Introduction
Pyothorax-associated lymphoma (PAL) is a unique and
rare disease involving malignant lymphoma. PAL appears in the
pleural cavity with chronic pyothorax (CP) following artificial
collapse therapy for pulmonary tuberculosis (1,2).
Lymphoma comprises Hodgkin's and non-Hodgkin's types. PAL is a
non-Hodgkin's lymphoma developing in the pleural cavity after a
long-standing history of CP, and is strongly associated with
Epstein-Barr virus (EBV) infection (3). It has been reported that approximately
90% of the cases are diffuse large B cell lymphoma and that the
5-year survival rate is approximately 20% (1). It is crucial to evaluate the area of
invasion in PAL, which may determine the appropriate treatment,
such as surgery, chemotherapy, irradiation and best supportive
care. However, conventional imaging modalities cannot provide
sufficient information for an accurate diagnosis of PAL (4).
The development of the new modality of F-18
2′-deoxy-2fluoro-D-glucose (FDG) positron emission tomography
combined with computed tomography (PET/CT) has contributed to the
evaluation of human cancer. Additionally, the usefulness of
FDG-PET/CT for lymphoma staging is well established (5,6).
However, few studies exist describing FDG-PET/CT findings in PAL
(7). This study reported three
patients with PAL, who had previously undergone artificial collapse
therapy for pulmonary tuberculosis. The first two cases involved
initial occurrences, and the last case showed recurrent disease
following right pleuropneumonectomy for PAL. FDG-PET/CT imaging
revealed a unique intense uptake of FDG in the area of CP and in
the lymphatic and systemic metastatic lesions. Therefore, the
usefulness of FDG-PET/CT imaging to evaluate the area of invasion
in PAL was examined.
Patients and methods
This study was performed with informed consent of
the patients and with approval of the Ethics Committee of the
Tokorozawa PET Diagnostic Imaging Clinic.
Case 1
An 84-year-old male complaining of abdominal pain
consulted the M Clinic in Tokyo. An ultrasound study revealed a
mass shadow in the left chest wall without abnormal findings in the
abdomen. CT and magnetic resonance imaging scans suggested
malignant lymphoma of the chest. A physical examination showed no
apparently abnormal findings or signs of systemic lymphadenopathy
other than a mass in the left chest wall. Blood analysis showed an
elevated serum interleukin-2 receptor (IL-2R, 1,560 Ug/ml) without
other abnormalities, including tumor markers such as
carcinoembryonic antigen (CEA) and CA19-9. The patient had
previously undergone left artificial collapse therapy for pulmonary
tuberculosis at the age of 20.
18F-FDG PET/CT scans were obtained using
a Biograph Duo (Siemens CTI) at the Tokorozawa PET Diagnostic
Imaging Clinic, as described in our previous study (8,9). To
determine semi-quantitative FDG uptake, regions of interest (ROIs)
were placed over the lesion, including the highest uptake area
(circular ROI, 1 cm in diameter), and the standardized uptake value
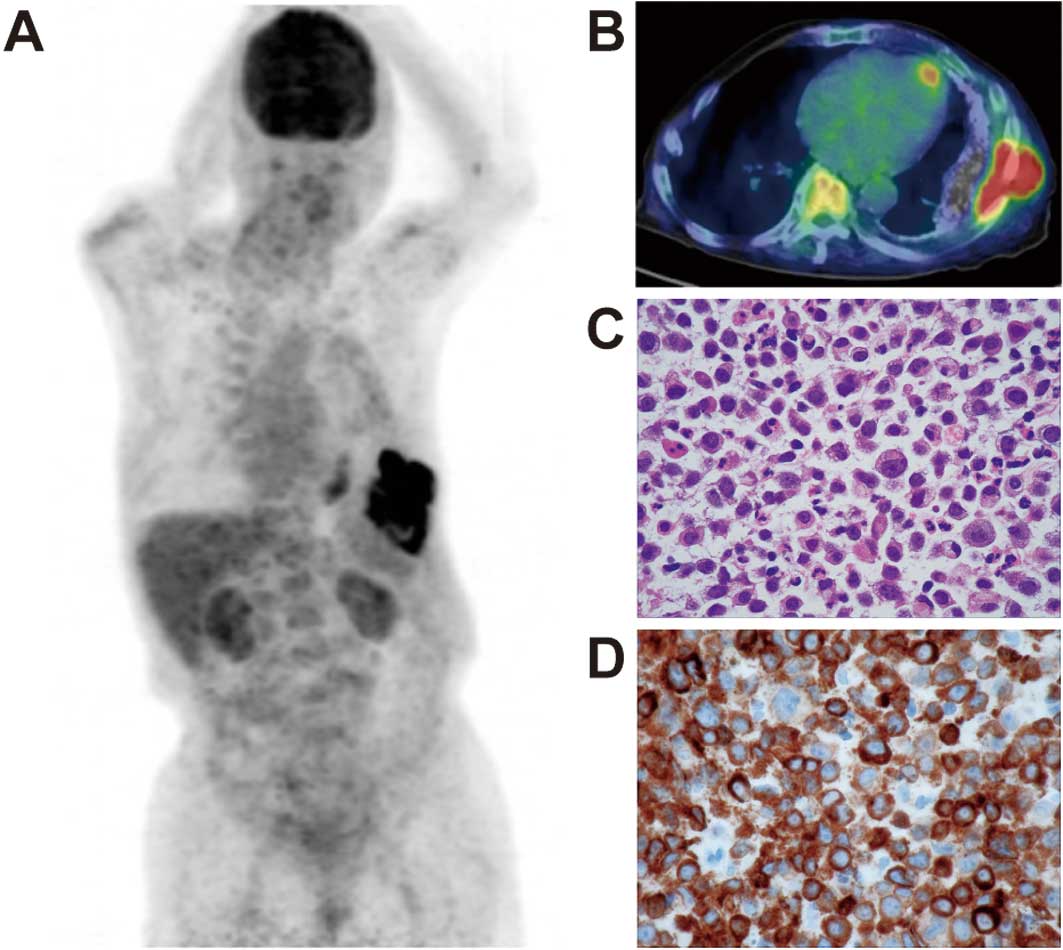
(SUV) was calculated. Early PET/CT showed intense abnormal FDG
uptake only in the left pleura and chest wall, suggesting CP
(SUVmax, 14.8) (Fig. 1A and B). A
delayed scan showed a more intense FDG uptake (SUVmax, 19.4) in CP.
No areas, other than CP, showed an abnormal uptake of FDG. The
PET/CT findings strongly suggested malignancy of the chest wall
without lymphatic or systemic metastasis.
Histopathological examination was performed, and the
biopsy specimens were obtained from the PET/CT-positive pleura. A
microscopic examination showed a diffuse infiltrative growth of the
large atypical lymphoid cells (Fig.
1C). The lymphoid cells contained irregular nuclei.
Immunohistochemical analysis showed that the neoplastic cells were
positive for LCA (CD45RO), CD79a (Fig.
1D), CD20 and BCL-2. The neoplastic cells were also positive
for LMP-1, suggesting EBV infection. Histopathological examination
confirmed the diagnosis as non-Hodgkin's, diffuse large B cell
lymphoma. Due to poor general condition, the patient received best
supportive care without chemotherapy or surgery despite the
localized lesion of PAL.
Case 2
An 83-year-old male complaining of abdominal pain
presented at the Tokorozawa Clinic in Saitama. An ultrasound study
revealed a mass shadow in the left chest wall without abnormal
findings in the abdomen. A physical examination showed no
apparently abnormal findings or signs of systemic lymphadenopathy
other than the mass of the left chest wall. Blood analysis showed
elevation of the serum IL-2R (634 Ug/ml) and neuron-specific
enolase (58 ng/ml). The patient had previously undergone left
artificial collapse therapy for pulmonary tuberculosis at the age
of 24.
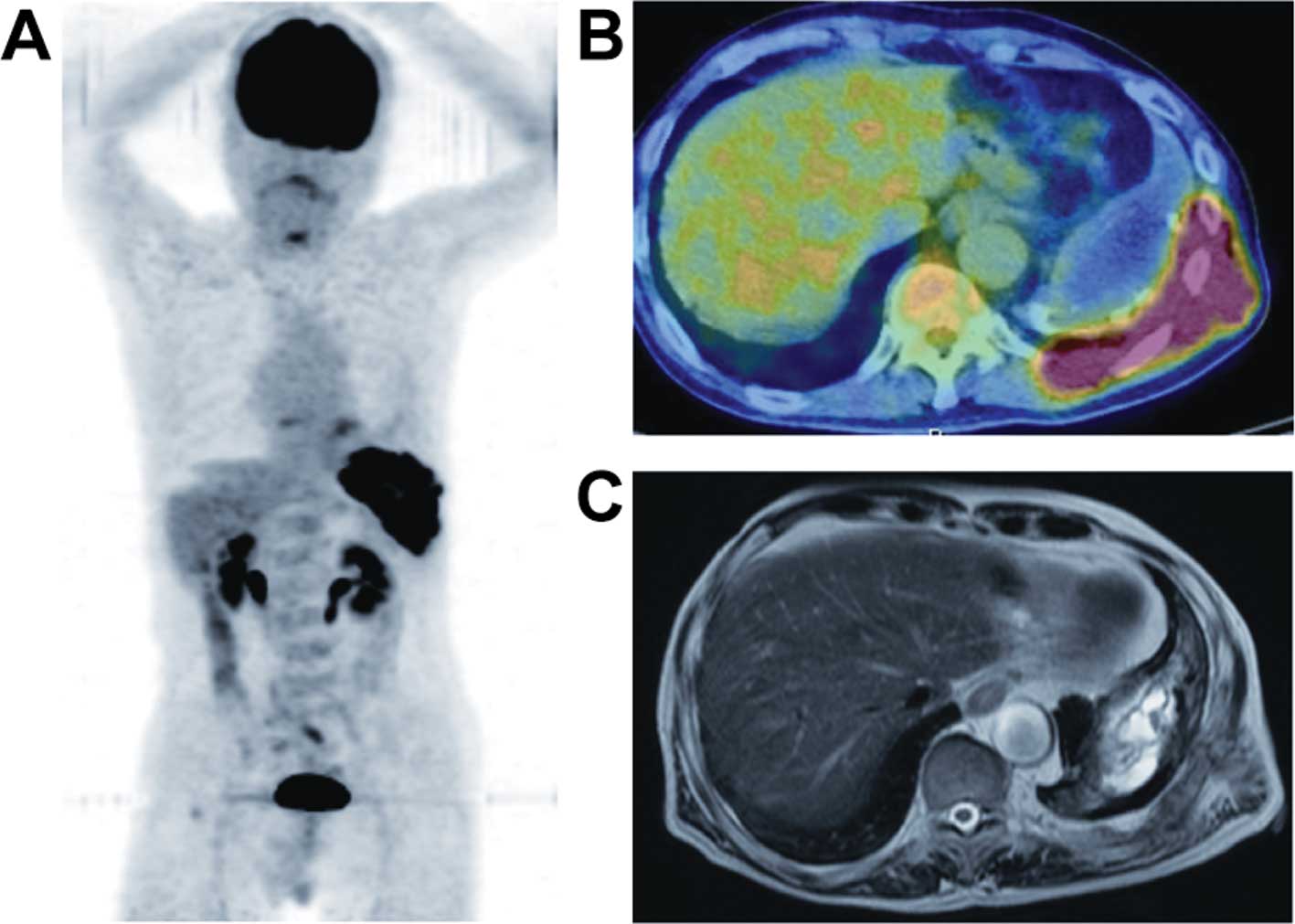
18F-FDG PET/CT scans were obtained in our
PET clinic. Early PET/CT showed intense abnormal FDG uptake only in
the left pleura and chest wall, suggesting CP (SUVmax, 20.8)
(Fig. 2A and B). A delayed scan
showed a more intense FDG uptake (SUVmax, 27.3) in the CP. No
areas, other than CP, revealed an abnormal FDG uptake. The PET/CT
findings strongly suggested malignancy of the chest wall without
lymphatic or systemic metastasis. An MRI scan showed high
signal-intensity on T2-weighted images in the left chest,
suggesting CP, as well as moderate signal-intensity around the CP,
which was consistent with malignant lymphoma (Fig. 2C).
Histopathological examination was performed on
biopsy specimens obtained from the PET/CT-positive pleura. This
examination confirmed the diagnosis as non-Hodgkin's, diffuse large
B cell lymphoma. The patient received chemotherapy (R-CHOP:
rituximab, cyclophosphamide, doxorubicin, vincristine and
prednisone) despite the localized lesion of PAL, following the
patient's request for non-surgical treatment.
Case 3
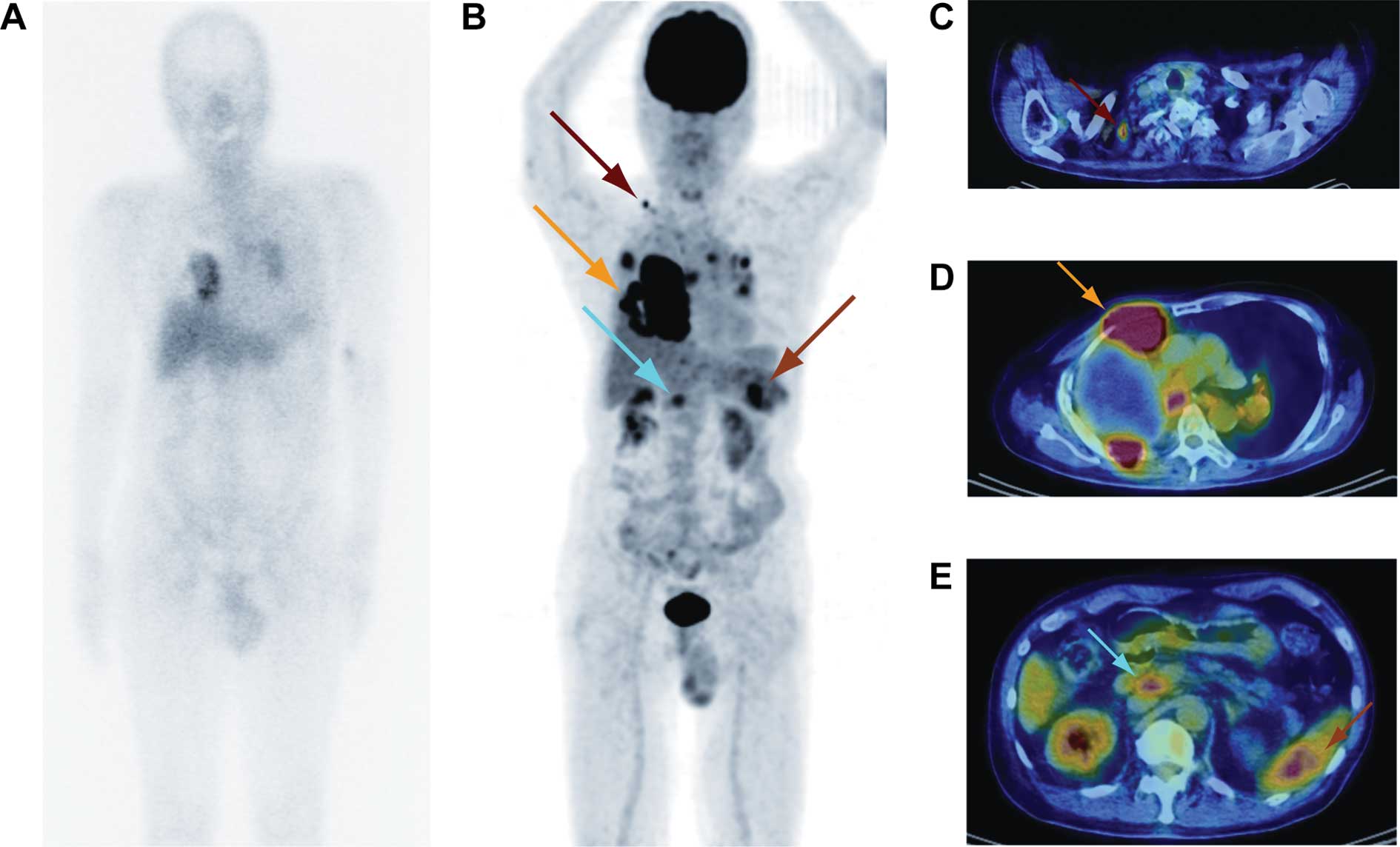
A 79-year-old male complaining of chest pain
presented at the Kyosai Tachikawa Hospital in Tokyo. He had
previously undergone right artificial collapse therapy for
pulmonary tuberculosis at the age of 24. Fifty years later, he was
diagnosed with PAL, diffuse large B cell lymphoma and was treated
with right pleuropneumonectomy. At the present examination, a blood
analysis showed elevation of the serum IL-2 receptor (2,360 U/ml),
suggesting a relapse of PAL. Gallium-67 (67Ga)
scintigraphy showed a faint level of abnormal uptake in the chest
(Fig. 3A). Histopathological
examination of specimens obtained from the pleural mass showed
diffuse large B cell lymphoma, and the patient was diagnosed as
having a recurrence of PAL.
Early 18F-FDG PET/CT showed intense
abnormal FDG uptake in the right pleura and chest wall, suggesting
CP (SUVmax, 19.9) (Fig. 3B-E).
Abnormal intense FDG uptake was also noted in the hilar,
mediastinal, supraclavicular and abdominal lymph nodes, as well as
in the spleen. A delayed scan showed a more intense FDG uptake
(SUVmax, 35.7) in the CP. The patient received chemotherapy
(R-CHOP) numerous times, but finally refused to receive further
chemotherapy.
Discussion
PAL is a non-Hodgkin's lymphoma that develops in the
pleural cavity following a long-standing history of CP. It is known
that approximately 90% of PAL cases involve diffuse large B cell
lymphoma, and that the 5-year survival rate is approximately 20%
(1). Standard treatment for PAL has
yet to be established, although the prognosis is poor. Certain
studies have described PAL cases in which surgery was performed
(10,11). It is essential that the area of
invasion in PAL be evaluated, since it may determine the
appropriate choice of therapy, including surgery, chemotherapy,
irradiation and best supportive care. However, conventional imaging
modalities cannot provide sufficient information for the accurate
diagnosis of PAL (4).
The development of FDG-PET/CT contributes to the
evaluation of human cancer staging. Moreover, the usefulness of
PET/CT is well established for lymphoma staging (5,6).
However, only one study on PET findings in PAL has been published,
by Asakura et al (7). These
authors reported a PAL case in which the FDG-PET finding determined
the area of PAL invasion and provided useful information for the
planning of radiotherapy. We presented three cases of PAL, two of
which showed initial occurrence and one recurrent case. The PET/CT
scan showed intense FDG uptake only in the chest wall in the two
cases showing initial occurrence of PAL. In these cases, the area
of invasion determined by the PET/CT scan contributed to decisions
regarding PAL treatment.
In the recurrent case of PAL, the PET/CT scan showed
intense FDG uptake, not only in the chest wall, but also in the
lymphatic and systemic metastatic lesions. On the other hand,
67Ga scintigraphy showed a faint level of abnormal
uptake only in the chest. Certain studies have shown the usefulness
of 67Ga scintigraphy in the diagnosis and assessment of
the effects of treatment (4,12).
However, our case showed that FDG-PET/CT imaging is a more reliable
and sensitive method for staging and monitoring therapy as opposed
to 67Ga scintigraphy in cases of PAL, which is in
agreement with Kostakoglu et al (13). Zinzani et al performed an
extensive analysis of the reliability of PET after induction
treatment in patients with Hodgkin's disease and aggressive
non-Hodgkin's lymphoma. Findings of these authors showed that there
were no false-negative results among 75 PET scans performed in that
study (14).
PAL is a non-Hodgkin's lymphoma that develops in the
pleural cavity following a long-standing history of CP, and is
strongly associated with EBV infection. In our first case,
histopathological analysis showed that the neoplastic cells were
positive for LMP-1, suggesting an association with EBV infection.
Takakuwa et al reported that the downregulation of EBV
nuclear antigen-2 expression may be a selection pressure for the
progression of PAL (3).
In conclusion, we report three cases of PAL that
showed a high FDG uptake in the lesions of PAL on the FDG-PET/CT
scan. FDG-PET/CT imaging is therefore useful in the evaluation of
the area of invasion, facilitation of treatment planning, as well
as the assessment of treatment response in PAL.
Acknowledgements
We thank Mr. Kenji Kawai for the technical
assistance.
References
|
1
|
Nakatsuka S, Yao M, Hoshida Y, Yamamoto S,
Iuchi K and Aozasa K: Pyothorax-associated lymphoma: a review of
106 cases. J Clin Oncol. 20:4255–4260. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Aozasa K: Pyothorax-associated lymphoma. J
Clin Exp Hematop. 46:5–10. 2006. View Article : Google Scholar
|
|
3
|
Takakuwa T, Ham MF, Luo WJ, Nakatsuka S,
Daibata M and Aozasa K: Loss of expression of Epstein-Barr virus
nuclear antigen-2 correlates with a poor prognosis in cases of
pyothorax-associated lymphoma. Int J Cancer. 118:2782–2789. 2006.
View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Ueda T, Andreas C, Itami J, Miyakawa K,
Fujimoto H, Ito H and Roos JE: Pyothorax-associated lymphoma:
imaging findings. AJR Am J Roentgenol. 194:76–84. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Weiler-Sagie M, Bushelev O, Epelbaum R,
Dann EJ, Haim N, Avivi I, Ben-Barak A, Ben-Arie Y, Bar-Shalom R and
Israel O: (18)F-FDG avidity in lymphoma readdressed: a study of 766
patients. J Nucl Med. 51:25–30. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Cronin CG, Swords R, Truong MT,
Viswanathan C, Rohren E, Giles FJ, O'Dwyer M and Bruzzi JF:
Clinical utility of PET/CT in lymphoma. AJR Am J Roentgenol.
194:W91–W103. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Asakura H, Togami T, Mitani M, Takashima
H, Yokoe K, Yamamoto Y, Nishiyama Y, Monden T, Toyama Y and Ohkawa
M: Usefulness of FDG-PET imaging for the radiotherapy treatment
planning of pyothorax-associated lymphoma. Ann Nucl Med.
19:725–728. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Ueda S, Tsuda H, Asakawa H, Shigekawa T,
Fukatsu K, Kondo N, Yamamoto M, Hama Y, Tamura K, Ishida J, Abe Y
and Mochizuki H: Clinicopathological and prognostic relevance of
uptake level using 18F-fluorodeoxyglucose positron
emission tomography computed tomography fusion imaging
(18F-FDG PET/CT) in primary breast cancer. Jpn J Clin
Oncol. 38:250–258. 2008.PubMed/NCBI
|
|
9
|
Abe Y, Tamura K, Sakata I, Ishida J, Mukai
M, Ohtaki M, Nakamura M and Machida K: Unique intense uptake
demonstrated by 18F-FDG positron emission
tomography/computed tomography (PET/CT) in primary pancreatic
lymphoma: A case report. Oncol Lett. 4:605–607. 2010.PubMed/NCBI
|
|
10
|
Fujimoto M, Haga H, Okamoto M, Obara E,
Ishihara M, Mizuta N, Nishimura K and Manabe T: EBV-associated
diffuse large B-cell lymphoma arising in the chest wall with
surgical mesh implant. Pathol Int. 58:668–671. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Santini M, Fiorello A, Vicidomini G,
Busiello L and Baldi A: A surgical case of pyothorax-associated
lymphoma of T-cell origin arising from the chest wall in chronic
empyema. Ann Thorac Surg. 88:642–645. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Aruga T, Itami J, Aruga M, Nakajima K,
Shibata K, Nojo T, Yasuda S, Uno T, Hara R, Isobe K, Machida N and
Ito H: Treatment for pyothorax-associated lymphoma. Radiother
Oncol. 56:59–63. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Kostakoglu L and Goldsmith SJ: Fluorine-18
fluorodeoxyglucose positron emission tomography in the staging and
follow-up of lymphoma: is it time to shift gears? Eur J Nucl Med.
27:1564–1578. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Zinzani PL, Fanti S, Battista G, Tani M,
Castellucci P, Stefoni V, Alinari L, Farsad M, Musuraca G, Gabriele
A, Marchi E, Nanni C, Canini R, Monetti N and Baccarani M:
Predictive role of positron emission tomography (PET) in the
outcome of lymphoma patients. Br J Cancer. 91:850–854.
2004.PubMed/NCBI
|