Introduction
Breast disease includes various benign and malignant
disorders. Among the malignant lesions, carcinoma of breast is the
most common type of cancer among women worldwide (1); its increasing incidence has surpassed
that of cervical cancer, and it has become the most common
malignancy among Indian women as well (2). According to the GLOBOCAN 2020 data,
>2 million women were diagnosed with breast cancer and there
685,000 related deaths globally. The age-standardized incidence
rate for breast cancer in females worldwide was shown to be 47.8
and in Asia it was 36.8 per 100,000 women (3). According to the study by Malvia et
al (2), the age-adjusted
incidence of breast cancer is as high as 41 per 100,000 women for
Delhi followed by Chennai (37 per 100,000 women), Bangalore (34.4
per 100,000 women) and the Thiruvananthapuram district (33.7 per
100,000 women) in India (2). Some
of the common clinical symptoms of female breast disease include
palpable breast lumps, breast pain and nipple discharge (4). Therefore, one of the key challenges
for the treating clinician is whether the breast lump is malignant
or benign. On the other hand, patients are also mentally stressed
anticipating breast cancer even though the majority of breast
lesions are benign (5,6).
The evaluation of breast lumps includes a detailed
clinical history, breast examination, imaging techniques and a
tissue diagnosis. However, the triple test is very useful for the
diagnosis of breast cancer, which includes a physical examination
of the breast, mammography and fine needle aspiration (FNA)
cytology (FNAC) of the breast lump (7).
Among these tests, FNAC is considered a
cost-effective, minimally invasive and relatively painless
procedure with rapid results. It has a good sensitivity and
specificity, and is highly accurate in the diagnosis of breast
carcinoma (8). Since some of the
breast lesions do not require surgical intervention, the
pre-operative cytological diagnosis can reduce unwanted surgeries,
thus reducing the morbidity rate (9).
In order to increase the quality, clarity and
reproducibility of FNA reports, the International Academy of
Cytology (IAC), has developed the classification of breast lesions
into the C1 to C5 category, as reported on cytology results
(10), which helps not only in the
proper communication between the pathologist and clinician, but is
also useful in deciding upon more effective treatment options for
the management of patients with breast cancer.
A thorough clinical examination of a breast lump is
the first step in the triple assessment approach, as well as for
the FNA procedure. Both breasts and axillae should be examined
methodically by the clinician. Although it may be tempting to
bypass the physical examination due to the availability of other
more targeted investigative techniques, such as mammography or
ultrasonography, the findings of the physical examination are
critical for the optimal diagnosis and management of breast disease
(11). Previous studies have also
revealed that only by combining all three assessment methods
optimal sensitivity and specificity can be achieved (11,12).
Thus, the present study aimed to evaluate the significant
differences in the clinical examination features of benign and
malignant breast lumps utilizing cytological data.
Materials and methods
Patients and examined parameters
The present study was a prospective
clinicopathological study of patients who presented with breast
lumps in the FNA clinic of a tertiary care Hindu Rao Hospital and
NDMC Medical College. The present study was performed after
obtaining approval from Institutional Ethics Committee, NDMC
Medical College and Hindu Rao Hospital vide letter no.
IEC/NDMC/2022/109 dated 17.06.2022. All guidelines as per the
Declaration of Helsinki and good clinical practice guidelines were
followed. Informed written consent from the patients for
participation was also obtained.
Over a period of 1 year from October, 2022 to
October, 2023, a total of 301 cases of all patients with breast
lesions who had given consent for participation were included for a
cytological examination. The patients who had not given written
consent for participation were excluded from the study. Following
proper counselling about the FNAC procedure, all related clinical
features including age, the sex of the patients, side, site, size
of lump, duration of symptoms, consistency of lump, tenderness and
mobility of lump were noted. The patients underwent FNA sampling by
an experienced cytopathologist and a smear was made by spreading
the aspirate material with the aid of another clean glass slide.
The smear was stained using Romanowsky stain (May Grunwald-Giemsa
stain, Merck India). Absolute methanol was used for the fixation of
air dried FNAC smear for 5 min at room temperature. Subsequently,
the fixed smear was stained with May Grunwald stain, followed by
Giemsa stain for 10 min each at room temperature. The smear was
washed with tap water thoroughly and air-dried. The stained smear
was mounted with DPX mountant. Subsequently, a microscopic
evaluation was performed by a senior cytopathologist using a
compound light microscope (Olympus Corporation). On the basis of
types of obtained cells, nuclear characteristics and
intracytoplasmic features of cells, a specific cytological
impression was made and the lesions were categorized according to
the IAC classification system for the FNAC of breast lesions
reporting into categories from C1 to C5. The clinical features
studied include the patients' age, sex, side of the lesion, site of
the lesion, size of the lesion, duration of symptoms, consistency
of the lump, tenderness and mobility of the lump. The duration of
symptoms is presented in months. The size of the lesion was
measured in centimeter squared (cm2). For further
statistical analysis, the C4 and C5 categories were combined and
considered as the malignant group, to be compared with the benign
group comprising of categories C1, C2 and C3.
Statistictal analysis
Statistical analysis was performed using Python
language package V3.0 (https://www.python.org) along with Jupyter V5.0
(https://jupyter.org) as the IDE for Python
language. The Mann-Whitney test, Fisher's exact test and the
Kruskal-Wallis test were used to assess the association between
various clinicopathological features of breast lumps and the
diagnosis of the lesion. Bonferroni's correction was applied
following Fisher's exact test for the multiple comparisons of the
categorical data. In the case that the results of the
Kruskal-Wallis test were statistically significant, Dunn's post hoc
test was then performed. A P-value <0.05 was considered to
indicate a statistically significant difference.
Results
Out of 301 patients with breast lumps, 296 were
females and only 5 were male, with a female to male ratio of
59.2:1. The overall range of patients' age was 6 to 75 years with a
mean age of 28.97 years (SD ± 12.25 years). The maximum incidence
of breast lumps was found in the age group of 21-30 years (113/301
cases, 37.54%), followed by the group of 11-20 years (83/301 cases,
27.57%) and 31-40 years (51/301 cases, 16.94%). The mean age of the
benign cases was 27.4 years (SD ± 10.6 years) and the mean age of
the malignant cases was 50.4 years (SD ± 14.2 years). This
difference in the mean age between the two groups was statistically
significant (P=0.001, Mann-Whitney test, Table I).
 | Table IAnalysis of the age and tumor size of
the patients. |
Table I
Analysis of the age and tumor size of
the patients.
| A, Age
distribution |
|---|
| Age group
(years) | Total cases, n
(%) | Benign cases, n
(%) | Malignant cases, n
(%) |
|---|
| 1-10 | 4 (1.33) | 4 (1.43) | 0 |
| 11-20 | 83 (27.57) | 83 (29.64) | 0 |
| 21-30 | 113 (37.54) | 112(40) | 1 (4.76) |
| 31-40 | 51 (16.94) | 47 (16.78) | 4 (19.05) |
| 41-50 | 35 (11.63) | 26 (9.29) | 9 (42.86) |
| 51-60 | 9 (2.99) | 7 (2.5) | 2 (9.52) |
| 61-70 | 3 (1.0) | 0 | 3 (14.29) |
| 71-80 | 3 (1.0) | 1 (0.36) | 2 (9.52) |
| Mean ± SD | 28.97±12.25
years | 27.4±10.6
yearsa | 50.4±14.2
yearsa |
| Total | 301(100) | 280 (93.02) | 21 (6.98) |
| B, Tumor size |
| | Total cases
(n=301) | Benign cases
(n=280) | Malignant cases
(n=21) |
| Median (range) | 2.0 (0.04-117.0)
cm2 | 2.0 (0.04-117.0)
cm2b | 4.0 (0.64-100.0)
cm2b |
Among all the breast lesion cases, 93.02% were
benign (280 cases), as compared with 6.98% (21 cases) malignant
lesions. However, all male breast lumps were benign. Furthermore,
all the benign lumps were diagnosed as fibroadenoma (157 cases,
52.16%), which was the most common diagnosis followed by
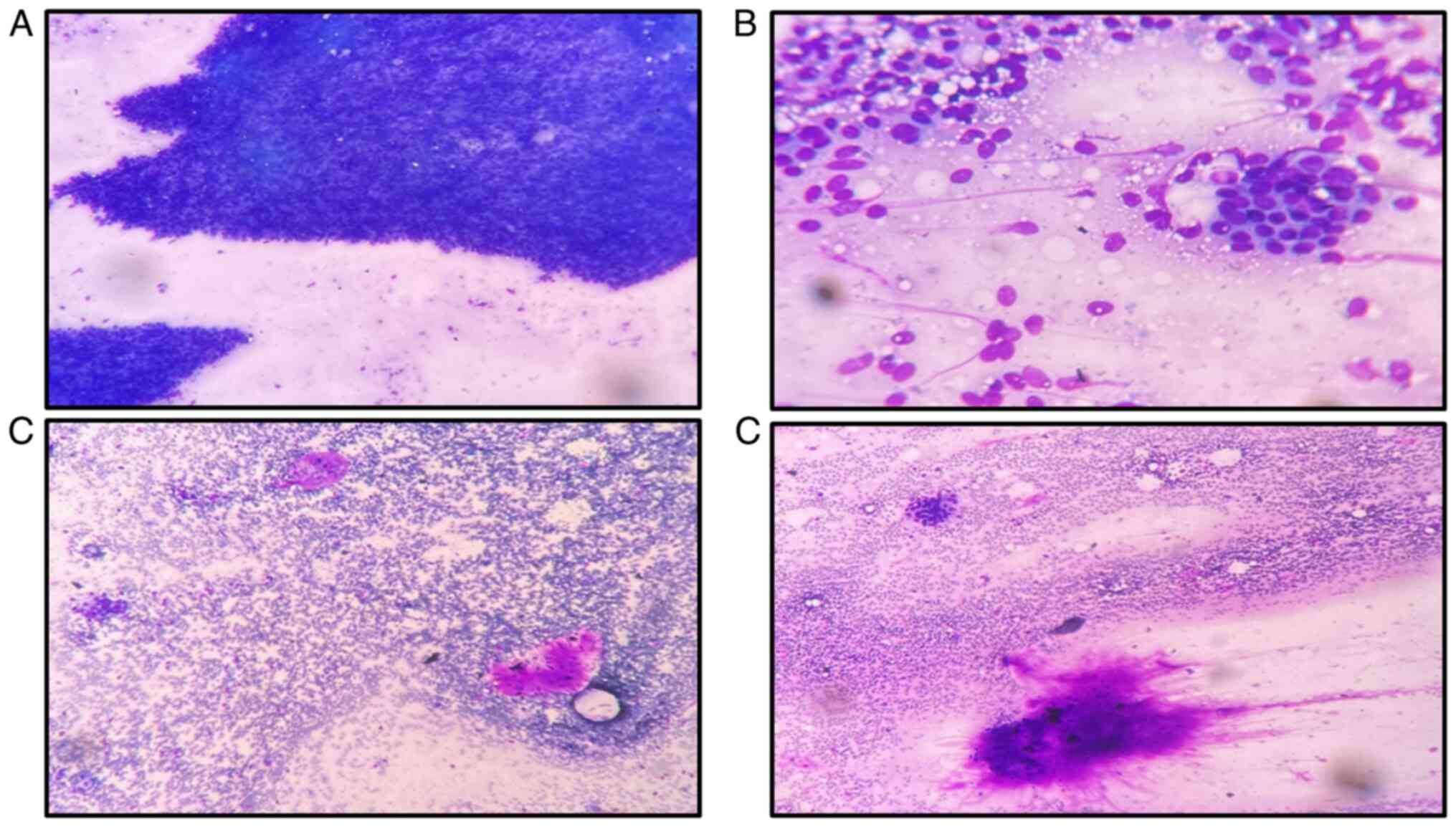
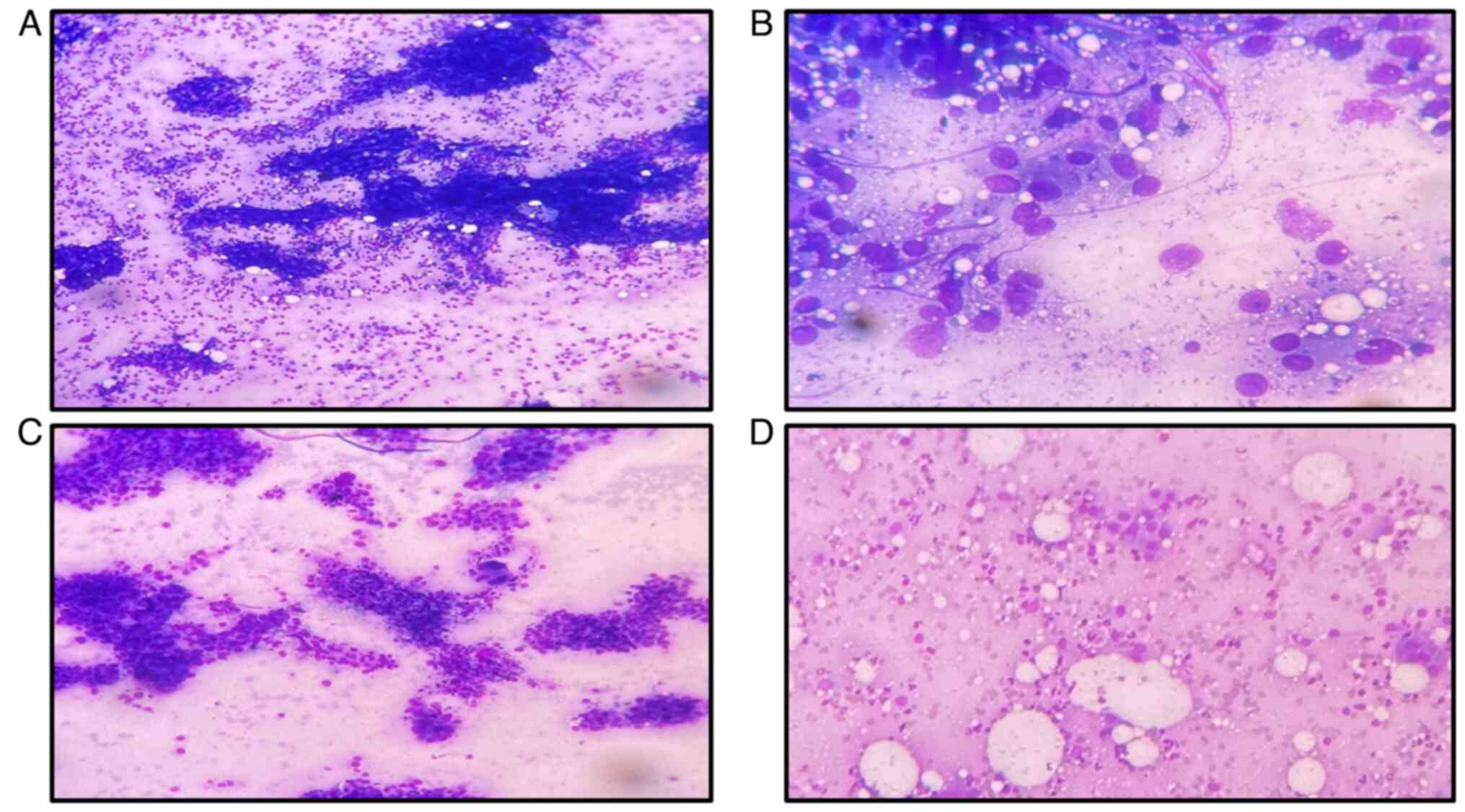
inflammatory lesion/mastitis/abscess (22 cases, 7.31%) (Figs. 1 and 2). The distribution of cases according to
the IAC reporting system is presented in Table II.
 | Table IIDistribution of breast lesions
according to the IAC reporting system. |
Table II
Distribution of breast lesions
according to the IAC reporting system.
| IAC | Description | Frequency | Percentage |
|---|
| C1 |
Insufficiency/unsatisfactory | 59 | 19.6 |
| C2 | Benign | 197 | 65.4 |
| C3 | Atypical probably
benign | 24 | 8.0 |
| C4 | Suspicious for
malignancy | 9 | 3.0 |
| C5 | Malignant | 12 | 4.0 |
| Total | | 301 | 100 |
The median duration of presentation of breast lumps
for the male subjects was 2 months (range, 1-6 months), which was
lower than that for the female subjects (4 months; range, 0.1-144
months). However, this difference between males and females was not
statistically significant (P=0.351, Mann-Whitney test, Table III). The present study also
analyzed the site of the breast lump; it was found that upper-outer
quadrant (113 cases, 37.5%) was the most common site, followed by
the upper-inner quadrant (73 cases, 24.2%) and sub-areolar area (55
cases, 18.27%). In terms of the side of the breast lump, right side
lumps were the most common (166/301 cases, 55.15%), closely
followed by left (127/301 cases, 42.19%) and bilateral (8 cases,
2.7%) lumps (Table IV).
 | Table IIIAnalysis of the duration of
clinicopathological features. |
Table III
Analysis of the duration of
clinicopathological features.
| A, Sex |
|---|
| Duration | Total (n=301) | Male (n=5) | Female (n=296) | P-value |
|---|
| Median (range) | 4 (0.1-144)
months | 2 (1-6) months | 4 (0.1-144)
months | P=0.351,
Mann-Whitney test |
| B, Nature of
lesion |
| Duration | Total (n=301) | Benign cases
(n=280) | Malignant cases
(n=21) | P-value |
| Median (range) | 4 (0.1-144)
months | 4 (0.1-144)
months | 4 (0.1-48)
months | P=0.767,
Mann-Whitney test |
| C, Laterality |
| Duration | Total (n=301) | Left (n=127) | Right (n=166) | Bilateral
(n=8) |
P-valuea |
| Median (range) | 4 (0.1-144)
months | 6 (0.1-144)
months | 3 (0.1-120)
months | 12 (1-120)
months | P=0.018,
Kruskal- Wallis test |
| D, IAC
category |
| Duration | Total (n=301) | C1 (n=59) | C2 (n=197) | C3 (n=24) | C4 (n=9) | C5 (n=12) |
P-valueb |
| Median (range) | 4 (0.1-144)
months | 4 (0.1-120)
months | 4 (0.1-144)
months | 12 (0.2-84)
months | 2 (0.1-12)
months | 7.5 (0.5-48)
months | P=0.039,
Kruskal- Wallis test |
 | Table IVDistribution of breast lesions
according to clinical features and comparison with IAC
category. |
Table IV
Distribution of breast lesions
according to clinical features and comparison with IAC
category.
| A, Site of
tumor |
|---|
| Site | Total (%) | C1 | C2 | C3 | C4 | C5 |
|---|
| Upper-outer | 113 (37.54) | 24 | 66 | 12 | 3 | 8 |
| Lower-outer | 42 (13.95) | 7 | 31 | 3 | 1 | 0 |
| Sub-areolar | 55 (18.27) | 15 | 33 | 5 | 2 | 0 |
| Upper-inner | 73 (24.25) | 7 | 57 | 2 | 3 | 4 |
| Lower-inner | 14 (4.65) | 3 | 10 | 1 | 0 | 0 |
| Axillary tail of
breast | 4 (1.34) | 3 | 0 | 1 | 0 | 0 |
| Total | 301(100) | Overall Fisher's
exact testa,
P=0.022 |
| B, Site of tumor
(upper half) |
| Site | Total (%) | C1 | C2 | C3 | C4 | C5 |
| Upper half | 186 (61.8) | 31 | 123 | 14 | 6 | 12 |
| Non-upper half | 115 (38.2) | 28 | 74 | 10 | 3 | 0 |
| Total | 301(100) | Overall Fisher's
exact testb,
P=0.028 |
| C, Laterality of
tumor |
| Laterality | Total (%) | C1 | C2 | C3 | C4 | C5 |
| Left | 127 (42.19) | 26 | 86 | 8 | 2 | 6 |
| Right | 166 (55.15) | 30 | 107 | 15 | 7 | 6 |
| Bilateral | 8 (2.66) | 1 | 6 | 1 | 0 | 0 |
| Total | 301(100) | Overall Fisher's
exact testc,
P=0.852 |
| D, Mobility of
tumor |
| Mobility | Total (%) | C1 | C2 | C3 | C4 | C5 |
| Mobile | 294 (97.7) | 58 | 197 | 23 | 8 | 8 |
| Non-mobile | 7 (2.3) | 1 | 0 | 1 | 1 | 4 |
| Total | 301(100) | Overall Fisher's
exact testd,
P=0.001 |
| E, Consistency of
tumor |
| Consistency | Total (%) | C1 | C2 | C3 | C4 | C5 |
| Firm,
non-tender | 288 (95.7) | 56 | 193 | 22 | 8 | 9 |
| Firm, tender | 7 (2.31) | 1 | 4 | 2 | 0 | 0 |
| Hard,
non-tender | 6 (1.99) | 2 | 0 | 0 | 1 | 3 |
| | 301(100) | Overall Fisher's
exact teste,
P=0.001 |
The mean size of the benign lumps was 4.90
cm2 (SD ± 11.18; median, 2 cm2, ranging
0.04-117.0 cm2) as compared with the mean size of
malignant lumps, which was 13.01 cm2 (SD ± 22.42; median
4 cm2, ranging 0.64-100.0 cm2). This
difference was statistically significant (P=0.002, Mann-Whitney
test, Table I).
The duration of presentation of breast lumps was
also analyzed for each side. The median duration of presentation in
patients with bilateral breast lumps was significantly higher (12
months; range, 0.1-120 months) compared with that in patients with
right-sided breast lumps (3 months; range, 0.1-120 months; P=0.044;
Dunn's test), whereas no significant difference (P=0.204; Dunn's
test) was found for the presentation of lumps between bilateral (12
months; range, 0.1-120 months) and left-sided lumps (6 months;
range, 0.1-144 months). However, the difference in duration of
presentation between right- and left-sided lumps were statistically
significant (P=0.024; Dunn's test; Table III).
Moreover, the median duration of presentation was
greater for patients in the C3 category (12 months; range, 0.2-84
months) than for those in the C2 and C5 categories (4 months;
range, 0.1-144 months) and 7.5 months (range, 0.5-48 months),
respectively (Table III).
From the analysis of the difference in duration of
presentation among different IAC categories of breast lesions,
overall statistically significant differences were found among
various IAC categories (P=0.039, Kruskal-Wallis test). Furthermore,
it was found that the difference in the duration of presentation
between C1 and C3, C2 and C3, and C3 and C4 was statistically
significant (P=0.006, P=0.021 and P=0.015, respectively, Dunn's
test), whereas it was insignificant between the remainder of the
categories of breast lesions (all P>0.05, Dunn's test, Table III). The mean duration of
presentation of benign cases was 12.37 months (SD ± 21.59 months)
with median 4 months, ranging 0.1-144 months as compared with the
mean duration of presentation of 7.52 months (SD ± 10.38 months)
with median 4 months, ranging 0.1-48 months for malignant cases;
however, this difference was not statistically significant
(P=0.767, Mann Whitney test). Moreover, the median duration of
presentation in both benign and malignant patients was 4 months
with a range of 0.1-144 and 0.1-48 months, respectively (Table III).
The percentage of non-mobile lumps in categories C2
(0/197 cases), C3 (1/24 cases) and C5 (4/12 cases) was 0, 4.2 and
33.3%, respectively. Among the categories, the difference in
mobility between C1 and C5, and C2 and C5 breast lumps was
statistically significant (P=0.020 and P=0.010, respectively;
Fisher's exact test). However, the difference in mobility between
rest of the categories was not statistically significant (all
P>0.05, Fisher's exact test, Table
IV).
The percentage of breast lumps with a hard,
non-tender consistency in the malignant group (C4 and C5; 4/21
cases) was 19%, whereas in the benign group (C1, C2 and C3; 2/280
cases) this was about 1% only. In terms of IAC category, the
percentage of hard, non-tender lumps in category C5 (3/12 cases)
was 25%, whereas in C2 and C3, this was 0%. This difference in
consistency only between C2 and C5 breast lumps was found to be
statistically significant (P=0.010, Fisher's exact test). The
difference in consistency between other remaining categories of
breast lump was insignificant (all P>0.05, Fisher's exact test,
Table IV).
In the present study, there was no significant
difference found in laterality (side) among all the IAC category of
breast lumps (P=0.852, Fisher's exact test, Table IV).
The proportions of breast lumps in the upper
quadrant for categories C1 (31/59 cases), C2 (123/197 cases), C3
(14/24 cases), C4 (6/9 cases) and C5 (12/12 cases) were 52.5, 62.4,
58.3, 66.7 and 100%, respectively, whereas the proportions of lumps
in quadrants other than the upper quadrant were 47.5% (28/59
cases), 37.6% (74/197 cases), 41.7% (10/24 cases), 33.3% (3/9
cases) and 0% (0/12 cases), for categories in the C1 to C5 in
sequence, respectively. This difference in quadrant (site) between
the C1 and C5 breast lesions was statistically significant
(P=0.020, Fisher's exact test). However, this difference in
quadrant was insignificant (all P>0.05, Fisher's exact test)
between the remaining of the breast lesions category (Table IV).
Discussion
The incidence of breast cancer has been
significantly increasing globally, which predominantly affects the
health of women and has an adverse cosmetic impact in females
(13). Although cytological
techniques, particularly FNAC are emerging as a key diagnostic
tools for the preoperative assessment of palpable breast lumps, the
clinical examination of breast lumps also plays a crucial role for
the evaluation of breast lumps.
In the present study, the number of female patients
was higher than that of male patients, with a male to female ratio
of 59.2:1, which was higher than 26:1 and 4:1, as reported by
Embaye et al (13) and
Qadri et al, respectively (14). Overall, the mean age of the
patients was slightly lower in the present study than in the
studies by Embaye et al (13) (mean age, 33.05 years) and Madan
et al (15) (mean age 34.54
years).
In the present study, it was found that the maximum
incidence of breast lumps occurred in the age group of 21-30 years
followed by the age group of 11-20 years, which can be considered
as younger age group (<30 years). Additionally, the mean age of
presentation was significantly higher for patients with
malignancies than for those with benign lesions. This finding is
similar to that of other studies performed by Rioki et al
(16), Madan et al
(15), Embaye et al
(13) and Khanam et al
(1), as they also reported the
maximum incidence of cases in younger (<30 years) age group.
However, the study by Singh and Tyagi (17) reported that patients aged 31 to 40
years had the most cases of breast lumps.
Moreover, the present study revealed that
fibroadenoma was the most common diagnosis followed by inflammatory
lesion/mastitis/abscess among the benign lesions of the breast.
These findings are in agreement with those of other studies
performed by Singh and Tyagi, Rioki et al (16), Madan et al (15), Qadri et al (14), Embaye et al (13) and Khanam et al (1). These authors also reported that the
most common diagnosis was fibroadenoma in benign lesions (1,13-17).
In contrast to previous studies, FNA clinic of Hindu Rao Hospital
deals with a variety of benign lesions with significant proportions
of benign cases other than fibroadenomas.
However, the present study also reported that 19.6%
of FNA procedures in the IAC category C1
(insufficient/unsatisfactory). This may be due to involvement of
fresh DNB/post graduate student in FNA procedure. Although the
adequacy of FNAC is dependent on multiple factors, the experience
of the operator is second most common cause for its inadequacy. In
previous studies, the percentage of inadequacy of aspiration was
shown to range from 0.7 to 25.3%. As stated in the study by Mendoza
et al (18), the success
rate of FNAC is also dependent on the experience of the
operator.
The significance of various clinical features of
breast lumps should be considered. The present study assessed the
association of different clinical features of breast lumps with the
diagnosis of the lesions. The present study reported that the
duration of presentation of breast lumps in males was lower than
that in the female; this may be due to the reason that breasts in
male are not developed; moreover; even minimal changes can be
immediately noticeable by the patient.
In terms of the site of breast lumps, in the present
study, it was found that the majority of the lumps were in the
upper quadrant of the breast. This finding is in accordance with
the findings of the study by Khanam et al (1).
The present study also analyzed the laterality
(side) of breast lumps and found that breast lumps were most common
in the right-sided breast as compared with the left-sided and
bilateral breasts. This result was similar to that of the study by
Qadri et al (14). However,
in the study done Khanam et al (1), left-sided breast lumps were reported
to be the most common.
In the present study, the median size of breast
lumps was significantly lower in patients with lumps as compared
with those with malignant lumps (median size, 2 vs. 4
cm2, respectively). A previous study also revealed that
the malignant lesion was larger in size than the benign (19).
Moreover, following the analysis of the duration of
presentation of breast lumps for each side, it was found that
duration of presentations of lumps was highest in the bilateral
breast as compared with the left and right-sided breast. The
duration of presentation of lumps was also higher in the
left-compared with the right-sided breast.
In terms of mobility and consistency of the breast
lumps, the present study found significant differences in mobility,
as well as consistency between the malignant and benign lumps. The
malignant lumps were non-mobile, whereas the benign lumps were
mobile. In addition, in terms of the consistency of lumps,
malignant lumps were hard and non-tender, while the benign ones
were not.
To the best of our knowledge, none of the studies
published to date in the English language have assessed the
association between the duration of presentation of breast lumps,
mobility and consistency and the IAC category of breast lesions. In
view of this, the significant findings of the present study, in the
context of the duration of presentation, mobility and consistency
of breast lumps are key factors.
There were no significant differences found in the
laterality and IAC category of the lesions, except for the
localization (site) of the lumps. It was found that the upper
quadrant of the breast was the most prevalent site for malignant
lesions, whereas for benign lesions, the non-upper quadrant was the
most prevalent site. In previous studies performed by Chan et
al (20) and Hussain (21), it was also reported that the upper
quadrant was dominant site for overall palpable breast lumps.
In conclusion, there were statistically significant
differences between some of the clinical features, namely the
duration of presentation, site, mobility, consistency of breast
lump and cytology category. Considering that the clinical
examination features of breast lump is crucial for the effective
diagnosis of breast disease, the findings of the present study not
only re-emphasize (12) the
importance of thorough clinical examination of patient with breast
lumps, but can also be considered as relevant for the better
management of breast lumps.
Acknowledgements
Not applicable.
Funding
Funding: No funding was received.
Availability of data and materials
The datasets used and/or analyzed during the current
study are available from the corresponding author on reasonable
request.
Authors' contributions
All authors (SKS, SS and SK) contributed to the
conception and design of the study. Material preparation was
performed by SKS and SS. Data collection and analysis were
performed by SKS and SS. Analysis was performed by SKS and SS. SS
and SK confirm the authenticity of all the raw data. The first
draft of the manuscript was written by SKS and all authors
commented on previous versions of the manuscript. All authors have
read and approved the final version of the manuscript.
Ethics approval and consent to
participate
The present study was performed after obtaining
approval from the Institutional Ethics Committee, NDMC Medical
College and Hindu Rao Hospital, Delhi vide letter no.
IEC/NDMC/2022/109 dated 17.06.2022 and written informed consent
from the patients for participation was also obtained. The present
study was conducted in accordance with the Declaration of
Helsinki.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Khanam KF, Akter N, Tabashum T, Raza AKM,
Hosna AU, Rahman F and Begum A: A clinicopathologic study of
various breast lesions by fine needle aspiration cytology (FNAC). J
Curr Surg. 8:27–31. 2018.
|
|
2
|
Malvia S, Bagadi SA, Dubey US and Saxena
S: Epidemiology of breast cancer in Indian women. Asia Pac J Clin
Oncol. 13:289–295. 2017.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Sung H, Ferlay J, Siegel RL, Laversanne M,
Soerjomataram I, Jemal A and Bray F: Global cancer statistics 2020:
GLOBOCAN estimates of incidence and mortality worldwide for 36
cancers in 185 countries. CA Cancer J Clin. 71:209–249.
2021.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Nkonge KM, Rogena EA, Walong EO and Nkonge
DK: Cytological evaluation of breast lesions in symptomatic
patients presenting to Kenyatta National Hospital, Kenya: A
retrospective study. BMC Womens Health. 15(118)2015.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Sankaye SB and Dongre SD: Cytological
study of palpable breast lumps presenting in an Indian rural setup.
Indian J Med Paediatr Oncolc. 35:159–164. 2014.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Brakohiapa EK, Armah GE, Clegg-Lamptey JN
and Brakohiapa WO: Pattern of breast diseases in Accra: Review of
mammography reports. Ghana Med J. 47:101–106. 2013.PubMed/NCBI
|
|
7
|
Kaufman Z, Shpitz B, Shapiro M, Rona R,
Lew S and Dinbar A: Triple approach in the diagnosis of dominant
breast masses: Combined physical examination, mammography, and
fine-needle aspiration. J Surg Oncol. 56:254–257. 1994.PubMed/NCBI View Article : Google Scholar
|
|
8
|
de Cursi JAT, Marques MEA, de Assis Cunha
Castro CAC, Schmitt FC and Soares CT: Fine-needle aspiration
cytology (FNAC) is a reliable diagnostic tool for small breast
lesions (≤1.0 cm): A 20-year retrospective study. Surg Exp Pathol.
3(29)2020.
|
|
9
|
Bhagat R, Bal MS, Bodal VK, Suri AK and
Jindal K: Cytological study of palpable breast lumps with their
histological correlation. Int J Med Dent Sci. 2:128–136. 2013.
|
|
10
|
Field AS, Schmitt F and Vielh P: IAC
standardized reporting of breast fine-needle aspiration biopsy
cytology. Acta Cytol. 61:3–6. 2017.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Karim MO, Khan KA, Khan AJ, Javed A, Fazid
S and Aslam MI: Triple assessment of breast lump: Should We perform
core biopsy for every patient? Cureus. 12(e7479)2020.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Provencher L, Hogue JC, Desbiens C,
Poirier B, Poirier E, Boudreau D, Joyal M, Diorio C, Duchesne N and
Chiquette J: Is clinical breast examination important for breast
cancer detection? Curr Oncol. 23:e332–e339. 2016.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Embaye KS, Raja SM, Gebreyesu MH and
Ghebrehiwet MA: Distribution of breast lesions diagnosed by
cytology examination in symptomatic patients at Eritrean National
Health Laboratory, Asmara, Eritrea: A retrospective study. BMC
Womens Health. 20(250)2020.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Qadri S, Khan SP, Farooq S and Bhat AR:
Cytomorphological pattern of breast lesions diagnosed on
fine-needle aspiration cytology in a district hospital in Kashmir
valley. Int J Adv Med. 9:814–817. 2022.
|
|
15
|
Madan M, Sharma M, Mannan R, Manjari M,
Kaur J and Garg S: Cytomorphological study of spectrum of breast
lesions and determination of efficacy of FNAC in the diagnosis of
various breast lesions. J Evol Med Dent Sci. 4:9581–9587. 2015.
|
|
16
|
Rioki JN, Muchiri L, Mweu M, Songok E and
Rogena E: Cytomorphological patterns of breast lesions among women
with palpable breast lumps attending select teaching and referral
hospitals in Kenya: A descriptive cross-sectional study. Pan Afr
Med J. 44(171)2023.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Singh S and Tyagi MS: A prospective study
on cytological evaluation of palpable breast lumps. Int J Contemp
Med Res. 7:H1–H4. 2020.
|
|
18
|
Mendoza P, Lacambra M, Tan PH and Tse GM:
Fine needle aspiration cytology of the breast: The nonmalignant
categories. Patholog Res Int. 2011(547580)2011.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Ballo MS and Sneige N: Can core needle
biopsy replace fine-needle aspiration cytology in the diagnosis of
palpable breast carcinoma. A comparative study of 124 women.
Cancer. 78:773–777. 1996.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Chan S, Chen JH, Li S, Chang R, Yeh DC,
Chang RF, Yeh LR, Kwong J and Su MY: Evaluation of the association
between quantitative mammographic density and breast cancer
occurred in different quadrants. BMC Cancer. 17(274)2017.PubMed/NCBI View Article : Google Scholar
|
|
21
|
Hussain MT: Comparison of fine needle
aspiration cytology with excision biopsy of breast lump. J Coll
Physicians Surg Pak. 15:211–214. 2005.PubMed/NCBI
|