BT, Hahr AJ and Elaraj DM: Primary
hyperaldosteronism: Challenges in subtype classification. BMC Res
Notes. 5:6022012. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Kim SH, Ahn JH, Hong HC, Choi HY, Kim YJ,
Kim NH, Yoo HJ, Kim HY, Seo JA, Kim NH, et al: Changes in the
clinical manifestations of primary aldosteronism. Korean J Intern
Med. 29:217–225. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Rosei CA, Giacomelli L, Salvetti M, Paini
A, Corbellini C, Tiberio G and Muiesan ML: Advantages of renin
inhibition in a patient with reninoma. Int J Cardiol. 187:240–242.
2015. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Karaosmanoğlu AD, Onur MR, Shirkhoda A,
Ozmen M and Hahn PF: Unusual benign solid neoplasms of the kidney:
Cross-sectional imaging findings. Diagn Interv Radiol. 21:376–381.
2015. View Article : Google Scholar : PubMed/NCBI
|