A total of 167 adult patients
undergoing maximal safe resection of newly diagnosed World Health
Organization grade 4 IDH-wt glioblastoma were included. The
variables of interest (MPV, PT ratio, and aPTT ratio) were
dichotomized at the median, while the overall PLT count was split
using the central distribution (10th to 90th percentile).
Correlation analyses of markers with tumoral and demographic
characteristics, Kaplan Meier survival analysis, and Cox
multivariate regression analysis were conducted to assess the
single contributions of these parameters in building a predictive
model of overall survival (OS) in these patients.
The mean baseline MPV correlated with increasing age
(r=0.18, P=0.01), the overall fluid-attenuated inversion recovery
tumoral volume (r=0.17, P=0.02), and lesion T1-weighted
post-contrast sequence (T1-CE) volume (r=0.19, P=0.01). The median
OS in the whole cohort of patients with GBM was 14.4 months (95% CI
12.9-17.6). Patients with MPV >10.3×10−15 l had a
median OS of 13.4 months (95% CI 10.6-17.6) compared with 14.5
months (95% CI 13.4-20.6) in patients with MPV
≤10.3×10−15 l (P=0.028). Similarly, shorter OS was
recorded in patients with PT ratio >1.01 (12.3 months, 95% CI
10.2-15.1 vs. 17.6 months, 95% CI 13.4-20.6; P=0.006) and PLT count
out-of-range 165–300×109/l (11.5 months, 95% CI 8.8-16.3
vs. 14.7 months, 95% CI 13.4-19.1; P=0.026). A subgroup analysis of
patients >65 years of age confirmed baseline MPV >10.3
10−15 l was associated with shorter OS (9.4 months, 95%
CI 8.1-13.4) compared with 13.3 months (95% CI 11.3-32.3, P=0.028)
for those with MPV ≤10.3×10−15 l. Baseline-increased MPV
showed an independent predictive role for poor survival (HR, 1.56;
95% CI 1.13-2.16; P=0.006) in multivariate analysis accounting for
age, gender, performance status, extent or resection, adjuvant
therapies, and tumoral molecular and radiological characteristics,
whereas PLT count within the central range predicted longer OS (HR,
0.26; 95% CI 0.13-0.54; P<0.001).
The present study indicates a possible association
between tumoral burden and systemic hemostasis activation in
patients with IDH-wt GBM. Increased MPV and deranged PLT outside
the central range demonstrated an independent role in predicting
shorter OS, which was even more prominent among older patients.
These findings require additional studies to further validate these
results and specifically characterize GBM pathological features of
aggressiveness related to hemostasis activation, neo-angiogenesis,
the tumor immune microenvironment, and their effect on response to
treatments and OS.
Introduction
Glioblastoma (GBM) is the most common, fast-growing,
and aggressive malignant primary CNS tumor worldwide, accounting
for 48.6% of malignant central nervous system tumors (1), with an incidence of 3–4 cases per
100,000 person-years (2). The
median survival time is ~15 months, despite the use of surgery and
adjuvant treatments (3). The
diagnosis of GBM is currently defined by the 2021 World Health
Organization (WHO) classification of CNS tumors (4), which uses integrated molecular marker
analysis and chromosomal aberrations. GBM WHO grade 4 is defined as
a diffuse astrocytic glioma, with isocitrate dehydrogenase (IDH),
histone 3 (H3) and wild type (wt) features, and characterized by
prominent cellular and nuclear atypia, frequent mitotic activity,
necrosis, and vascular proliferation. Telomerase reverse
transcriptase (TERT) promoter mutation, epidermal growth factor
receptor (EGFR) gene amplification, and +7/-10 chromosome
copy-number changes characterize the specific molecular features.
Current GBM treatment is multimodal and has not been substantially
changed since 2005, despite notable efforts in neuro-oncological
research. GBM treatment consists of maximal safe resection surgery,
followed by concomitant adjuvant radiotherapy and chemotherapy
(3).
In recent years, there has been a growing study of
the potential contribution of hemostasis and platelet activation in
cancer biology (5–18). Although the exact interplay between
circulating blood cells, peritumoral immune infiltrate, and
intra-tumoral microenvironment is still not fully understood, the
relevance of cancer-induced systemic activation of soluble and
cellular hemostasis components in promoting tumor growth and
progression has been increasingly emphasized (19). The mechanism of platelet-induced
tumorigenesis and progression has only been partly elucidated and
is thought to be mainly associated with the role served by
activated platelets in sustaining tumoral neo-angiogenesis via the
release of pro-angiogenic factors contained in α-granules.
Additionally, the excessive and unbalanced release of
pro-thrombotic molecules and pro-inflammatory cytokines results in
changes in the thrombotic/fibrinolytic balance, and the recruitment
of circulating leukocytes, contributing to their extravasation and
polarization towards immune-permissive subpopulations which
contribute to immune escape (20,21).
These mechanisms, together, contribute to the promotion of cellular
evasion and metastatic seeding (19).
Platelet number and morphology are evaluated through
routine, low-cost blood tests, such as platelet count (PLT count)
and mean platelet volume (MPV). The latter is considered a feature
of platelets' activation, with increased MPV indicating activation
of a large number of platelets (22). Given this, the PLT count and MPV
have been used as diagnostic markers in solid tumors, as they have
proved helpful in distinguishing malignant from benign lesions in
hepatic, nasopharyngeal, and colorectal cancer (12,14).
Additionally, MPV has been reported to show prognostic value in
predicting shorter OS in certain types of solid cancers including
esophageal, gastric (23),
pancreatic (24), lung (25), breast, colorectal, head and neck,
hepatic, urothelial cancer, melanoma and osteosarcoma, and
hematologic cancers including multiple myeloma and diffuse large
B-cell lymphoma (23–25).
The present study addressed the association of
baseline pre-operative PLT count, MPV, coagulation profile
including prothrombin time (PT), prothrombin ratio (PT ratio),
activated partial thromboplastin time (aPTT), and aPPT ratio with
demographic and tumoral parameters, and their impact on OS in
patients with GBM.
Materials and methods
Study design, patient selection, and
data retrieval
The present study was a single-center,
retrospective, non-controlled clinical study, designed to assess
the role of platelet activation and the coagulation profile in
patients with GBM. Patients with adequate clinical follow-up, who
underwent maximal safe resection of newly diagnosed grade 4
isocitrate dehydrogenase-wildtype (IDH-wt) glioblastoma at IRCCS
San Raffaele Hospital (Milan, Italy) between 2016 and 2023 were
included. Pediatric patients (<18 years of age) and patients who
demonstrated unresectable disease, underwent biopsy only, had
IDH-mutant tumors, or recurrent GBM were excluded from the current
analysis.
Diagnoses were originally performed according to the
2016 World Health Organization (WHO) classification of tumors of
the central nervous system (26) or
the 2021 WHO edition (4), depending
on when surgery was performed. As the intent of the present study
was to analyze a homogenous population of ‘primary’ (i.e., IDH-wt)
GBM, cases defined as ‘secondary’ or ‘IDH-mutated’ lesions were
excluded (27). Between January
2016 and December 2021, only patients who presented a diagnosis of
IDH-wt GBM through immunohistochemical detection of the absence of
IDH1 R132 mutations were enrolled (n=136).
After January 2021, only GBM IDH-wt patients
according to the 2021 WHO classification were included (n=31).
IDH1-2 mutational status was determined, and all cases whose IDH
status was not available were excluded. Pathological and molecular
findings such as O-6-methylguanine-DNA-methyltransferase (MGMT)
promoter methylation status, Ki-67 index, and p53 expression were
reported. Testing for TERT mutation was not routinely performed
before 2021 at the IRCCS San Raffaele Hospital, therefore only a
subset of patients in this cohort had TERT mutation status data.
Specimens were processed and analyzed at the Department of
Pathology (San Raffaele Scientific Institute) as per standard of
care methods for diagnosis, according to WHO standards (4,26).
Briefly, for immunohistochemistry, 2 µm thick paraffin-embedded
representative tissue sections were de-waxed in xylene and
rehydrated using 3×10 min 99% ethanol and 2×10 min 96% ethanol
washes. Endogenous peroxidase activity was blocked with 0.3%
H2O2 in methanol for 20 min. Antigen
retrieval (when necessary) was performed by using a microwave oven
or a thermostatic bath at 98°C for 40 min in either 1.0 mM EDTA
buffer (pH 8.0) or 1 mM Citrate buffer (pH 6.0). Sections were then
washed in TBS (pH 7.4), and incubated in the specific primary
antibody at 37°C for 30 min. The signal was revealed using the DAKO
Envision + System-HRP Labelled Polymer Anti-Rabbit or Anti-Mouse
(Novocastra™) followed by DAB as chromogen and hematoxylin as
counterstain, according to the manufacturer's instructions. The
primary antibodies used were as follows: mouse monoclonal anti-p53
(Prediluted; clone DO-7; cat. no. 800-2912; Roche Tissue
Diagnostics; Roche Diagnostics, Ltd.), rabbit monoclonal anti-Ki-67
(clone 30-9; Prediluted; cat. no. 790-4286; Roche Tissue
Diagnostics; Roche Diagnostics, Ltd.), rabbit polyclonal anti-ATRX
(1:300; cat. no. PA5-21348; Sigma-Aldrich), rabbit monoclonal
anti-GFAP (Prediluted; clone EP672Y; cat. no. 760-4345; Roche
Tissue Diagnostics; Roche Diagnostics, Ltd.), mouse monoclonal
anti-IDH1 R132H (1:100; clone H09; cat. no. DIA-H09; Dianova GmbH).
In cases with negative immunostaining for IDH1-R132H, IDH1/2
mutational status was assessed using Illumina MiSeq (Myriapod NGS
Kit Cancer panel DNA, Diatech Pharmacogenetics) according to the
manufacturer's protocol. Evaluation of O6-methylguanine DNA
methyltransferase (MGMT) promoter methylation status was performed
using a pyrosequencing methylation assay using the MGMT PLUS kit CE
IVD (Diatech Pharmacogenetics) according to manufacturer's
instructions.
Tumoral volumes were calculated on preoperative MRI
imaging using Cranial Planning Anatomical Mapping (version 1.1.1.8)
and SmartBrush (version 3.0.0.92) (Brainlab AG) to assess
fluid-attenuated inversion recovery (FLAIR) and T1-weighted
post-contrast sequences (T1-CE). The presence of satellite lesions
was defined as the occurrence of hyperintense signals in the FLAIR
sequence non-contiguous with the target lesion and therefore
outside the planned surgical field. The extent of resection (EOR)
was calculated on MRI imaging performed within 72 h post-surgery
when available, or on MRI scans performed for RT planning, before
any additional treatment as per Response Assessment in
Neuro-Oncology guidelines (28).
Baseline and follow-up clinical data were retrospectively retrieved
from clinical records and included age, gender, and performance
status using the Karnofsky score (29).
Blood sampling
Preoperative peripheral blood samplings including
PLT count (normal range, 130–400×109/l), MPV (normal
range 9.1-12.5×10−15 l), PT ratio (normal range
0.85-1.18) and aPTT ratio (normal range 0.8-1.23) were routinely
performed upon hospital admission, before any treatment, and within
the 24 h period preceding surgery. Specimens were processed
immediately after collection in the IRCCS Ospedale San Raffaele
Hospital central analysis laboratory as per the normal standard of
care.
Statistical analysis
Statistical analysis was performed using R Core Team
(2022) (30), using survival
(version 3.5-5) (31), ggsurvfit
(version 1.0) (32), corrplot
(version 0.92) (33), and ggplot2
(version 1.0) (34) packages.
Categorical variables are reported as absolute numbers and
percentages whereas continuous variables are reported as mean and
standard deviation or median and interquartile range. The
difference in baseline characteristics and the unadjusted
univariate analyses were performed using Student's t-test or
Mann-Whitney U test in accordance with the normality of the
distribution. χ2 and Fisher's exact test, were used
depending on the expected count.
Pearson's correlation test was used to infer
associations between demographics, clinical and serum markers
variables, and mortality. The continuous variables of interest
(MPV, PT, and aPTT) were dichotomized at the median, whereas the
PLT count was taken from the central range (10th to 90th
percentile) and two-sided lower and upper ‘out-of-range’ tails. The
Kaplan-Meier method was used to estimate OS in the study population
using the newly dichotomized variables. To address the association
between serum markers and age, a subgroup analysis of an older
patient population (>65 years) was conducted utilizing the same
cut-offs for the continuous variables. The log-rank test was used
to analyze differences between groups. Univariate and multivariate
Cox regression analyses were used to detect variables associated
with increased overall survival. P<0.05 was considered to
indicate a statistically significant difference. A two-stage
procedure for comparing hazard rate functions was applied using the
TSHRC (version 0.1-6) package (35), when the proportional hazard
assumption was violated.
Results
Patients, pathological
characteristics, and treatments
A total of 167 patients with WHO grade 4 IDH-wt GBM
were included in the present study. The mean age of the patients
was 63±10.5 years. Most of the patients were male (n=111, 66%) and
aged <65 years old (n=92, 55.1%). Overall, patients displayed a
good functional status using Karnofsky performance status (KPS
>80) in 63.4% of cases. Patients were followed up clinically for
a median period of 12.8 months. A comprehensive summary of the
baseline characteristics of included patients, tumors, and
peripheral markers is presented (Table
I). Assessment of MGMT promoter status was available in 134
patients (80%) and revealed promoter hypermethylation in 49/134
(37%) patients. The quantitative analysis of ki67 and p53 reported
a mean of 31±18 and 20±24% immunoreactive cells, respectively. EGFR
amplification and TERT mutation data were available in <10% of
patients and therefore were not included in the present
analysis.
 | Table I.Baseline characteristics of included
patients, and lesions characteristics. |
Table I.
Baseline characteristics of included
patients, and lesions characteristics.
| Epidemiology
characteristics | Value | n | Percentage (%) |
|---|
| Age (years) |
|
| . |
|
Mean | 63±10.5 |
|
|
|
<65 |
| 92 | 55 |
|
≥65 |
| 75 | 45 |
| Gender |
|
|
|
|
Male |
| 111 | 66 |
|
Female |
| 56 | 34 |
| Median KPS | 80 (70–90) |
|
|
| Tumor
characteristics |
|
|
|
| Mean
FLAIR volume, cm3 | 98.3±59.2 |
|
|
| Mean
T1-CE volume, cm3 | 34.5±26.7 |
|
|
|
Satellite FLAIR lesions |
| 28 | 17 |
| Genetics (sample
size) |
|
|
|
| MGMT
met (134) |
| 49 | 37 |
| Mean
Ki67 (136) |
|
| 31±18 |
| Mean
p53 (138) |
|
| 20±24 |
| Extent of resection
(n=167) |
|
|
|
|
Complete |
| 69 | 41 |
| Near
total |
| 51 | 31 |
|
Partial |
| 13 | 8 |
|
Subtotal |
| 34 | 20 |
| Postoperative
protocol (n=149) |
|
|
|
|
Completed concurrent
RT/TMZ |
| 115 | 77 |
| RT
only/incomplete RT/TMZ |
| 34 | 23 |
| Adjuvant treatments
(n=129) |
|
|
|
|
Adjuvant TMZ |
| 107 | 83 |
| 6
cycles |
| 54 | 42 |
| 12
cycles |
| 9 | 7 |
| Mean preoperative
blood test markers |
|
|
|
| PLT,
×109/l | 240±78.7 |
|
|
| MPV,
×10−15 l | 10.3±0.98 |
|
|
| PT ratio | 1.01±0.11 |
|
|
| aPTT ratio | 0.94±0.10 |
|
|
| Overall
survival |
|
|
|
|
Dead |
| 129 | 77 |
|
Alive |
| 38 | 23 |
The EOR was retrieved for all included patients and
calculated as complete in 69 (41%), near total in 51 (31%), partial
in 13 (8%), and subtotal in 34 (20%). Post-operative treatment data
were available for 149 patients (89%). Among them, the
post-operative concurrent radiotherapy (RT) and chemotherapy with
temozolomide (TMZ) regimen were completed in 115 (77%) patients,
conversely, the remaining 34 (23%) only received RT or did not
complete the concurrent RT/TMZ regimen for TMZ. Data on additional
adjuvant therapies was available for 129 patients (73%). Most of
these received adjuvant TMZ (n=107, 83%) completing 6 cycles in 42%
of cases and 12 cycles in 7% of cases.
Cut-off selection and baseline
characteristics of pre-operative laboratory parameters
The blood marker values of MPV, PT, PT ratio, aPTT,
and aPTT ratio were split at the median. The resultant thresholds
for survival analysis were as follows: MPV, 10.3×10−15
l; PT, 13.2 sec; PT ratio, 1.01; aPTT, 28.4 sec; and aPTT ratio,
0.94. The PLT count was split up using the central distribution
(10th to 90th percentile) which corresponded to the range of
165–300×109/l.
The baseline demographic characteristics of patients
were not significantly different between patients with high and low
MPVs, except for age (64.7±10.8 vs. 60.8±9.96 years, respectively;
P=0.01). No significant differences in baseline performance status,
steroid use (dexamethasone), inflammatory markers (white blood cell
count and neutrophil count), or molecular signature were detected.
Patients with MPV >10.3×10−15 l had slightly larger
T1-CE volumes (P=0.07). Univariate analysis for MPV is presented
(Table II).
 | Table II.Univariate analysis of baseline
characteristics of patients and lesions in low-MPV compared with
high-MPV cohorts. |
Table II.
Univariate analysis of baseline
characteristics of patients and lesions in low-MPV compared with
high-MPV cohorts.
| Preoperative
characteristics | MPV ≤10.3
(×10−15 l) (n=77) | MPV >10.3
(×10−15 l) (n=88) | P-value |
|---|
| Age, mean ± SD | 60.8±9.96 | 64.7±10.8 | 0.01 |
| Male, n (%) | 54 (70.1) | 55 (62.5) | 0.30 |
| Female, n (%) | 23 (29.9) | 33 (37.5) | 0.30 |
| Performance
status |
|
|
|
| KPS, median
(IQR) | 80 (70–90) | 80 (70–90) | 0.45 |
| Inflammation
markers |
|
|
|
| WBC,
109/l | 10.3±3.88 | 10.2±3.7 | 0.76 |
|
Neutrophils,
109/l | 7.98±4.01 | 8.20±3.97 | 0.73 |
| Pathology |
|
|
|
|
Presence of central necrosis
(n, %) | 68 (90.6) | 73 (85.8) | 0.35 |
| Midline
shift > 5 mm | 27 (36.4) | 39 (45.3) | 0.25 |
| Mean
FLAIR volume (cm3) | 92.3±54.2 | 105.2±63.2 | 0.17 |
| Mean
T1-CE volume (cm3) | 31.6±25.9 | 37.6±27.4 | 0.07 |
| Presence of
satellite FLAIR lesions (n, %) | 16 (21.6) | 11 (12.9) | 0.14 |
| Genetics |
|
|
|
| MGMT
methylation, (n, %) | 23 (35.9) | 26 (37.6) | 0.85 |
| p53 (%
immunoreactive cells) | 0.22±0.26 | 0.18±0.23 | 0.38 |
| Ki67 (%
immunoreactive cells) | 0.31±0.18 | 0.31±0.19 | 0.92 |
| Mean daily dose
pre-operative dexamethasone (mg) | 5.32±7.7 | 6.12±8.1 | 0.58 |
Similarly, patients with increased PT ratio showed
slightly greater mean age (64.8±10.4 vs. 60.4±10.2 years, P=0.009)
compared with patients with lower values. All other parameters were
otherwise comparable in these patients as well as in the other
study groups (aPTT ratio and PLT count).
Survival analysis
Pre-operative laboratory parameters
The median OS in the whole cohort of patients with
GBM was 14.4 months (95% CI, 12.9-17.6). The median OS of patients
with a PLT count out of the central range was significantly shorter
than that of patients with PLT in the central range (165–300
109/l) with a median OS of 11.5 months (95% CI,
8.8-16.3) compared with 14.7 months (95% CI, 13.4-19.1) (P=0.026,
Fig. 1A).
Patients with MPV >10.3×10−15 l had a
median OS of 13.4 months (95% CI, 10.6-17.6) compared with 14.5
months (95% CI, 13.4-20.6) in patients with MPV
≤10.3×10−15 l (P=0.028, Fig.
1B). Similarly, patients with PT ratio >1.01 achieved a
median OS of 12.3 months (95% CI, 10.2-15.1) compared with 17.6
months (95% CI, 13.4-20.6) in patients with PT ratio ≤1.01
(P=0.006, Fig. 1C). However, the
difference in median OS of patients with baseline aPTT ratio
>0.94 of 12.2 months (95% CI: 10.2-17) was not significantly
different to the 14.6 months (95% CI, 13.4-20.4) of patients with
aPTT ≤0.94 (P=0.06, Fig. 1D).
Age and performance status
Patients aged >65 years had a median OS of 11
months (95% CI, 9.5-14.7) which was significantly shorter when
compared with the 20.2 months (95% CI, 14.7-23) in younger patients
(P<0.001; Fig. S1A).
The median OS for patients with low (<70) and
high (≥80) KPS were 12 (95% CI, 9.6-16.3) and 14.7 months (95% CI,
13.4-19.8), respectively (P=0.03; Fig.
S1B).
Gender, MGMT status, and satellite
lesions
Survival analysis for gender (P=0.57, Fig. S1C) and MGMT methylation (P=0.14,
Fig. S1D) status did not indicate
any significant differences in OS in this patient cohort. However,
female patients did achieve a gain in OS against males in the
subgroup of patients with MGMT promoter methylation (OS 24.8 months
with 95% CI 14.6-32 vs. 14.5 months with 95% CI 13.3-20.2; P=0.04;
Fig. S1E). The presence of
satellite FLAIR lesions was associated with a significantly shorter
OS, of 11.5 months (95% CI, 8.7-14.4) for the additional areas
group compared with 15.1 months (95% CI, 13.4-18.7) for the
unifocal group (P=0.02; Fig.
S1F).
Subgroup analysis in patients aged
>65 years
Additional survival analysis in the older subgroup
of patients (>65 years of age) was conducted to evaluate the
association between increased age and baseline MPV and PT. Besides
a worse overall performance status (KPS) compared with younger
patients (P=0.001), no other variables including tumoral volumes,
mutations, ki67 status, or demographic parameters differed in the
two populations.
PLT count within range and aPTT ratio did not show
any significant difference in terms of OS (Fig. S2A and D). However, patients with
MPV >10.3×10−15 l demonstrated a shorter median OS of
9.4 months (95% CI, 8.1-13.4) compared with 13.3 months (95% CI,
11.3-32.3) for patients with MPV ≤10.3×10−15 l (P=0.028,
Fig. S2B). Similarly, patients
with a high PT ratio (>1.01) achieved OS of 8.9 months (95% CI,
8.1-11.3) compared with 13.8 months (95% CI, 11.4-23.1) for
patients with a low PT ratio (P=0.01, Fig. S2C).
Additionally, to further test the interaction of age
and MPV in OS, the relative mortality rate of patients with
increased or decreased MPV values in the 2 subgroups of patients
with different ages, were calculated. Within the elderly group
(>65 years) the mortality rate for patients with increased vs.
decreased MPV was 31/32 (97%) vs. 11/15 (73%). In the younger group
of patients (<65 years) it was 44/58 (76%) vs. 43/62 (69%) and
the effect of age and MPV on OS rate was not statistically
significant (P=0.092).
Correlation and regression
analyses
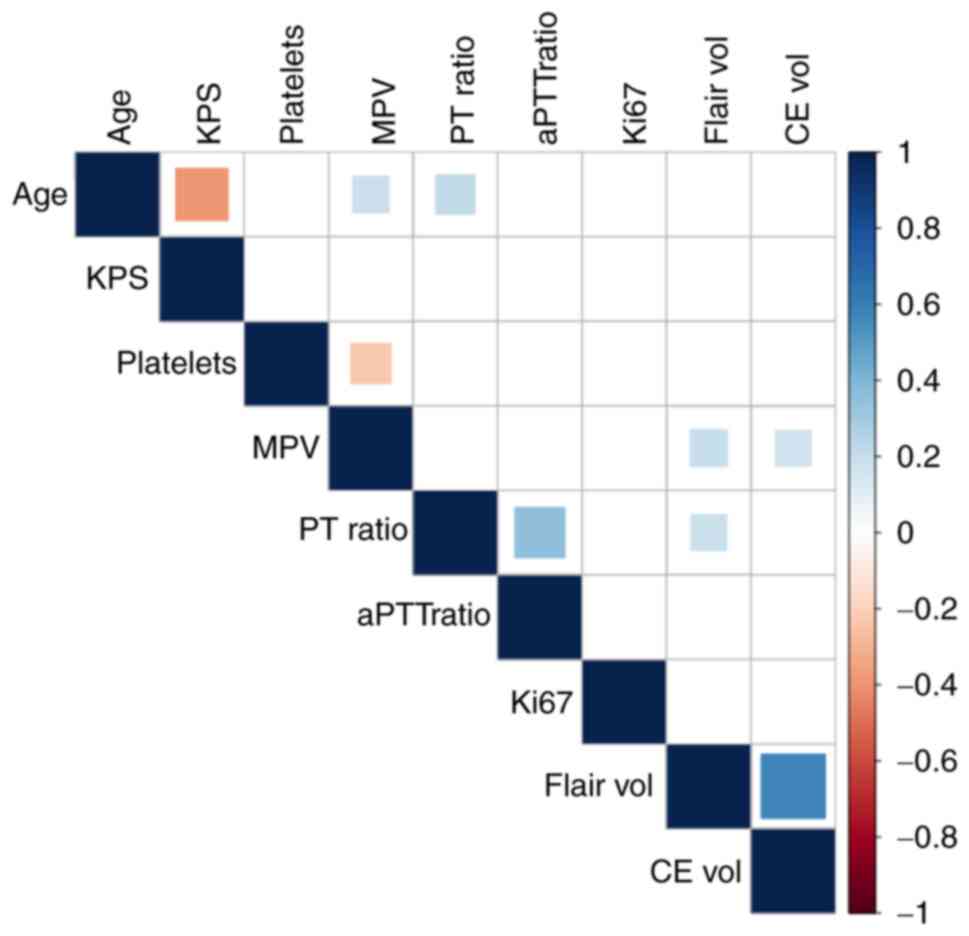
Significant associations were observed between
increasing age and lower KPS (r=−0.38, P<0.001), increased MPV
(r=0.18, P=0.01), and increased PT ratio (r=0.21, P=0.005).
Additionally, MPV values were significantly associated with the
FLAIR (r=0.17, P=0.02) and the T1-CE volumes (r=0.19, P=0.01). A
similar association was observed between the PT ratio and FLAIR
volume (r=0.18, P=0.02). The MPV was also significantly inversely
correlated with PLT (r=−0.22, P=0.003). Correlation analyses
between demographic characteristics, baseline platelet and
coagulation parameters, and tumoral burden were summarized
(Fig. 2).
In terms of post-operative treatments, no
significant associations between MPV values or PLT count and
completion rate of concurrent RT/chemotherapy schedules were
demonstrated (OR 0.84, 95% CI 0.56-1.25, P=0.39; and OR 0.99, 95%
CI 0.99-1.00, P=0.77; respectively). Similarly, the completion of
at least 6 cycles of adjuvant temozolomide (TMZ) was not associated
with baseline MPV (OR 0.88; 95% CI, 0.59-1.32; P=0.55) or PLT count
(OR 1.00; 95% CI, 0.99-1.01; P=0.08). Moreover, no significant
association was observed between the number of adjuvant TMZ cycles
and pre-operative MPV (r=−0.27, P=0.41; OR 0.94, 95% CI 0.61-1.45,
P=0.80) or PLT count (r=−0.001, P=0.81; OR 1.00, 95% CI 0.99-1.00,
P=0.73).
The mortality rate among patients with higher MPV
values was significantly different from that of patients with lower
MPV values (58.1 vs. 41.86%; OR 2.12, 95% CI 1.01-4.45;
P=0.04).
Survival Cox regression analysis
Cox regression between preoperative platelet
parameters and adjuvant chemotherapeutic regimen indicated that all
included parameters retained a significant value in predicting OS.
Specifically, increased MPV had a detrimental effect (HR 1.49; 95%
CI, 1.21-1.83; P<0.001), while in-range-PLT (HR 0.35; 95% CI,
0.21-0.58; P<0.001), concurrent RT/TMZ (HR 0.37; 95% CI,
0.22-0.60; P<0.001) and adjuvant TMZ (HR 0.48; 95% CI,
0.29-0.78; P<0.001) predicted better OS (Table III).
 | Table III.Multivariate Cox regression for MPV
and therapies following surgery. |
Table III.
Multivariate Cox regression for MPV
and therapies following surgery.
|
|
| Multivariate |
|
|---|
|
|
|
|
|
|---|
| Variable | Reference | HR | 95% CI | P-value |
|---|
| MPV
(10−15 l) | NA | 1.49 | 1.21-1.83 | <0.001 |
| PLT central range
(165–300 109/l) | Out of range | 0.35 | 0.21-0.58 | <0.001 |
| Completed
concurrent RT/TMZ | No/interrupted
TMZ | 0.37 | 0.22-0.60 | 0.001 |
| Adjuvant TMZ | No additional
TMZ | 0.48 | 0.29-0.78 | <0.001 |
In addition, multivariate Cox regression analysis of
OS accounting for age, gender, pre-operative performance status,
and tumoral characteristics (R2=0.70, P<0.001)
indicated high MPV as an independent predictive variable for poor
OS (HR 1.56; 95% CI, 1.13-2.16; P=0.006) together with increased
age (HR 1.03; 95% CI, 1.01-1.06; P=0.01). Platelet counts within
the central range were confirmed as predictors of increased OS (HR
0.26; 95% CI, 0.13-0.54; P<0.001), together with complete
surgical resection (HR 0.52; 95% CI, 0.30-0.90; P=0.01), and
completion of post-operative concurrent RT/TMZ (HR 0.24; 95% CI,
0.13-0.45; P<0.001) (Table
IV).
 | Table IV.Multivariate Cox regression analysis
shows an independent prognostic role of age, MPV, and PLT after
controlling for other demographic and lesion parameters, and
adjuvant therapies. |
Table IV.
Multivariate Cox regression analysis
shows an independent prognostic role of age, MPV, and PLT after
controlling for other demographic and lesion parameters, and
adjuvant therapies.
| Variable | Reference | HR | 95% CI | P-value |
|---|
| Age | NA | 1.03 | 1.01-1.06 | 0.01 |
| Female | Male | 0.70 | 0.38-1.26 | 0.24 |
| KPS <80 | ≥80 | 1.21 | 0.72-2.03 | 0.45 |
| Pathology |
|
|
|
|
| MGMT
met | Non met | 0.57 | 0.31-1.05 | 0.07 |
| Ki67
(%) | NA | 3.77 | 0.83-17.1 | 0.08 |
| p53
(%) | NA | 0.83 | 0.30-2.30 | 0.73 |
| Markers |
|
|
|
|
| MPV
(10−15 l) | NA | 1.56 | 1.13-2.16 | 0.006 |
| PT
ratio | NA | 6.02 | 0.70-51.1 | 0.10 |
| aPTT
ratio | NA | 3.24 | 0.11-89.6 | 0.48 |
| PLT
central range (165–300 109/l) | Out of range | 0.26 | 0.13-0.54 | <0.001 |
| Radiology |
|
|
|
|
| FLAIR
volume (cm3) | NA | 1.00 | 0.99-1.01 | 0.74 |
| T1-CE
volume (cm3) | NA | 1.01 | 0.99-1.02 | 0.08 |
|
Satellite FLAIR lesions | No satellite
lesions | 1.23 | 0.58-2.61 | 0.57 |
| Complete
resection | Near
total/subtotal/partial | 0.52 | 0.30-0.90 | 0.01 |
| Completed
concurrent RT/TMZ | No/interrupted
TMZ | 0.24 | 0.13-0.45 | <0.001 |
Discussion
This retrospective study evaluated the association
of baseline peripheral markers of hemostasis and platelet
activation, and relevant oncological outcomes in patients with GBM.
The analysis indicated that higher MPV values were associated with
lower OS and a higher mortality rate compared with patients with
lower MPV levels. Other parameters that demonstrated a negative
association with OS were: PLT count outside the central
distribution and increasing age. Other markers including PT and
aPTT ratio did not demonstrate a strong predictive role in
multivariate analysis, to account for other relevant demographic,
clinical, and molecular variables. It can be hypothesized that the
higher mortality rate observed among the patients with increased
MPV reflected the reduced OS time observed in this cohort. These
findings highlight the need for additional studies to investigate
the role of circulating hemostasis and platelet mediators in the
elucidation of mechanisms of glioblastoma aggressiveness.
Diagnostic and prognostic role of baseline
MPV in other tumors
The concept of platelets being associated with
tumorigenesis and tumor progression has been previously reported,
with growing reports suggesting a diagnostic and prognostic role
for platelet counts and MPV in oncology research (5–16,18).
An increased MPV value represents an index of platelet activation
and has been previously investigated as a diagnostic marker in
solid tumors including breast (11,36–38),
endometrial (39–44), gastric (9,45,46),
colon (47), esophageal (48,49),
and lung cancer (50–52). However, the association between MPV
and the presence of cancer has not always been unequivocal, with
other studies reporting an opposing relationship with decreased MPV
value in patients affected by gastric (53), colon (54), locally advanced esophageal cancer
(55), and renal cell carcinoma
(6). A wide meta-analysis on the
topic conducted in 2016 (56)
concluded that the baseline MPV tends to be higher in oncological
patients when compared with healthy subjects and that its mean
value decreased after treatment, which suggested a proportional
tumoral activation of circulating platelets, in at least some of
the investigated tumors.
The MPV has also been reported as a prognostic
factor for survival in certain types of solid cancers including
esophageal (23), gastric,
pancreatic (24), lung (25), breast, colorectal, head and neck,
hepatic, urothelial cancer, melanoma, osteosarcoma and hematologic
malignancies (23–25), again with equivocal results. In a
large meta-analysis (23) of 38
studies including 9,894 patients with both solid and hematological
tumors, authors reported that pre-treatment MPV value was not
broadly associated with OS, with certain reports suggesting a worse
prognosis in patients with increased MPV (particularly in gastric
and pancreatic cancer), while this effect seemed opposite in lung
cancer (25). In a second review
that investigated the role of MPV (24), it was reported that most studies on
colon carcinoma reported an unfavorable prognostic role for
increased MPV. Based on the results of the present study, it was
hypothesized that these mixed results could be partially explained
by the existence of a different grade of platelet activation as
part of the tumorigenesis process, which is peculiar to each tumor,
and is the result of the unique metabolic and immune interplay that
sustains the cellular growth and invasion. For this reason, markers
of platelet activation may not have a universal role in the
detection and grading of patients' prognosis in patients with
cancer, rather their significance needs to be understood and
validated for each unique type of tumor.
MPV and platelet activation in the
pathophysiology of GBM
The role of platelets in the intricate interplay of
the peritumoral microenvironment is still largely unknown, however
increasing studies have reported their active involvement in
promoting inflammation, immunosuppression, and neo-angiogenesis in
patients with GBM. Platelets can be activated by numerous chemical
or mechanical signals and can potently interact with circulating
leukocytes. Upon activation, platelets express CD40L and P-selectin
which directly recruit circulating leukocytes (20,21)
and further promote white cell extravasation by inducing the
upregulation of endothelial P-selectin, E-selectin, I-CAM1, and
V-CAM1 molecules (19). The role of
platelets in initiating or promoting the immune response is not
limited to leukocyte adhesion and extravasation but is also
intimately related to the active recruitment of specific
subpopulations through the release of the chemokine (C-X-C motif)
ligand (CXCL)1, CXCL4, CXCL5, CXCL7, and CXCL12 chemokines. It has
been previously reported that high levels of TGF-β and CD40L have a
potent immunosuppressive activity by promoting a decrease in
tumor-infiltrating CD8+ T cell levels and a relative
increase of immunosuppressive
CD4+FOXP3+T-regulatory lymphocytes (57) and M2 macrophages (58). Additionally, it is well established
that platelet activation is one of the most potent neo-angiogenesis
events, which is mediated by the release of vascular endothelial
growth factor VEGF and FGF-2 from α granules of activated
platelets, IL-8, IL-10, and prostaglandin E2 (59). This cascade of events has been
observed in glioma models (57)
showing significant platelet activation, soluble CD40 release, and
an increase in immunosuppressive T-reg cells, neo-angiogenesis,
vascular damage, and cellular evasion leading to tumor progression.
In this context, monitoring MPV and PLT count could be used to
estimate the systemic activation of platelets and therefore of
tumor-promoting mechanisms being active in sustaining the survival
and growth of tumoral cells.
Prognostic role of platelet activation in
GBM
Only a few studies (60–62)
have previously specifically addressed the relationship between
platelet activation markers and relevant oncological outcomes in
GBM. Campanella et al (62)
reported that tumoral cells promoted the systemic activation of
platelets and highlighted the key role of VEGF and sphingolipid
signaling pathways in GBM tumorigenesis. More specifically, Wach
et al (60) reported that
patients with a baseline elevated MPV/PLT count ratio before
cranial surgery had significantly shorter progression-free
survival; however, they did not report any effect on OS.
Differently, Alimohammadi et al (61) reported that elevated platelet
distribution width (PDW)/PLT count ratio was an independent
predictor of shortened OS, supporting the relationship between
platelet activity and survival outcome in GBM. PDW reflects
platelet size variations and is also a marker of platelet
activation (63). A recent large
retrospective analysis (64)
concluded that no baseline blood tests could be reliably used as
prognostic indicators in GBM. However, although the previous study
was notable for the quality and large sample size, it should be
noted that candidates for both biopsy and surgical resection, IDH
mutated and wildtype tumors, were included. Furthermore only PLT
count, aPTT and PT values were considered and MPV was not.
Therefore, the heterogeneity in patient selection could have masked
the prognostic role of PLT counts and coagulation markers on
relevant oncological outcomes. The present study however, showed a
relationship between MPV and OS in a homogeneous population of
patients with IDH-wt GBM lesions undergoing craniotomy for maximal
safe resection, which may represent a smaller, yet neuro-surgically
relevant subgroup of patients with GBM, than those considered by
Maas et al (64).
In accordance with the report of Wach et al
(60), who reported increased MPV
and lower PLT count in GBM models as the result of excessive
systemic platelet activation and consumption, the present study
found an inverse correlation between MPV values and PLT count in
the patient cohort. A positive correlation of MPV values with
increasing age and the overall tumoral volume was also observed. To
investigate the role of aging in this physio-pathological
mechanism, a subgroup analysis of patients aged >65 years was
performed which confirmed that in this subpopulation the MPV value
showed an even stronger predictive role of decreased survival in
these patients. This latter phenomenon could be explained by a
relatively different biology of GBM in elderly patients (65), as reported by Bozdag et al
(66), who reported age-specific
increased hypermethylation in polycomb group protein target genes
and the upregulation of angiogenesis-related genes which could be
associated with stronger systemic platelet activation in this
subgroup of patients. At the same time, the contribution of the PLT
count, PT, and aPTT were smaller than that which was observed in
the younger population. These older patients did not differ from
the young cohort for other baseline characteristics besides a worse
performance status, which did not directly correlate with the MPV
values in the analysis performed.
The positive correlation between tumor volumes and
MPV values supports further future evaluation, as the extent of
platelet activation could be associated with the lesion burden and
relative aggressiveness.
The multivariate Cox regression model was used to
help differentiate the single contributions to the overall OS
length loss and indicated that increasing age, increasing MPV and
deranged PLT count are independent predictors of worse OS in the
patient cohort of the present study. However, the KPS, gender, and
MGMT mutation status did not indicate a significant prognostic role
in this cohort. Although the KPS is a well-known prognostic factor
in GBM (67), in the present study
only patients eligible for major surgery were included, ruling out
those in extremely poor general conditions; therefore, the impact
of KPS on OS could have been partially mitigated by patient
selection. The MGMT methylation status was not determined in all
included patients, of those for whom this was assessed, 37%
presented MGMT methylation. This could suggest that the higher
relative incidence of MGMT-unmethylated lesions could have reduced
the survival benefit that would be expected from the surgery and
adjuvant treatments in this patient cohort. Similarly, the female
gender has been reported to be associated with better overall
survival (68). In the present
study, however, this relationship was only found in the subgroup of
female patients with MGMT promoter methylation. These results
indicate the importance of further investigations; however, this
does not obscure the relevance of the role of MPV and PLT count in
OS in patients with GBM. Overall, the results of the present study
support the idea that systemic hemostasis and platelet activation
might contribute to tumor aggressiveness, as indicated by the
significant association between tumoral volumes, MPV, PLT count,
and survival. To the best of our knowledge, no previous studies
have reported an association between hemostasis markers and
prognosis in a homogeneous population for both treatment and
histology. Additional studies are required to elucidate the
interplay between tumoral activity and platelet activation.
The principal limitations of the present study are
the monocentric, retrospective design, the relatively small number
of included patients, and the lack of thorough molecular analysis,
such as full MGMT methylation profile and, TERT and EGFR mutation
assessment. Data were retrospectively retrieved from the medical
records of included patients and no control group was available.
Additionally, this study lacks cross-sectional time research.
Results from this study suggest that, despite the
intrinsic inter-individual and time-dependent variability of blood
markers, PLT count and MPV could reveal the role of systemic
hemostasis and platelet activation in promoting a pro-tumoral
microenvironment in patients with GBM. These findings require
additional studies to further validate this hypothesis and
specifically characterize for GBM the pathological features of
aggressiveness related to hemostasis activation, neo-angiogenesis,
and the tumor immune microenvironment, and their impact on response
to therapies and OS.
Supplementary Material
Supporting Data
Acknowledgments
Not applicable.
Funding
The present study was supported by the non-profit association
‘Amici di Tosco’ (Merate, Italy; association no. 94038420132).
Availability of data and materials
The data generated in the present study may be
requested from the corresponding author.
Authors' contributions
SS, PDD, FR, AB, MB, AG, LRB, CM, PM, and FG
contributed to the study's conception and design. Material
preparation, data collection strategy, and analysis were performed
by PDD, SS, and FG. Retrospective data collection was conducted by
AB, MB, and CM. The first draft of the manuscript was written by SS
and PDD. SS and FG confirm the authenticity of all the raw data.
All authors read and approved the final manuscript.
Ethics approval and consent to
participate
This study was performed in line with the principles
of the Declaration of Helsinki. Data were collected after approval
from the Internal Ethics Committee of IRCCS San Raffaele Hospital
granted on 13th July 2022 (protocol ID, NCH 02-2022; approval no.
82/INT/2022). At hospital admission, each patient signed written
consent for the treatment and collection and analysis of personal
data and specimens.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
Authors' information
Dr Pierfrancesco De Domenico - ORCID:
0000-0003-3330-162X.
References
|
1
|
Koshy M, Villano JL, Dolecek TA, Howard A,
Mahmood U, Chmura SJ, Weichselbaum RR and McCarthy BJ: Improved
survival time trends for glioblastoma using the SEER 17
population-based registries. J Neurooncol. 107:207–212. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Fabbro-Peray P, Zouaoui S, Darlix A,
Fabbro M, Pallud J, Rigau V, Mathieu-Daude H, Bessaoud F, Bauchet
F, Riondel A, et al: Association of patterns of care, prognostic
factors, and use of radiotherapy-temozolomide therapy with survival
in patients with newly diagnosed glioblastoma: A French national
population-based study. J Neurooncol. 142:91–101. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Stupp R, Mason WP, van den Bent MJ, Weller
M, Fisher B, Taphoorn MJ, Belanger K, Brandes AA, Marosi C, Bogdahn
U, et al: Radiotherapy plus concomitant and adjuvant temozolomide
for glioblastoma. N Engl J Med. 352:987–996. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Louis DN, Perry A, Wesseling P, Brat DJ,
Cree IA, Figarella-Branger D, Hawkins C, Ng HK, Pfister SM,
Reifenberger G, et al: The 2021 WHO classification of tumors of the
central nervous system: A summary. Neuro Oncol. 23:1231–1251. 2021.
View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Seles M, Posch F, Pichler GP, Gary T,
Pummer K, Zigeuner R, Hutterer GC and Pichler M: Blood platelet
volume represents a novel prognostic factor in patients with
nonmetastatic renal cell carcinoma and improves the predictive
ability of established prognostic scores. J Urol. 198:1247–1252.
2017. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Yun ZY, Zhang X, Liu YS, Liu T, Liu ZP,
Wang RT and Yu KJ: Lower mean platelet volume predicts poor
prognosis in renal cell carcinoma. Sci Rep. 7:67002017. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Tuncel T, Ozgun A, Emirzeoglu L, Celik S,
Bilgi O and Karagoz B: Mean platelet volume as a prognostic marker
in metastatic colorectal cancer patients treated with
bevacizumab-combined chemotherapy. Asian Pac J Cancer Prev.
15:6421–6423. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Kumagai S, Tokuno J, Ueda Y, Marumo S,
Shoji T, Nishimura T, Fukui M and Huang CL: Prognostic significance
of preoperative mean platelet volume in resected non-small-cell
lung cancer. Mol Clin Oncol. 3:197–201. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Kilincalp S, Ekiz F, Başar O, Ayte MR,
Coban S, Yılmaz B, Altınbaş A, Başar N, Aktaş B, Tuna Y, et al:
Mean platelet volume could be possible biomarker in early diagnosis
and monitoring of gastric cancer. Platelets. 25:592–594. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Zhang F, Chen Z, Wang P, Hu X, Gao Y and
He J: Combination of platelet count and mean platelet volume
(COP-MPV) predicts postoperative prognosis in both resectable early
and advanced stage esophageal squamous cell cancer patients. Tumour
Biol. 37:9323–3931. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Gu M, Zhai Z, Huang L, Zheng W, Zhou Y,
Zhu R, Shen F and Yuan C: Pre-treatment mean platelet volume
associates with worse clinicopathologic features and prognosis of
patients with invasive breast cancer. Breast Cancer. 23:752–760.
2016. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Cho SY, Yang JJ, You E, Kim BH, Shim J,
Lee HJ, Lee WI, Suh JT and Park TS: Mean platelet volume/platelet
count ratio in hepatocellular carcinoma. Platelets. 24:375–377.
2013. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Inagaki N, Kibata K, Tamaki T, Shimizu T
and Nomura S: Prognostic impact of the mean platelet
volume/platelet count ratio in terms of survival in advanced
non-small cell lung cancer. Lung Cancer. 83:97–101. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Zhang X, Qin YY, Chen M, Wu YY and Lin FQ:
Combined use of mean platelet volume/platelet count ratio and
platelet distribution width to distinguish between patients with
nasopharyngeal carcinoma, those with benign tumors of the
nasopharynx, and healthy subjects. Cancer Manag Res.
11:10375–10382. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Feng JF, Sheng C, Zhao Q and Chen P:
Prognostic value of mean platelet volume/platelet count ratio in
patients with resectable esophageal squamous cell carcinoma: A
retrospective study. PeerJ. 7:e72462019. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Lin YC, Jan HC, Ou HY, Ou CH and Hu CY:
low preoperative mean platelet volume/platelet count ratio
indicates worse prognosis in non-metastatic renal cell carcinoma. J
Clin Med. 10:36762021. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Giannakeas V, Kotsopoulos J, Brooks JD,
Cheung MC, Rosella L, Lipscombe L, Akbari MR, Austin PC and Narod
SA: Platelet count and survival after cancer. Cancers (Basel).
14:5492022. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Giannakeas V, Kotsopoulos J, Cheung MC,
Rosella L, Brooks JD, Lipscombe L, Akbari MR, Austin PC and Narod
SA: Analysis of platelet count and new cancer diagnosis over a
10-year period. JAMA Netw Open. 5:e21416332022. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Olsson AK and Cedervall J: The
pro-inflammatory role of platelets in cancer. Platelets.
29:569–573. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Lievens D, Zernecke A, Seijkens T,
Soehnlein O, Beckers L, Munnix IC, Wijnands E, Goossens P, van
Kruchten R, Thevissen L, et al: Platelet CD40L mediates thrombotic
and inflammatory processes in atherosclerosis. Blood.
116:4317–4327. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Thomas MR and Storey RF: The role of
platelets in inflammation. Thromb Haemost. 114:449–458. 2015.
View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Thompson CB, Eaton KA, Princiotta SM,
Rushin CA and Valeri CR: Size dependent platelet subpopulations:
Relationship of platelet volume to ultrastructure, enzymatic
activity, and function. Br J Haematol. 50:509–519. 1982. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Chen X, Li J, Zhang X, Liu Y, Wu J, Li Y,
Cui X and Jiang X: Prognostic and clinicopathological significance
of pretreatment mean platelet volume in cancer: A meta-analysis.
BMJ Open. 10:e0376142020. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Detopoulou P, Panoutsopoulos GI, Mantoglou
M, Michailidis P, Pantazi I, Papadopoulos S and Rojas Gil AP:
Relation of mean platelet volume (MPV) with Cancer: A systematic
review with a focus on disease outcome on twelve types of cancer.
Curr Oncol. 30:3391–3420. 2023. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Kharel S, Shrestha S, Shakya P, Rawat R
and Shilpakar R: Prognostic significance of mean platelet volume in
patients with lung cancer: A meta-analysis. J Int Med Res.
50:30006052210848742022. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Louis DN, Perry A, Reifenberger G, von
Deimling A, Figarella-Branger D, Cavenee WK, Ohgaki H, Wiestler OD,
Kleihues P and Ellison DW: The 2016 World Health Organization
Classification of Tumors of the Central Nervous System: A summary.
Acta Neuropathol. 131:803–820. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Nobusawa S, Watanabe T, Kleihues P and
Ohgaki H: IDH1 mutations as molecular signature and predictive
factor of secondary glioblastomas. Clin Cancer Res. 15:6002–6007.
2009. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Karschnia P, Young JS, Dono A, Häni L,
Sciortino T, Bruno F, Juenger ST, Teske N, Morshed RA, Haddad AF,
et al: Prognostic validation of a new classification system for
extent of resection in glioblastoma: A report of the RANO resect
group. Neuro Oncol. 25:940–954. 2023. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Mor V, Laliberte L, Morris JN and Wiemann
M: The karnofsky performance status scale. An examination of its
reliability and validity in a research setting. Cancer.
53:2002–2007. 1984. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
R Core Team, . R: A language and
environment for statistical computing. R Foundation for Statistical
Computing; Vienna, Austria: 2022, Available from:. https://www.R-project.org/
|
|
31
|
Therneau TM: A Package for Survival
Analysis in R. R package. Version 3.5-5, 2023. Available from.
https://CRAN.R-project.org/package=survival
|
|
32
|
Sjoberg DD, Baillie M, Fruenchtenicht C,
Haesendonckx S and Treis T: Flexible Time-to-Event Figures. R
package. Version 1.0.0. 2023.Available from:. https://CRAN.R-project.org/package=ggsurvfit
|
|
33
|
Wei T and Simko V: R package ‘corrplot’:
Visualization of a Correlation Matrix. Version 0.92. 2021.Available
from:. https://github.com/taiyun/corrplot
|
|
34
|
Wickham H: ggplot2: Elegant Graphics for
Data Analysis. Springer-Verlag New York. Version 1.0.2016.Available
from:. https://ggplot2.tidyverse.org
|
|
35
|
Sheng J, Qiu P and Geyer CJ: TSHRC: Two
Stage Hazard Rate Comparison. Version 0.1-6. 2019.Available from:.
https://CRAN.R-project.org/package=TSHRC
|
|
36
|
Tanriverdi O, Menekse S, Teker F, Oktay E,
Nur Pilanc K, Gunaldi M, Kocar M, Kacan T, Bahceci A, Avci N, et
al: The mean platelet volume may predict the development of
isolated bone metastases in patients with breast cancer: A
retrospective study of the Young Researchers Committee of the
Turkish Oncology Group (TOG). J BUON. 21:840–850. 2016.PubMed/NCBI
|
|
37
|
Sun H, Yin CQ, Liu Q, Wang F and Yuan CH:
Clinical signi fi cance of routine blood test-associated
inflammatory index in breast cancer patients. Med Sci Monit.
23:5090–5095. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
38
|
Divsalar B, Heydari P, Habibollah G and
Tamaddon G: Hematological parameters changes in patients with
breast cancer. Clin Lab. 67:2021. View Article : Google Scholar : PubMed/NCBI
|
|
39
|
Kurtoglu E, Kokcu A, Celik H, Sari S and
Tosun M: Platelet indices may be useful in discrimination of benign
and malign endometrial lesions, and early and advanced stage
endometrial cancer. Asian Pac J Cancer Prev. 16:5397–5400. 2015.
View Article : Google Scholar : PubMed/NCBI
|
|
40
|
Zhang H, Liang K, Ke L and Tang S:
Clinical application of red cell distribution width, mean platelet
volume, and cancer antigen 125 detection in endometrial cancer. J
Clin Lab Anal. 34:e233092020. View Article : Google Scholar : PubMed/NCBI
|
|
41
|
Karateke A, Kaplanoglu M and Baloglu A:
Relations of platelet indices with endometrial hyperplasia and
endometrial cancer. Asian Pac J Cancer Prev. 16:4905–4908. 2015.
View Article : Google Scholar : PubMed/NCBI
|
|
42
|
Oge T, Yalcin OT, Ozalp SS and Isikci T:
Platelet volume as a parameter for platelet activation in patients
with endometrial cancer. J Obstet Gynaecol. 33:301–304. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
43
|
Song J, Lai X, Zhang Y, Zheng X and Su J:
Preoperative platelet morphology parameters as prognostic
predictors for endometrial malignant carcinoma stage and
progesterone receptor. Medicine (Baltimore). 98:e178182019.
View Article : Google Scholar : PubMed/NCBI
|
|
44
|
Yayla Abide C, Bostanci Ergen E, Cogendez
E, Kilicci C, Uzun F, Ozkaya E and Karateke A: Evaluation of
complete blood count parameters to predict endometrial cancer. J
Clin Lab Anal. 32:e224382018. View Article : Google Scholar : PubMed/NCBI
|
|
45
|
Shen XM, Xia YY, Lian L, Zhou C, Li XL,
Han SG, Zheng Y, Gong FR, Tao M, Mao ZQ and Li W: Mean platelet
volume provides beneficial diagnostic and prognostic information
for patients with resectable gastric cancer. Oncol Lett.
12:2501–2506. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
46
|
Pietrzyk L, Plewa Z, Denisow-Pietrzyk M,
Zebrowski R and Torres K: Diagnostic power of blood parameters as
screening markers in gastric cancer patients. Asian Pac J Cancer
Prev. 17:4433–4437. 2016.PubMed/NCBI
|
|
47
|
Li JY, Li Y, Jiang Z, Wang RT and Wang XS:
Elevated mean platelet volume is associated with presence of colon
cancer. Asian Pac J Cancer Prev. 15:10501–10504. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
48
|
Zhou X, Chen H, Zhang W, Li X, Si X and
Zhang G: Predictive value of routine blood test in patients with
early esophageal cancer: A matched case-control study. J Cancer.
12:4739–4744. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
49
|
Surucu E, Demir Y and Sengoz T: The
correlation between the metabolic tumor volume and hematological
parameters in patients with esophageal cancer. Ann Nucl Med.
29:906–910. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
50
|
Zhu X, Chen Y and Cui Y: Absolute
neutrophil count and mean platelet volume in the blood as
biomarkers to detect lung cancer. Dis Markers. 2020:13719642020.
View Article : Google Scholar : PubMed/NCBI
|
|
51
|
Zu R, Yu S, Yang G, Ge Y, Wang D, Zhang L,
Song X, Deng Y, He Q, Zhang K, et al: Integration of platelet
features in blood and platelet rich plasma for detection of lung
cancer. Clin Chim Acta. 509:43–51. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
52
|
Goksel S, Ozcelik N, Telatar G and Ardic
C: The role of hematological inflammatory biomarkers in the
diagnosis of lung cancer and in predicting TNM Stage. Cancer
Invest. 39:514–520. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
53
|
Aksoy EK, Kantarcı S, Torgutalp M, Akpınar
MY, Sapmaz FP, Yalçın GŞ, Uzman M, Şimşek GG and Nazlıgül Y: The
importance of complete blood count parameters in the screening of
gastric cancer. Prz Gastroenterol. 14:183–187. 2019.PubMed/NCBI
|
|
54
|
Huang L, Hu Z, Luo R, Li H, Yang Z, Qin X
and Mo Z: Predictive values of the selected inflammatory indexes in
colon cancer. Cancer Control. 29:107327482210913332022. View Article : Google Scholar : PubMed/NCBI
|
|
55
|
Sun SY, Zhao BQ, Wang J, Mo ZX, Zhao YN,
Wang Y and He J: The clinical implications of mean platelet volume
and mean platelet volume/platelet count ratio in locally advanced
esophageal squamous cell carcinoma. Dis Esophagus. 31:2018.
View Article : Google Scholar
|
|
56
|
Pyo JS, Sohn JH and Kang G: Diagnostic and
prognostic roles of the mean platelet volume in malignant tumors: A
systematic review and meta-analysis. Platelets. 27:722–728. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
57
|
Panek WK, Pituch KC, Miska J, Kim JW,
Rashidi A, Kanojia D, Lopez-Rosas A, Han Y, Yu D, Chang CL, et al:
Local application of autologous platelet-rich fibrin Patch (PRF-P)
suppresses regulatory T cell recruitment in a murine glioma model.
Mol Neurobiol. 56:5032–5040. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
58
|
Neuzillet C, Tijeras-Raballand A, Cohen R,
Cros J, Faivre S, Raymond E and de Gramont A: Targeting the TGFβ
pathway for cancer therapy. Pharmacol Ther. 147:22–31. 2015.
View Article : Google Scholar : PubMed/NCBI
|
|
59
|
Filippelli A, Del Gaudio C, Simonis V,
Ciccone V, Spini A and Donnini S: Scoping review on platelets and
tumor angiogenesis: Do we need more evidence or better analysis?
Int J Mol Sci. 23:134012022. View Article : Google Scholar : PubMed/NCBI
|
|
60
|
Wach J, Apallas S, Schneider M, Weller J,
Schuss P, Vatter H, Herrlinger U and Güresir E: Mean platelet
volume/platelet count ratio and risk of progression in
glioblastoma. Front Oncol. 11:6953162021. View Article : Google Scholar : PubMed/NCBI
|
|
61
|
Alimohammadi E, Bagheri SR, Bostani A,
Rezaie Z and Farid M: Preoperative platelet distribution
width-to-platelet count ratio as a prognostic factor in patients
with glioblastoma multiforme. Br J Neurosurg. 38:307–313. 2024.
View Article : Google Scholar : PubMed/NCBI
|
|
62
|
Campanella R, Guarnaccia L, Cordiglieri C,
Trombetta E, Caroli M, Carrabba G, La Verde N, Rampini P, Gaudino
C, Costa A, et al: Tumor-Educated platelets and angiogenesis in
glioblastoma: Another brick in the wall for novel prognostic and
targetable biomarkers, changing the vision from a localized tumor
to a systemic pathology. Cells. 9:2942020. View Article : Google Scholar : PubMed/NCBI
|
|
63
|
Huang K, Wei S, Huang Z, Xie Y, Wei C, Xu
J, Dong L, Zou Q and Yang J: Effect of preoperative peripheral
blood platelet volume index on prognosis in patients with invasive
breast cancer. Future Oncol. 19:1853–186. 2023. View Article : Google Scholar : PubMed/NCBI
|
|
64
|
Maas SLN, Draaisma K, Snijders TJ, Senders
JT, Berendsen S, Seute T, Schiffelers RM, van Solinge WW, Ten Berg
MJ, Robe PA and Broekman MLD: Routine blood tests do not predict
survival in patients with glioblastoma-multivariable analysis of
497 patients. World Neurosurg. 126:e1081–e1091. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
65
|
Bruno F, Pellerino A, Palmiero R, Bertero
L, Mantovani C, Garbossa D, Soffietti R and Rudà R: Glioblastoma in
the Elderly: Review of molecular and therapeutic aspects.
Biomedicines. 10:6442022. View Article : Google Scholar : PubMed/NCBI
|
|
66
|
Bozdag S, Li A, Riddick G, Kotliarov Y,
Baysan M, Iwamoto FM, Cam MC, Kotliarova S and Fine HA:
Age-specific signatures of glioblastoma at the genomic, genetic,
and epigenetic levels. PLoS One. 8:e629822013. View Article : Google Scholar : PubMed/NCBI
|
|
67
|
Zhang K, Wang XQ, Zhou B and Zhang L: The
prognostic value of MGMT promoter methylation in Glioblastoma
multiforme: A meta-analysis. Fam Cancer. 12:449–458. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
68
|
Tian M, Ma W, Chen Y, Yu Y, Zhu D, Shi J
and Zhang Y: Impact of gender on the survival of patients with
glioblastoma. Biosci Rep. 38:BSR201807522018. View Article : Google Scholar : PubMed/NCBI
|