1. Introduction
Cardiovascular disease refers to a group of diseases
that affect the heart and blood vessels and contributes to
approximately 30% of global mortality, making it the most
contributory cause of mortality worldwide. Although the events
leading to cardiovasucular disorders are multi-faceted, a
fundamental problem is the presence of scar tissue, and the
irreversible loss of cardiomyocytes, which dynamically contribute
to the contractility and the relaxation of ventricles. This can
eventually predispose to ventricular arrhythmias and lead to heart
failure (HF).
Traditional therapeutic options employ a strategy to
limit further scar formation and adverse remodeling (1), but do not address the problem of
cardiomyocyte loss which can only be treated by heart
transplantation. In view of the palliative rather curative effect
of these treatments, new alternative therapies have been explored
for over a decade, including gene, protein and stem cell therapies.
In particular, stem cell therapy has become a new focal point for
the treatment of cardiovascular disorders. The demonstration that
bone marrow-derived mono-nuclear cells (BMMNCs) can repair
myocardial damage and improve heart function by favoring myocardial
regeneration or reduction of ventricular remodelling has generated
great expectations (2). This
discovery has transformed experimental research in the field of
regenerative cardiovascular medicine and considerably increased the
clinical investigation. Herein, we present an overview on advances
in stem cell therapy for cardiovascular disease. Specifically, in
this review, we address the present state of research as regards
different stem cells that may be used to regenerate the myocardium,
their modes of delivery and their mechanisms of action.
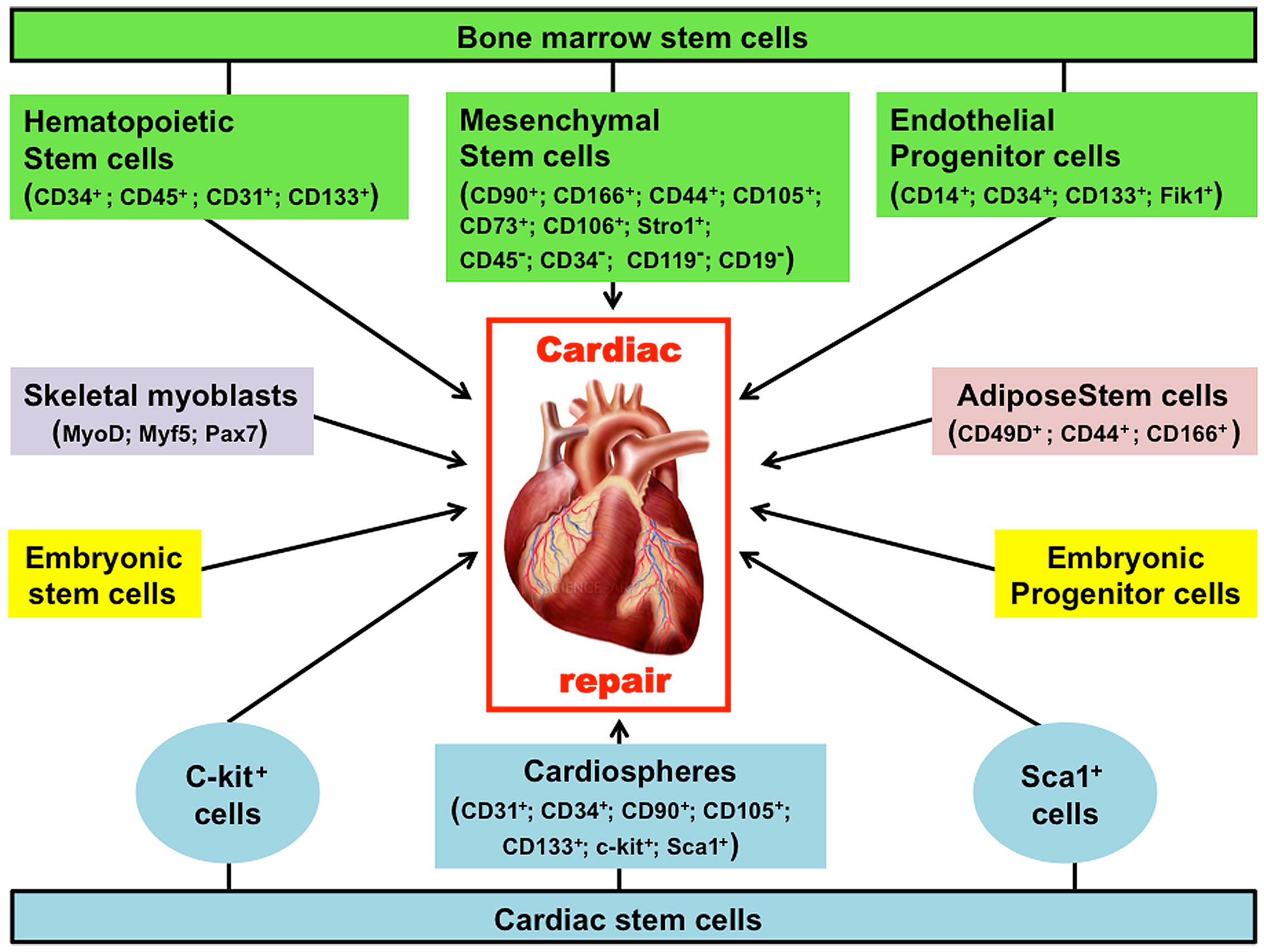
2. Spectrum of stem cells investigated
Since the first study reported in 1998 indicating
the ability of skeletal muscle to repair the heart (3), various cell types illustrated in
Fig. 1, have been investigated as
possible candidates for treatment of cardiovascular disease.
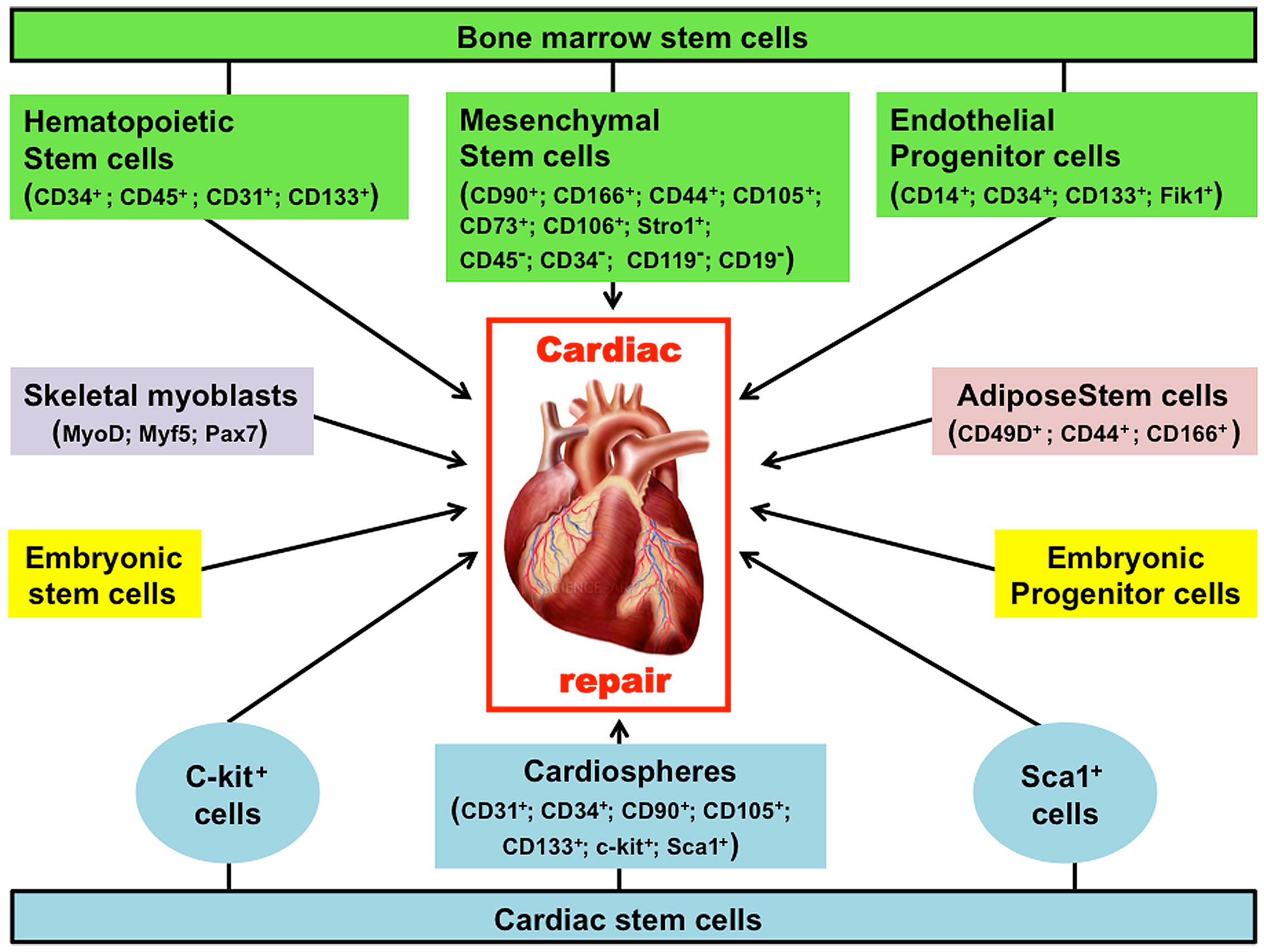 | Figure 1Spectrum of stem cells investigated
for cardiac repair. Although the pathologic events leading to
injured heart are multi-faceted, an underlying cause is a
diminished blood supply to parts of the myocardium as a result of
an occlusion to coronary artery. This translates into low, or no
oxygen supply to the cardiac muscle leading to wide apoptosis and
necrosis of the cells. As consequence, the heart cannot pump blood
effectively to the rest of the body, thus leading to heart failure
and ultimately death of the patient. The main purpose of stem cell
therapies is the prevention and or regeneration of dying muscle. A
variety of cell types have been investigated as candidates for such
treatment. These cells include skeletal myoblasts, whole bone
marrow cells or bone marrow-derived HSCs, bone marrow-derived MSCs,
adipose-derived stem cells, adult cardiac resident stem cells, and
ESCs including their differentiated progeny. The surface marker
phenotypes that distinguish certain different stem cells are given
in parentheses. HSCs, hematopoietic stem cells; MSCs, mesenchymal
stem cells; ESCs, embryonic stem cells. |
Skeletal myoblasts (SMs)
Given that SMs are believed to have sufficient
plasticity to give rise to cardiac muscle, specimens of SMs
obtained from muscle biopsies were originally used for cardiac
regeneration (3). Advantageously,
these cells have the ability to derive autologous cells, thus
eliminating the need for immunosupression (4,5).
In addition, SMs have a high proliferative ability at a later stage
of differentiation and are resistant to ischemia (3–5).
Preclinical and clinical studies have revealed that SMs could
differentiate into myotubes and form skeletal muscle-like grafts
that are viable and functional in the damaged portions of
myocardium. These changes were accompanied by a reduction in
adverse ventricular remodelling and interstitial fibrosis as well
as increased cardiac function (3–7).
However, the inability of these implanted skeletal muscle cells to
differentiate into cardiomyocytes (6), and to form electrical junctions
(6) has raised potential concerns
as regards the risk of ventricular tachycardia, and waned interest
in their use for treatment of cardiovascular disease.
Bone marrow-derived stem cells
Bone marrow harbors several types of stem cells that
include mesenchymal and hematopoietic stem cells (HSCs) that have
been largely tested for their use in tissue/organ regeneration in
several preclinical and clinical studies. These cells are easily
procurable and also include unfractionated mononuclear cells, and
endothelial progenitor cells (EPCs).
BMMNCs
In several animal models of acute myocardial
infarction (AMI), BMMNCs have been used (2,8)
and were found to contribute to the regeneration of cardiomyocytes
and endothelial cells following injection into infarcted
myocardium.
The first clinical trial of BMMNCs in AMI, carried
out in 2002 by Strauer et al (9), revealed that these cells improved
global and regional ventricular function and enhanced myocardial
perfusion. Similar results were obtained more recently in two
separate trials of BMMNCs in AMI (10,11). However, a double-blind
investigation of BMMNC transplantation in the placebo-controlled
LateTIME trial, at 2–3 weeks after myocardial infarction (MI)
revealed no improvement in regional or global cardiac function
(12). Furthermore, although the
analysis of cohort studies and randomized clinical trials has shown
a modest benefit in favor of BMMNCs in the treatment of patients
suffering from left ventricular (LV) dysfunction post-MI, neutral
result from other studies of autologous BMMNCs continue to fuel
controversy about the clinical role of this potential new
therapeutic tool.
Mesenchymal stem cells (MSCs)
MSCs are non-hematopoietic cells that have the
potential to differentiate into a variety of cell types. They have
initially been identified in bone marrow, but are also found in
umbilical cord blood, adipose tissue, and the heart. Importantly,
MSCs from bone marrow do not express costimulatory molecules of the
T-cell activation such as HLA class II and B7, allowing them to
survive even under inflammatory conditions without interacting with
host T cells. The use of these cells in rodent models of MI
resulted in improvement of remodeling and reduction of infarct size
following their differentiation into cardiomyocyte and endothelial
phenotypes (13). Similarly,
intracoronary infusion of autologous bone marrow-derived MSCs given
to patients after MI resulted in improved LV function and
myocardial perfusion (14). In
the setting of HF, infusion of autologous or allogeneic MSCs
improved ventricular remodeling as well as the functional capacity,
and quality of life of patient (15).
HSCs and EPCs
HSCs present in the bone marrow have the potential
to differentiate into myeloid as well as lymphoid cell lineages.
Whereas, EPCs are found in peripheral blood and they can
differentiate into endothelial cells to promote neovascularisation
in response to ischemic injury. CD34 and CD133 are surface markers
of both HSCs and EPCs.
A sustained improvement in regional perfusion and LV
remodeling by intracoronary cell therapy with both
CD133+ or CD34+ cell types could be observed
in old anterior MI patients (16). Interestingly, injection of
CD34+ cells into the peri-infarct during coronary artery
bypass grafting (CABG) surgery in patients with ischemic
cardiomyopathy led to better improvement of contractile function as
compared to CABG alone (17).
Similarly, left ventricular ejection fraction (LVEF) and perfusion
of the infarcted myocardium were found to be much improved in
ischemic HF patients who received CABG and CD133+
therapy in contrast to patients treated only with CABG (18). The use of a novel population of
hematopoietic cells, known as aldehyde dehydrogenase-bright
(ALDHbr) cells, resulted in reduced LV end-systolic
volume and an improvement of maximal oxygen consumption (19).
Adipose-derived MSCs
Miyahara et al were the first investigators
to practice transplantation of adipose-derived MSCs into scarred
myocardium in a rat model of chronic MI, and reported that this
intervention led to better cardiac function, which was associated
with reversal of wall thinning in the scar area (20). A subsequent comparative study
demonstrated that MSCs not only help in improving LVEF, but they
also promote angiogenesis and lower fibrosis and this ability of
MSCs is better than adipose-derived cardiomyogenic cells or BMMNCs
(21). However, the application
of adipose-derived MSCs in the clinical setting for cardiovascular
disease is still under evaluation.
Cardiac stem cells (CSCs)
It is now known that there is a continuous turnover
of cellular components of adult heart and this is an important
development in our understanding of cardiac tissue biology. In as
much as this process of cardiac cellular turnover is likely to be
dependent on the population of stem cells present in the heart,
several cardiac-derived stem cells have been evaluated as potential
therapeutic tools.
c-kit+ CSCs
The c-kit+ CSCs refer to a multipotent
cell population expressing the tyrosine kinase receptor c-kit, and
are considered as a primary source for generation of a new
myocardium subsequent to injury. The ability of these
c-kit+ CSCs to curtail LV dysfunction and vascular
remodeling, and also to promote cardiac tissue regeneration was
consistently demonstrated in animal models of AMI (22–24). Clinical and preclinical studies
have suggested that the intracoronary infusion of autologous
c-kit+ CSCs results in the restoration of LV systolic
function, and reduces infarct size in patients with cardiovascular
disease due to ischemia (25).
Cardiosphere-derived cells (CDCs)
CDCs are composed of various cell types that include
cells expressing antigenic markers that are charactersitic of
endothelial cells [KDR (human)/Flk-1 (mouse), CD3], stem cells
(CD34, c-kit, Sca-1), and MSCs (CD105, CD90). These cells are able
to promote regeneration, and to reduce both post-MI dysfunction and
vascular remodeling in various animal models of MI (26–28); however, the specific cells
responsible for these effects have not yet been identified.
Nevertheless, considering that 98% of CDCs infused are found to be
positive for CDC105, it has been suggested that the stem cell type
responsible for this restoration is likely mesenchymal in nature
(26). However, therapy with CDCs
does not lead to a reduction in LV volume, an increase in LVEF, and
an improvement in quality of life. Nevertheless, therapy with CDCs
has been shown to lead to a 42% reduction in scar size along with
an increase in viable tissue and regional systolic wall thickening
in the infarcted region, which suggests cardiac regeneration
(26).
Sca-1+ CSCs
Oh et al (29) originally reported the presence of
Sca-1+ cells in the adult mouse heart, and demonstrated
that these cells express cardiac structural genes, and
differentiate into beating cardiomyocytes when treated with
5-azacydine or oxytocin. These authors also demonstrated that
Sca-1+ cells, when transplanted into the peri-infarct
and infarct zones in an animal model of MI, differentiated into
endothelial cells and cardiomyocytes, and attenuated LV
remodeling.
Embryonic stem cells (ESCs)
ESCs are considered to be promising therapeutic
candidate stem cells, since they are able to self-renew in an
unlimited manner and can differentiate into any cell type of the
organism, including cardiomyocytes. Accordingly, under appropriate
culture conditions, human ESCs form contracting areas (30) and embryoid bodies, which are
positive for cardiomyocyte markers such as myosin heavy chain,
α-actin, desmin and tropin I. The main advantage of ESCs is their
capacity of unlimited expansion in vitro, allowing them to
meet the need for large amounts of cells for transplantation. The
administration of ESCs in an animal model of MI has been shown to
result in engraftment, improved LV function and reduced LV
remodeling (31). The
disadvantages of ESCs are their propensity toward teratoma
formation, and malignant transformation.
Induced pluripotent stem cells
(iPSCs)
Adult human somatic cells (32) and mouse fibroblasts (33), reprogrammed to pluripotent stem
cells by transduction of transcription factors, were shown to
differentiate into cardiomyocytes which possess functional
properties typical of cardiac cells. Although these iPSCs are
potential therapeutic candidates for cardiac regeneration, the
transcription factors used for their generation such as cMyc, Oct4
and Klf4 are known oncogenes that can produce teratomas. In
addition, iPSCs have a very low efficiency for generation and this
varies among different batches of iPSCs, rendering their ability
unpredictable (34). The rapidly
evolving technology in this field may overcome these problems and
the iPSC-based therapeutic approach could find applications in the
treatment of cardiovascular disease.
3. Modes of stem cell delivery
The transplantation of sufficient numbers of cells
into the myocardial region of interest and the achievement of
maximum retention of cells within the area represent the primary
objective of any cell delivery strategy. Current delivery
strategies are transvascular approaches, and direct injection into
the LV wall.
Transvascular approaches
The transvascular strategies are particularly
appropriate for recent infarcted and reperfused myocardium when
expression of chemo-attractants and cell adhesion molecules is
prominent. These strategies include intracoronary delivery,
intravenous infusion, and mobilisation of stem cells.
Intracoronary delivery
In this approach, cells are infused inside the
coronary artery, and this is generally done during brief coronary
occlusion caused by inflating a balloon at the tip of the catheter
(35–37). The advantages of this procedure
include the uniform distribution of injected cells in the infarcted
region, relative simplicity of the technique without the need for
specialized equipment. The procedure is practical for widespread
utilization in clinical practice. However, intracoronary delivery
has some disadvantages. Indeed, with this approach, the immediate
retention of cells is low, there is a possibility of microvascular
occlusion due to large cells, and the cell delivery to a myocardial
region supplied by an occluded artery is impossible (35–37).
Intravenous infusion
It has been shown that the intravenous delivery of
EPCs (38) or MSCs (39) improves cardiac function in animal
models following AMI, while the homing of cells to non-cardiac
organs limits the clinical application of this approach. Indeed,
the myocardial homing of BMMNCs was found important only following
intracoronary stop-flow delivery, but not after intravenous
injection in patients with post-AMI (40).
Mobilization of stem cells
Given that the infarcted myocardium attracts
circulating stem cells to the site of injury, the mobilization of
stem cells by cytokines may provide a non-invasive approach for
cardiac regeneration. This possibility was tested preclinically in
animal models of AMI (41) and
clinically in patients with AMI and chronic myocardial ischemia
(42).
Direct injection into the ventricular
wall
The direct injection of cells into the ventricular
wall is considered as a favored method for cell delivery when an
occluded coronary artery precludes transvascular cell delivery or
when cell homing signals are expressed at low levels in the heart.
However, the direct injection of cells into the ischemic or scarred
myocardium creates islands of cells with limited blood supply. This
may lead to poor cell survival. Different approaches of direct
injection are particularly appropriate for the application of large
cells, such as MSCs or SMs that may cause microembolization
following intracoronary delivery. These approaches have been used
in patients with advanced coronary artery disease or ischemic
cardiomyopathy, but may be technically challenging in patients with
AMI, particularly if cells have to be injected into the border zone
of the infarct. The safety of such an approach should be
investigated, as the perforation of the friable necrotic tissue is
a matter of concern. In general, direct injection can be performed
by transendocardial, transepicardial, or transcoronary delivery
(43).
Transepicardial injection
Transepicardial injection is performed as an adjunct
to CABG during cardiac surgery. The procedure permits the direct
visualization of the myocardium and the targeted application of
cells to scarred areas and the border zone of an infarct scar.
However, the efficiency of cell transplantation may be difficult to
evaluate and determine if CABG is performed simultaneously
(44).
Transendocardial injection
In this approach, cells are delivered directly
inside the LV with an injection catheter advanced across the aortic
valve and positioned against the endocardial surface.
Advantageously, electromechanical mapping of the endocardial
surface with a catheter-based nonfluoroscopic three-dimensional
(NOGA) system (45) can be used
to monitor ischemic and scarred but viable myocardium, thereby
facilitating targeted injection of cells into the scar or into the
border zone. In addition, cells can be distributed in a scarred
region, even in the presence of a total occlusion of the coronary
artery supply (15). Given these
advantages, cell injection by transendocardial approach has been
largely performed in the clinical setting (46). However, it is important to note
that an intramyocardial injection can disrupt tissue architecture
and generate cell clumps that eventually die from a lack of
adequate blood supply. Furthermore, cells are always
heterogeneously distributed in the infarct zone.
Transcoronary vein injection
The procedure requires a catheter system
incorporating an ultrasound tip for guidance and an extendable
needle for myocardial access. With such a system, cells are
delivered parallel to the ventricular wall and deep into the
injured myocardium (47).
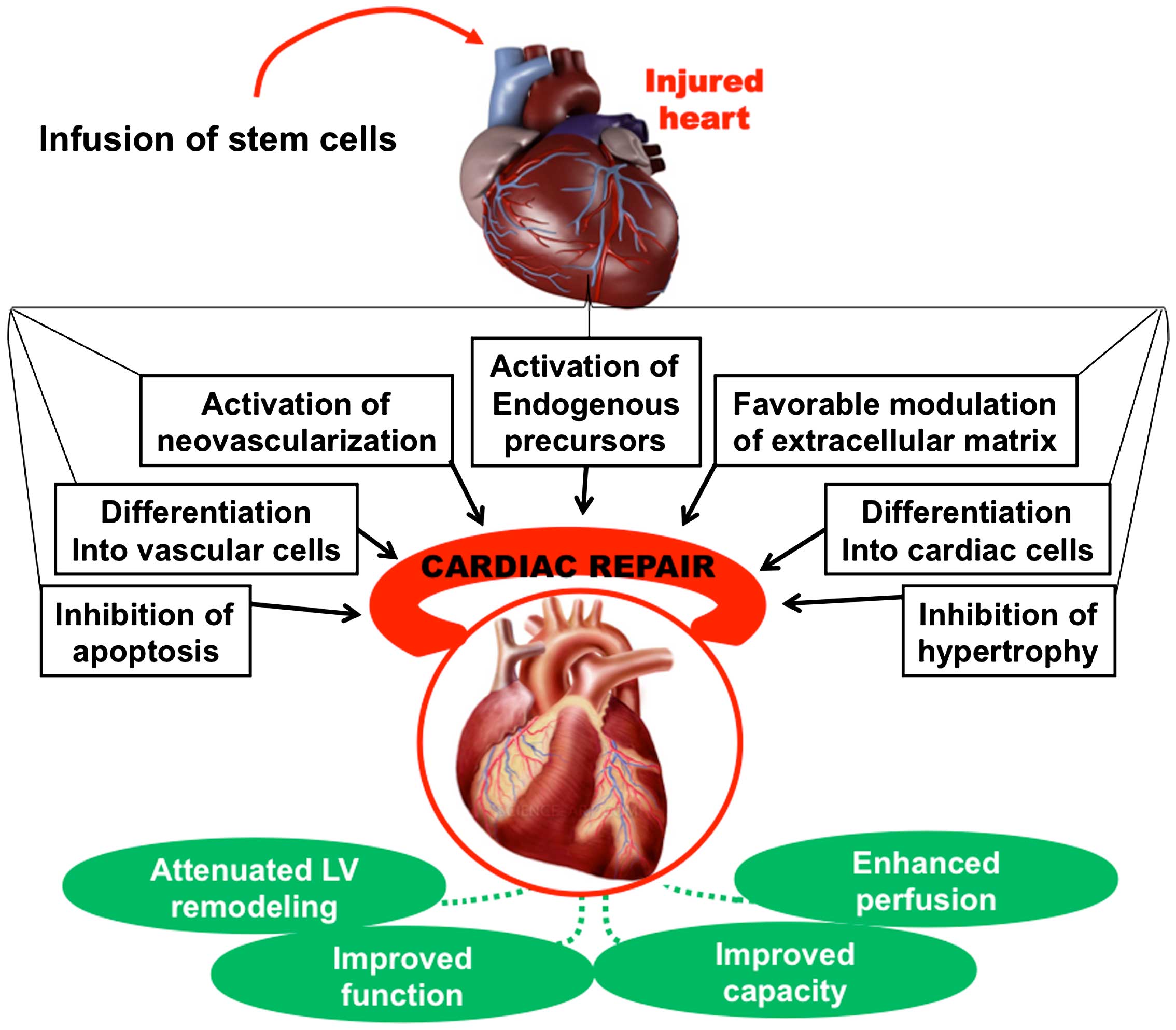
4. Potential therapeutic mechanisms of stem
cells
Stem cells have been reported to initiate myocardial
repair and improve cardiac function through direct and indirect
mechanisms, including differentiation into cardiac and vascular
cells, paracrine effects and cell fusion (Fig. 2).
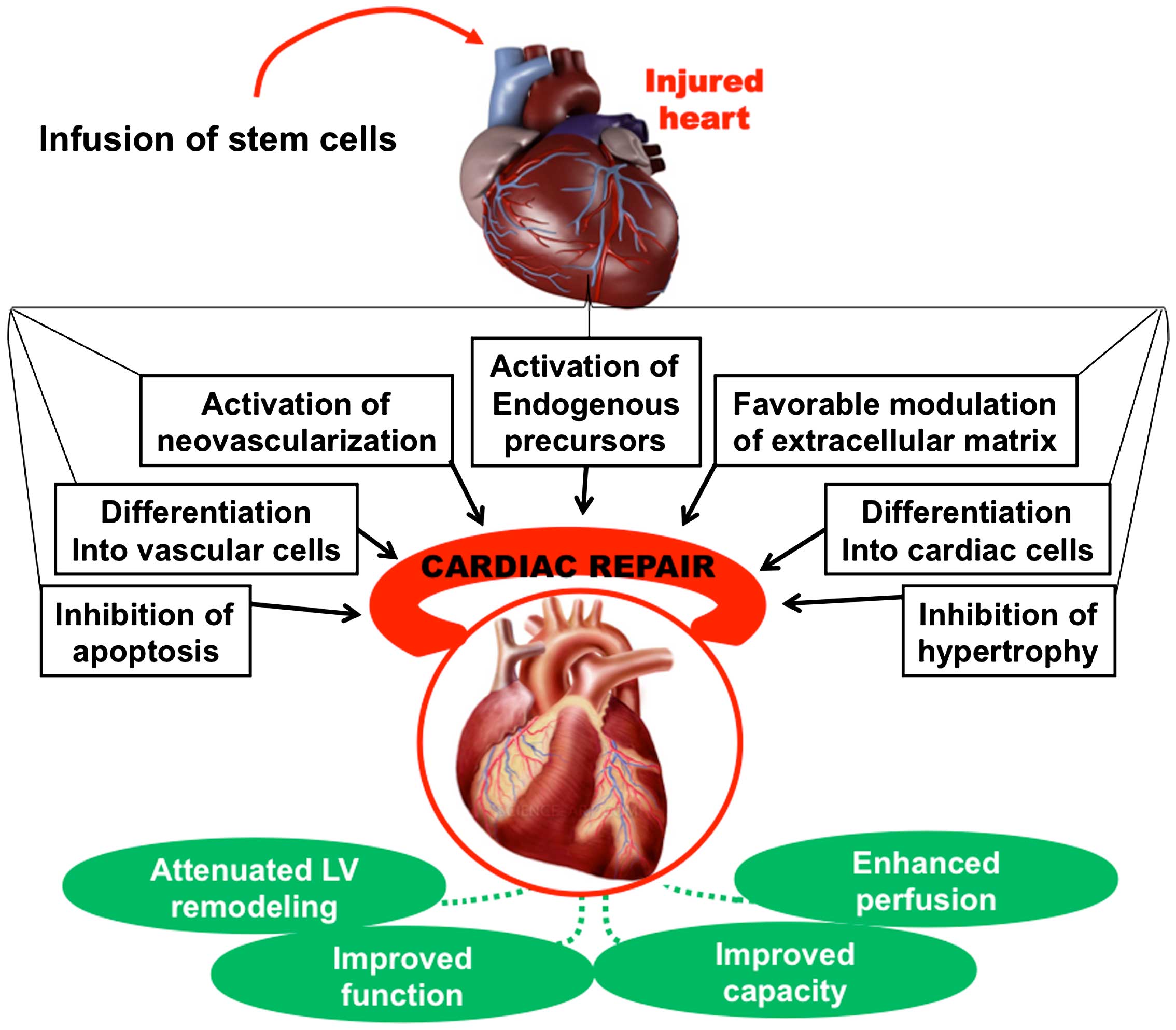 | Figure 2Potential therapeutic mechanisms of
stem cells. Infusion of stem cells in the injured heart initiates
myocardial repair via several direct and indirect mechanisms,
including differentiation into cardiac and vascular cells, cell
fusion and paracrine effects such as activation of endogenous
precursors, promotion of neovascularisation, favorable modulation
of the extracellular matrix, inhibition of apoptosis, and
inhibition of hypertrophy. Collectively, these events result in
enhanced LV function, improved perfusion, and improved cardiac
function, leading to improvement in clinical status. |
Differentiation of transplanted stem
cells into cardiac cells
The differentiation of injected stem cells into
cardiomyocytes is one of the major controversies in the field of
cardiac regeneration. Indeed, although differentiation may provide
the clearest explanation for the therapeutic effect of transplanted
stem cells, there is no clear evidence supporting this. While
certain studies using genetic and fluorescent labeling support the
differentiation as important mechanism for cardiac regeneration
(2,48–50), other studies challenge this notion
despite improved LV function (8,48).
Accordingly, the majority of stem cell-based therapies have
reported improvement of both LV function and vascular remodeling,
without necessarily forming new cardiomyocytes.
Formation of new blood vessels from
transplanted stem cells
Various cell types have demonstrated the ability to
differentiate into new blood vessels following their
transplantation. This phenomenon is likely essential for models of
chronic coronary occlusion with ischemic but viable myocardium,
however, not for models with infarcted and scarred myocardium
(49). Interestingly, patients
with ischemic heart disease have demonstrated improved cardiac
performance, which was associated with formation of new vessels
from transplanted stem cells (50). This is indicative of the clinical
importance of stem cell differentiation in patients suffering from
ischemic cardiomyopathy. It is however, difficult to envisage the
process in the setting of non-ischemic cardiomyopathy or in
patients suffering from ischemic heart disease but without
flow-limiting coronary lesions.
Paracrine effect
Paracrine effect is a concept that has been proposed
to provide an explication regarding the therapeutic effects of
transplanted stem cells on injury tissues. It refers to the notion
that transplanted stem cells repair damaged myocardium by releasing
into the surrounding tissue, several factors such as cytokines,
chemokines, growth factors, exosomes or microparticles, which
initiate various processes of restoration that include activation
of endogenous CSCs, neovascularisation (51), inhibition of apoptosis, inhibition
of hypertrophy, and favorable alterations of the extracellular
matrix.
Cell fusion
Cell fusion refers to a cellular mechanism in which
many mononuclear cells combine to form a syncytium. A study
examining cell fusion events of BMMNCs with cardiomyocytes using a
procedure based on Cre-lox recombination, has indicated that cell
fusion is the alternative mechanism used by transplanted BMMNCs to
generate different adult tissues (4). However, subsequent studies concluded
that cell fusion is not required for the differentiation of BMMNCs
into cardiomyocytes and coronary vessels (52). Furthermore, the Cre-lox
recombination-based method appears inappropriate to study cell
fusion, since unmodified Cre-recombinase in stem cells can imitate
cell fusion by crossing the cell membrane. Consequently, the
importance of cell fusion in therapeutic mechanisms of the stem
cell seems stripped of support.
5. Conclusion
Despite considerable resources and effort dedicated
over the last decade to study the bioactivity of stem cells and
examine their potentiality for clinical intervention, stem cell
therapy for cardiovascular disease remains a relatively young
science. Nevertheless, remarkable progress has been made in a
relatively short time during which, most of clinical trials
conducted were generally small and inconclusive. However, the
results were encouraging, and the stem cell therapy appears safe.
This therapeutic approach is likely a clinical reality that may
revolutionize the treatment of cardiovascular disease.
References
|
1
|
Zannad F, Agrinier N and Alla F: Heart
failure burden and therapy. Europace. 11(Suppl 5): v1–v9. 2009.
View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Orlic D, Kajstura J, Chimenti S, Jakoniuk
I, Anderson SM, Li B, Pickel J, McKay R, Nadal-Ginard B, Bodine DM,
et al: Bone marrow cells regenerate infarcted myocardium. Nature.
410:701–705. 2001. View
Article : Google Scholar : PubMed/NCBI
|
|
3
|
Taylor DA, Atkins BZ, Hungspreugs P, Jones
TR, Reedy MC, Hutcheson KA, Glower DD and Kraus WE: Regenerating
functional myocardium: improved performance after skeletal myoblast
transplantation. Nat Med. 4:929–933. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Murry CE, Wiseman RW, Schwartz SM and
Hauschka SD: Skeletal myoblast transplantation for repair of
myocardial necrosis. J Clin Invest. 98:2512–2523. 1996. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Pagani FD, DerSimonian H, Zawadzka A,
Wetzel K, Edge AS, Jacoby DB, Dinsmore JH, Wright S, Aretz TH,
Eisen HJ and Aaronson KD: Autologous skeletal myoblasts
transplanted to ischemia-damaged myocardium in humans. Histological
analysis of cell survival and differentiation. J Am Coll Cardiol.
41:879–888. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Menasché P, Hagège AA, Scorsin M, Pouzet
B, Desnos M, Duboc D, Schwartz K, Vilquin JT and Marolleau JP:
Myoblast transplantation for heart failure. Lancet. 357:279–280.
2001. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Menasché P, Hagège AA, Vilquin JT, Desnos
M, Abergel E, Pouzet B, Bel A, Sarateanu S, Scorsin M, Schwartz K,
et al: Autologous skeletal myoblast transplantation for severe
postinfarction left ventricular dysfunction. J Am Coll Cardiol.
41:1078–1083. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Murry CE, Soonpaa MH, Reinecke H, Nakajima
H, Nakajima HO, Rubart M, Pasumarthi KB, Virag JI, Bartelmez SH,
Poppa V, et al: Haematopoietic stem cells do not transdifferentiate
into cardiac myocytes in myocardial infarcts. Nature. 428:664–668.
2004. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Strauer BE, Brehm M, Zeus T, Köstering M,
Hernandez A, Sorg RV, Kögler G and Wernet P: Repair of infarcted
myocardium by autologous intracoronary mononuclear bone marrow cell
transplantation in humans. Circulation. 106:1913–1918. 2002.
View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Traverse JH, Henry TD, Pepine CJ,
Willerson JT, Zhao DX, Ellis SG, Forder JR, Anderson RD,
Hatzopoulos AK, Penn MS, et al: Cardiovascular Cell Therapy
Research Network (CCTRN): Effect of the use and timing of bone
marrow mononuclear cell delivery on left ventricular function after
acute myocardial infarction: the TIME randomized trial. JAMA.
308:2380–2389. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Sürder D, Schwitter J, Moccetti T, Astori
G, Rufibach K, Plein S, Lo Cicero V, Soncin S, Windecker S,
Moschovitis A, et al: Cell-based therapy for myocardial repair in
patients with acute myocardial infarction: rationale and study
design of the SWiss multicenter Intracoronary Stem cells Study in
Acute Myocardial Infarction (SWISS-AMI). Am Heart J. 160:58–64.
2010. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Traverse JH, Henry TD, Ellis SG, Pepine
CJ, Willerson JT, Zhao DX, Forder JR, Byrne BJ, Hatzopoulos AK,
Penn MS, et al: Cardiovascular Cell Therapy Research Network:
Effect of intracoronary delivery of autologous bone marrow
mononuclear cells 2 to 3 weeks following acute myocardial
infarction on left ventricular function: the LateTIME randomized
trial. JAMA. 306:2110–2119. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Davani S, Marandin A, Mersin N, Royer B,
Kantelip B, Hervé P, Etievent JP and Kantelip JP: Mesenchymal
progenitor cells differentiate into an endothelial phenotype,
enhance vascular density, and improve heart function in a rat
cellular cardiomyoplasty model. Circulation. 108(Suppl 1):
II253–II258. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Chen SL, Fang WW, Ye F, Liu YH, Qian J,
Shan SJ, Zhang JJ, Chunhua RZ, Liao LM, Lin S and Sun JP: Effect on
left ventricular function of intracoronary transplantation of
autologous bone marrow mesenchymal stem cell in patients with acute
myocardial infarction. Am J Cardiol. 94:92–95. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Hare JM, Fishman JE, Gerstenblith G,
DiFede Velazquez DL, Zambrano JP, Suncion VY, Tracy M, Ghersin E,
Johnston PV, Brinker JA, et al: Comparison of allogeneic vs
autologous bone marrow-derived mesenchymal stem cells delivered by
transendocardial injection in patients with ischemic
cardiomyopathy: the POSEIDON randomized trial. JAMA. 308:2369–2379.
2012. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Manginas A, Goussetis E, Koutelou M,
Karatasakis G, Peristeri I, Theodorakos A, Leontiadis E, Plessas N,
Theodosaki M, Graphakos S, et al: Pilot study to evaluate the
safety and feasibility of intracoronary CD133(+) and CD133(−)
CD34(+) cell therapy in patients with nonviable anterior myocardial
infarction. Catheter Cardiovasc Interv. 69:773–781. 2007.
View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Patel AN, Geffner L, Vina RF, Saslavsky J,
Urschel HC Jr, Kormos R and Benetti F: Surgical treatment for
congestive heart failure with autologous adult stem cell
transplantation: aprospective randomized study. J Thorac Cardiovasc
Surg. 130:1631–1638. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Stamm C, Kleine HD, Choi YH, Dunkelmann S,
Lauffs JA, Lorenzen B, David A, Liebold A, Nienaber C, Zurakowski
D, et al: Intramyocardial delivery of CD133+ bone marrow
cells and coronary artery bypass grafting for chronic ischemic
heart disease: safety and efficacy studies. J Thorac Cardiovasc
Surg. 133:717–725. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Perin EC, Silva GV, Zheng Y, Gahremanpour
A, Canales J, Patel D, Fernandes MR, Keller LH, Quan X, Coulter SA,
et al: Randomized, double-blind pilot study of transendocardial
injection of autologous aldehyde dehydrogenase-bright stem cells in
patients with ischemic heart failure. Am Heart J. 163:415–421.
421.e12012. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Miyahara Y, Nagaya N, Kataoka M, Yanagawa
B, Tanaka K, Hao H, Ishino K, Ishida H, Shimizu T, Kangawa K, et
al: Monolayered mesenchymal stem cells repair scarred myocardium
after myocardial infarction. Nat Med. 12:459–465. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Mazo M, Planat-Bénard V, Abizanda G,
Pelacho B, Léobon B, Gavira JJ, Peñuelas I, Cemborain A, Pénicaud
L, Laharrague P, et al: Transplantation of adipose derived stromal
cells is associated with functional improvement in a rat model of
chronic myocardial infarction. Eur J Heart Fail. 10:454–462. 2008.
View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Linke A, Müller P, Nurzynska D, Casarsa C,
Torella D, Nascimbene A, Castaldo C, Cascapera S, Böhm M, Quaini F,
et al: Stem cells in the dog heart are self-renewing, clonogenic,
and multipotent and regenerate infarcted myocardium, improving
cardiac function. Proc Natl Acad Sci USA. 102:8966–8971. 2005.
View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Fischer KM, Cottage CT, Wu W, Din S, Gude
NA, Avitabile D, Quijada P, Collins BL, Fransioli J and Sussman MA:
Enhancement of myocardial regeneration through genetic engineering
of cardiac progenitor cells expressing Pim-1 kinase. Circulation.
120:2077–2087. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Angert D, Berretta RM, Kubo H, Zhang H,
Chen X, Wang W, Ogorek B, Barbe M and Houser SR: Repair of the
injured adult heart involves new myocytes potentially derived from
resident cardiac stem cells. Circ Res. 108:1226–1237. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Bolli R, Chugh AR, D'Amario D, Loughran
JH, Stoddard MF, Ikram S, Beache GM, Wagner SG, Leri A, Hosoda T,
et al: Cardiac stem cells in patients with ischaemic cardiomyopathy
(SCIPIO): initial results of a randomised phase 1 trial. Lancet.
378:1847–1857. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Makkar RR, Smith RR, Cheng K, Malliaras K,
Thomson LE, Berman D, Czer LS, Marbán L, Mendizabal A, Johnston PV,
et al: Intracoronary cardiosphere-derived cells for heart
regeneration after myocardial infarction (CADUCEUS): a prospective,
randomised phase 1 trial. Lancet. 379:895–904. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Smith RR, Marban E and Marban L: Enhancing
retention and efficacy of cardiosphere-derived cells administered
after myocardial infarction using a hyaluronan-gelatin hydrogel.
Biomatter. 3:e244902013. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Bonios M, Chang CY, Pinheiro A, Dimaano
VL, Higuchi T, Melexopoulou C, Bengel F, Terrovitis J, Abraham TP
and Abraham MR: Cardiac resynchronization by cardiosphere-derived
stem cell transplantation in an experimental model of myocardial
infarction. J Am Soc Echocardiogr. 24:808–814. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Oh H, Bradfute SB, Gallardo TD, Nakamura
T, Gaussin V, Mishina Y, Pocius J, Michael LH, Behringer RR, Garry
DJ, et al: Cardiac progenitor cells from adult myocardium: homing,
differentiation, and fusion after infarction. Proc Natl Acad Sci
USA. 100:12313–12318. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Kehat I, Khimovich L, Caspi O, Gepstein A,
Shofti R, Arbel G, Huber I, Satin J, Itskovitz-Eldor J and Gepstein
L: Electromechanical integration of cardiomyocytes derived from
human embryonic stem cells. Nat Biotechnol. 22:1282–1289. 2004.
View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Min JY, Yang Y, Converso KL, Liu L, Huang
Q, Morgan JP and Xiao YF: Transplantation of embryonic stem cells
improves cardiac function in postinfarcted rats. J Appl Physiol
(1985). 92:288–296. 2002.
|
|
32
|
Takahashi K, Tanabe K, Ohnuki M, Narita M,
Ichisaka T, Tomoda K and Yamanaka S: Induction of pluripotent stem
cells from adult human fibroblasts by defined factors. Cell.
131:861–872. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Takahashi K and Yamanaka S: Induction of
pluripotent stem cells from mouse embryonic and adult fibroblast
cultures by defined factors. Cell. 126:663–676. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Ma T, Xie M, Laurent T and Ding S:
Progress in the reprogramming of somatic cells. Circ Res.
112:562–574. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Strauer BE, Brehm M, Zeus T, Gattermann N,
Hernandez A, Sorg RV, Kogler G and Wernet P: Intracoronary, human
autologous stem cell transplantation for myocardial regeneration
following myocardial infarction. Dtsch Med Wochenschr. 126:932–938.
2001. View Article : Google Scholar : PubMed/NCBI
|
|
36
|
Bui QT, Gertz ZM and Wilensky RL:
Intracoronary delivery of bone-marrow-derived stem cells. Stem Cell
Res Ther. 1:292010. View
Article : Google Scholar : PubMed/NCBI
|
|
37
|
Wojakowski W, Tendera M, Cybulski W,
Zuba-Surma EK, Szade K, Florczyk U, Kozakowska M, Szymula A, Krzych
L, Paslawska U, Paslawski R, Milewski K, Buszman PP, Nabialek E,
Kuczmik W, Janiszewski A, Dziegiel P, Buszman PE, Jozkowicz A and
Dulak J: Effects of intracoronary delivery of allogenic bone
marrow-derived stem cells expressing heme oxygenase-1 on myocardial
reperfusion injury. Thromb Haemost. 108:464–475. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
38
|
Kawamoto A, Gwon HC, Iwaguro H, Yamaguchi
JI, Uchida S, Masuda H, Silver M, Ma H, Kearney M, Isner JM and
Asahara T: Therapeutic potential of ex vivo expanded endothelial
progenitor cells for myocardial ischemia. Circulation. 103:634–637.
2001. View Article : Google Scholar : PubMed/NCBI
|
|
39
|
Pittenger MF and Martin BJ: Mesenchymal
stem cells and their potential as cardiac therapeutics. Circ Res.
95:9–20. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
40
|
Hofmann M, Wollert KC, Meyer GP, Menke A,
Arseniev L, Hertenstein B, Ganser A, Knapp WH and Drexler H:
Monitoring of bone marrow cell homing into the infarcted human
myocardium. Circulation. 111:2198–2202. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
41
|
Norol F, Merlet P, Isnard R, Sebillon P,
Bonnet N, Cailliot C, Carrion C, Ribeiro M, Charlotte F, Pradeau P,
et al: Influence of mobilized stem cells on myocardial infarct
repair in a nonhuman primate model. Blood. 102:4361–4368. 2003.
View Article : Google Scholar : PubMed/NCBI
|
|
42
|
Powell TM, Paul JD, Hill JM, Thompson M,
Benjamin M, Rodrigo M, McCoy JP, Read EJ, Khuu HM, Leitman SF, et
al: Granulocyte colony-stimulating factor mobilizes functional
endothelial progenitor cells in patients with coronary artery
disease. Arterioscler Thromb Vasc Biol. 25:296–301. 2005.
View Article : Google Scholar
|
|
43
|
Archundia A, Aceves JL, Lopez-Hernandez M,
Alvarado M, Rodriguez E, Diaz QG, Paez A, Rojas FM and Montano LF:
Direct cardiac injection of G-CSF mobilized bone-marrow stem-cells
improves ventricular function in old myocardial infarction. Life
Sci. 78:279–283. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
44
|
Laham RJ, Post M, Rezaee M, Donnell-Fink
L, Wykrzykowska JJ, Lee SU, Baim DS and Sellke FW: Transendocardial
and transepicardial intramyocardial fibroblast growth factor-2
administration: Myocardial and tissue distribution. Drug Metab
Dispos. 33:1101–1107. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
45
|
Klemm HU, Franzen O, Ventura R and Willems
S: Catheter based simultaneous mapping of cardiac activation and
motion: a review. Indian Pacing Electrophysiol J. 7:148–159.
2007.PubMed/NCBI
|
|
46
|
Perin EC, Silva GV, Henry TD,
Cabreira-Hansen MG, Moore WH, Coulter SA, Herlihy JP, Fernandes MR,
Cheong BY, Flamm SD, Traverse JH, Zheng Y, Smith D, Shaw S,
Westbrook L, Olson R, Patel D, Gahremanpour A, Canales J, Vaughn WK
and Willerson JT: A randomized study of transendocardial injection
of autologous bone marrow mononuclear cells and cell function
analysis in ischemic heart failure (FOCUS-HF). Am Heart J.
161:1078–1087. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
47
|
Wu K, Mo X, Lu S and Han Z: Retrograde
delivery of stem cells: Promising delivery strategy for myocardial
regenerative therapy. Clin Transplant. 25:830–833. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
48
|
Limbourg FP, Ringes-Lichtenberg S,
Schaefer A, Jacoby C, Mehraein Y, Jäger MD, Limbourg A, Fuchs M,
Klein G, Ballmaier M, et al: Haematopoietic stem cells improve
cardiac function after infarction without permanent cardiac
engraftment. Eur J Heart Fail. 7:722–729. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
49
|
Leri A, Kajstura J and Anversa P: Cardiac
stem cells and mechanisms of myocardial regeneration. Physiol Rev.
85:1373–1416. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
50
|
Humar R, de Miguel LS, Kiefer FN and
Battegay EJ: Formation of new blood vessels in the heart can be
studied in cell cultures. (ALTEX Spec No 24). pp. 35–38. 2007
|
|
51
|
Kinnaird T, Stabile E, Burnett MS, Lee CW,
Barr S, Fuchs S and Epstein SE: Marrow-derived stromal cells
express genes encoding a broad spectrum of arteriogenic cytokines
and promote in vitro and in vivo arteriogenesis through paracrine
mechanisms. Circ Res. 94:678–685. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
52
|
Kajstura J, Rota M, Whang B, Cascapera S,
Hosoda T, Bearzi C, Nurzynska D, Kasahara H, Zias E, Bonafé M, et
al: Bone marrow cells differentiate in cardiac cell lineages after
infarction independently of cell fusion. Circ Res. 96:127–137.
2005. View Article : Google Scholar
|