Introduction
Globally, lung cancer has been revealed to be the
most common cancer, the leading cause of cancer mortality in males,
and the second leading cause of cancer mortality in females during
the year 2008 (1). Although
substantial progress in surgical, chemotherapeutic and
radiotherapeutic approaches has been made, the long-term survival
rate in patients with lung cancer still remains low (2). A key determinant of the appropriate
therapy provided to patients with lung cancer depends on the
accurate detection of lymph node metastasis. Therefore, the correct
assessment of the lymph node status is crucial for the prognosis of
patients with lung cancer.
Non-invasive diagnostic imaging modalities, i.e.,
computed tomography (CT) and magnetic resonance imaging (MRI), are
commonly used for the identification of metastatic lymph nodes in
patients with lung cancer. However, conventional CT and MRI rely on
morphological criteria to differentiate malignant from benign lymph
nodes. Lymph nodes may be enlarged due to other factors, including
inflammation, infection, autoimmune disease, and so forth, and even
small lymph nodes may be infiltrated by cancer cells (3,4).
Therefore, it remains a challenge for radiologists and clinicians,
on the basis of morphological characteristics, to distinguish
metastatic from non-metastatic lymph nodes. Positron emission
tomography (PET)/CT is a generally accepted non-invasive approach
for the staging of pulmonary cancer (5,6).
However, the use of PET/CT has been known to result in
false-negative results for well-differentiated lung adenocarcinoma,
and false-positive results for inflammatory lesions (7,8).
Furthermore, PET/CT is not widely available on account of its great
expense.
Recently, diffusion-weighted imaging (DWI) has
successfully been applied to thoracic imaging, and has demonstrated
great potential in the detection of lung cancer and metastatic
lymph nodes (5,9–15).
However, previously published studies have reported the diagnostic
performance of DWI for the detection of metastatic lymph nodes with
widely varying sensitivities and specificities (60–91 and 70–100%,
respectively) (11,14–22).
Thus, there has been a burgeoning interest in meta-analysis to
identify consistent results for the diagnostic performance of DWI
in detecting metastatic lymph nodes of lung cancer.
Wu et al (23)
published a meta-analysis that compared the diagnostic capability
of DWI with that of 18F-fluorodeoxyglucose PET/CT in the
lymph node staging evaluation of non-small cell lung cancer
(NSCLC); however, only three DWI studies were included in that
study. Another meta-analysis of differential diagnosis between
metastatic and non-metastatic lymph nodes using DWI featured a
great variety of primary tumors, although this meta-analysis only
included four DWI studies on lung cancer (24). The different biological or
histological characteristics of each primary tumor may lead to
decreased reliability of the pooled results. The aim of the present
study was to perform a meta-analysis for more comprehensive and
precise assessment of the diagnostic value of DWI, in order to
discriminate between metastatic and non-metastatic lymph nodes in
patients with lung cancer.
Materials and methods
Literature search strategy
Systematic literature searches of the PubMed,
Embase, Web of Science, Cochrane Library, China Biomedicine, China
National Knowledge Infrastructure and Wanfang databases were
performed for English and Chinese language studies published
between January 1994 and June 2015. A search algorithm based on a
combination of the following terms was used: ‘Diffusion magnetic
resonance imaging’ OR ‘diffusion MR imaging’ OR ‘diffusion weighted
imaging [MeSH]’ OR ‘DWI’ AND ‘lung neoplasms [MeSH]’ OR ‘lung
cancer’ OR ‘lung lesions’ AND ‘lymphatic metastasis’ OR ‘lymph node
metastasis’. The reference lists of identified articles were also
manually searched to obtain additional papers.
Inclusion and exclusion criteria
All DWI studies for detecting lymph node metastasis
in patients with lung cancer yielded by our document retrieval were
assessed for potential eligibility. The studies that fulfilled the
following inclusion criteria were included: i) The studies were
published in the English or Chinese language in a peer-reviewed
journal; ii) the studies must have evaluated the diagnostic
performance of DWI for identifying metastatic and non-metastatic
lymph nodes in patients with lung cancer; iii) the studies had to
present on lymph node-based, not on patient-based, statistical
results; iv) sufficient information regarding true-positive (TP),
false-positive (FP), true-negative (TN) and false-negative (FN)
values could be identified or calculated from data in the original
articles; v) pathological examination and/or follow-up imaging
findings should have been set as the reference standards; and vi)
where data or subsets of data were reported in more than one
article, the article with the larger sample size, or the latest
article, was adopted.
Studies were excluded if they met at least one of
the following deficiencies: i) The studies were conference
abstracts, letters, comments, case reports or review articles; ii)
the studies were not associated with lung cancer; iii) combinations
of multiple magnetic resonance sequences, i.e., contrast enhanced
imaging and DWI, were applied in the studies, and the diagnostic
performance of DWI could not be assessed alone; iv) sufficient raw
data could not be obtained from the articles to construct the
four-fold (2×2) tables; or v) sample sizes of <20 patients or 30
lymph nodes were presented in the studies.
Data extraction and quality
assessment
Two authors (G.-X.C and M.-H.W) independently
searched the literature, screened the retrieved articles, and
extracted relevant data, including the study characteristics and
results using Microsoft Excel sheets. For each included study, the
following characteristics were extracted: The first author's name,
year of publication, age and gender of patients, number of patients
and lymph nodes, type of lung cancer, study design, patient
selection, blind study, B-value, diagnostic threshold of apparent
diffusion coefficient (ADC), reference standard, type of scanner,
MRI field strength and the relevant data (i.e., TP, FP, TN and FN).
The quality of the included studies was also assessed independently
by the same two authors according to the ‘quality assessment of
diagnostic accuracy studies’ (QUADAS-2) (25). If agreement was not reached between
the two authors, a third author (T.Z.) evaluated all discrepant
items, and the major viewpoint was adopted for statistical
analysis.
Statistical analysis
Heterogeneity was assessed using the Q statistic of
the Chi-square value test and inconsistency index (I2),
and P<0.1 or I2>50% suggested the presence of
heterogeneity (26). If
heterogeneity was detected among the studies, the test's
performance was summarized using a random-effects model (the
DerSimonian and Laird method); otherwise, a fixed-effects model
(the Mantel-Haenszel method) was used. The predominant outcome
indexes were pooled sensitivity, specificity, positive likelihood
ratio (PLR), negative likelihood ratio (NLR), diagnostic odds ratio
(DOR) and their corresponding 95% confidence intervals (CIs). The
summary receiver operating characteristic (SROC) curve and area
under the SROC curve (AUC) were used to demonstrate the diagnostic
performance of DWI in the detection of metastatic lymph nodes of
lung cancer.
Exploring the sources of heterogeneity is essential
to seek the latent factors that affect the pooled accuracy from
various studies. In diagnostic accuracy studies, the threshold
effect has been regarded as one of the predominant causes of
heterogeneity (27). The threshold
effect can be recognized visually by observing the typical pattern
of a ‘shoulder-arm’ shape in the ROC plane. Furthermore, Spearman's
correlation coefficient between the logit of sensitivity and the
logit of (1-specificity) was calculated to identify the presence of
a threshold effect. Strong positive correlation, with P<0.05,
was considered to indicate the existence of a threshold effect
(28).
In addition, in order to investigate the influence
of heterogeneity between individual studies on pooled diagnostic
performance, meta-regression analysis was performed to identify
those variables causing heterogeneity. Subgroup analysis was
further performed according to these identified variables. The
freely available software, Meta-DiSc (version 1.4), was used to
perform the heterogeneity test, assessment of threshold effect,
pooling of diagnostic performance, and the meta-regression and
subgroup analyses (29).
The possible existence of publication bias was
visually assessed with the Deeks' funnel plot and asymmetry test,
using Stata software (version 12.0; StataCorp LP, College Station,
TX, USA). An inverted symmetrical funnel plot with P>0.05 was
considered to indicate the absence of publication bias (30).
Results
Included studies
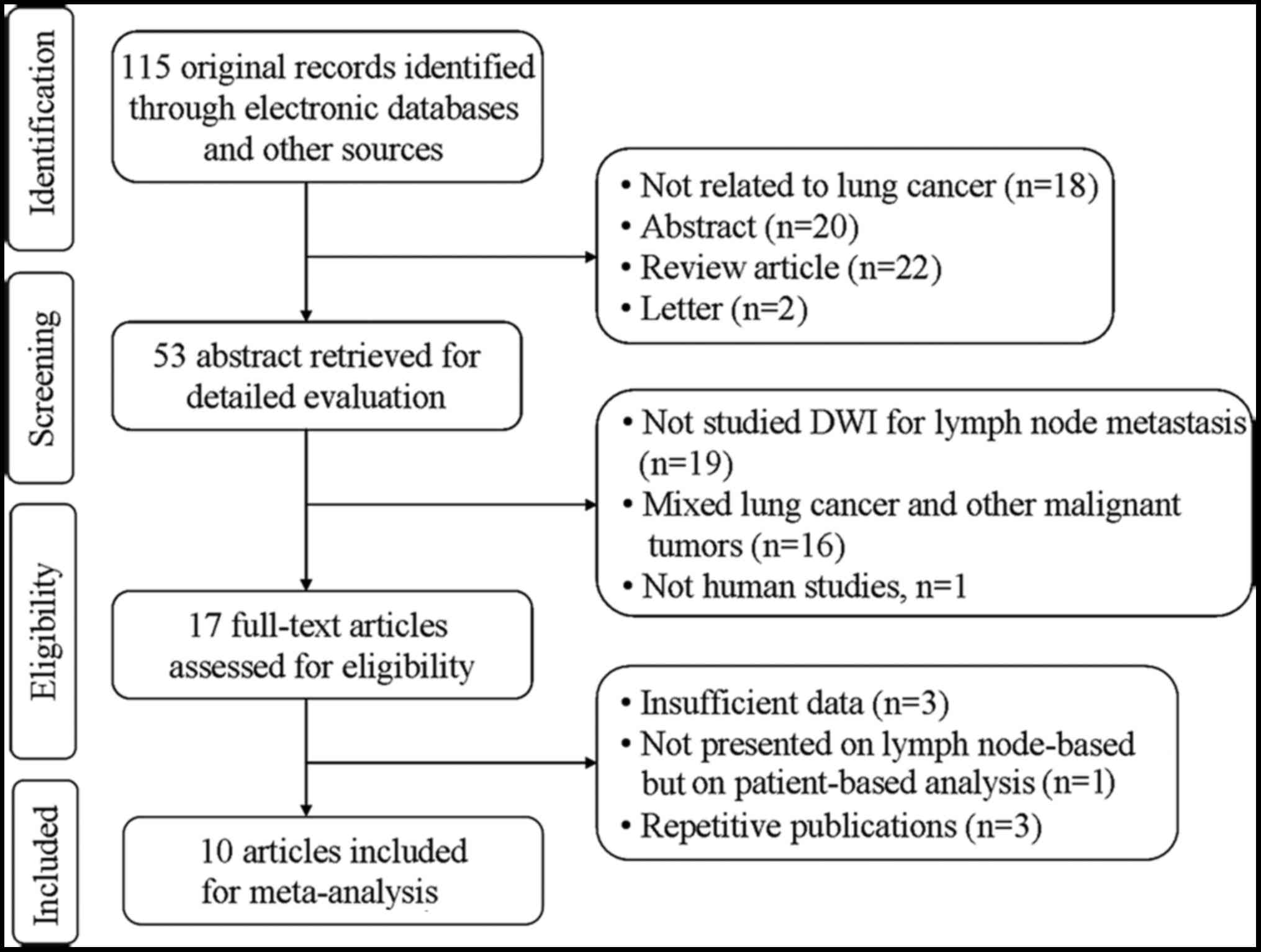
The search strategy initially yielded 115 studies,
of which 10 studies (11,14–22) with
11 datasets met the inclusion criteria, including 796 patients (472
male and 324 female; mean age, 66.3 years) with a total of 2,433
lymph nodes. In one study (15), the
analyses were performed based on normal-sized lymph nodes and
enlarged lymph nodes, respectively. Thus, that study was regarding
as comprising two unique datasets, which were included
independently in the present meta-analysis. The detailed flowchart
of the study selection process is shown in Fig. 1, and the characteristics of the
included studies are summarized in Table
I.
 | Table I.Characteristics of the included
studies in the meta-analysis. |
Table I.
Characteristics of the included
studies in the meta-analysis.
| Study ID | First author | Year | Age
(range/average) | Gender (M/F) | Study
sizea | Type of lung
cancer | Design | Patient
enrollment | Blind | Reference
standard | B-value
(s/mm2) | DT of ADC
(mm2/s) | Field strength | Type of
scanner | Refs. |
|---|
| 1 | Chen | 2010 | 35–76/51 | 35/21 | 56/135 | NSCLC | UN | Cons | Yes | Pathology and/or
follow-up | 1,000 | UN | 1.5 T | Siemens | (14) |
| 2 | Nakayama | 2010 | 48–82/68 | 38/32 | 70/56 | NSCLC | Retro | UN | UN | Pathology | 1,000 |
1.54×10−3 | 1.5 T | Siemens | (20) |
| 3 | Nomori | 2008 | 38–82/70 | 47/41 | 88/734 | NSCLC | Pros | UN | UN | Pathology | 1,000 |
1.60×10−3 | 1.5 T | Phillips | (11) |
| 4 | Usuda | 2013 | 37–83/68 | 94/64 | 158/705 | Lung cancer | UN | UN | UN | Pathology | 800 |
1.70×10−3 | 1.5 T | Siemens | (18) |
| 5 | Xu (ELN) | 2014 | 42–78/55 | 27/15 | 42/33 | NSCLC | Pros | Cons | Yes | Pathology | 1,000 |
1.98×10−3 | 1.5 T | Phillips | (15) |
| 6 | Xu (NLN) | 2014 | 42–78/55 | 27/15 | 42/86 | NSCLC | Pros | Cons | Yes | Pathology | 1,000 |
2.04×10−3 | 1.5 T | Phillips | (15) |
| 7 | Ohno | 2011 | 61–83/73 | 136/114 | 250/270 | NSCLC | Pros | Cons | Yes | Pathology | 1,000 |
2.50×10−3 | 1.5 T | Phillips | (19) |
| 8 | Bai | 2013 | 27–72/59 | 16/10 | 26/62 | NSCLC | UN | UN | UN | Pathology and/or
follow-up | 600 |
1.92×10−3 | 1.5 T | Phillips | (21) |
| 9 | He | 2013 | 33–77/58 | 27/9 | 36/206 | Lung cancer | UN | UN | UN | Pathology | 500 |
3.19×10−3 | 1.5 T | GE | (16) |
| 10 | Zhang | 2013 | 41–72/59 | 17/8 | 25/78 | NSCLC | UN | UN | Yes | Pathology | 800 |
2.21×10−3 | 3.0 T | Siemens | (17) |
| 11 | Zeng | 2012 | 48–69/58 | 35/10 | 45/68 | NSCLC | UN | UN | Yes | Pathology | 600 |
2.32×10−3 | 1.5 T | GE | (22) |
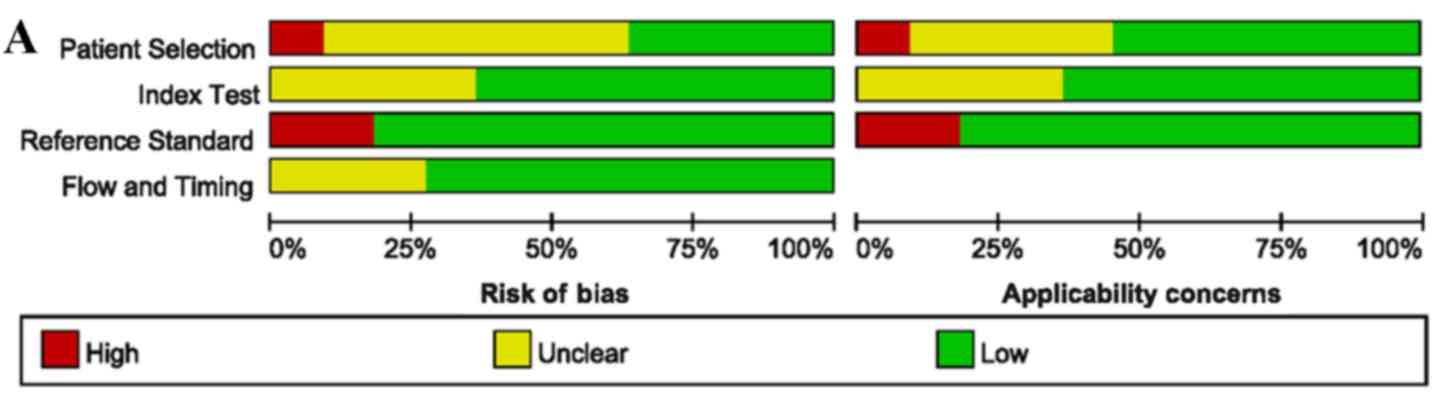
Assessment of study quality and
publication bias
The quality assessment of the included studies was
moderate according to the QUADAS-2 tool, and the results are shown
in Fig. 2. The Deeks' funnel plot
asymmetry tests revealed no strong evidence for the presence of
publication bias (bias=−0.15, P=0.887).
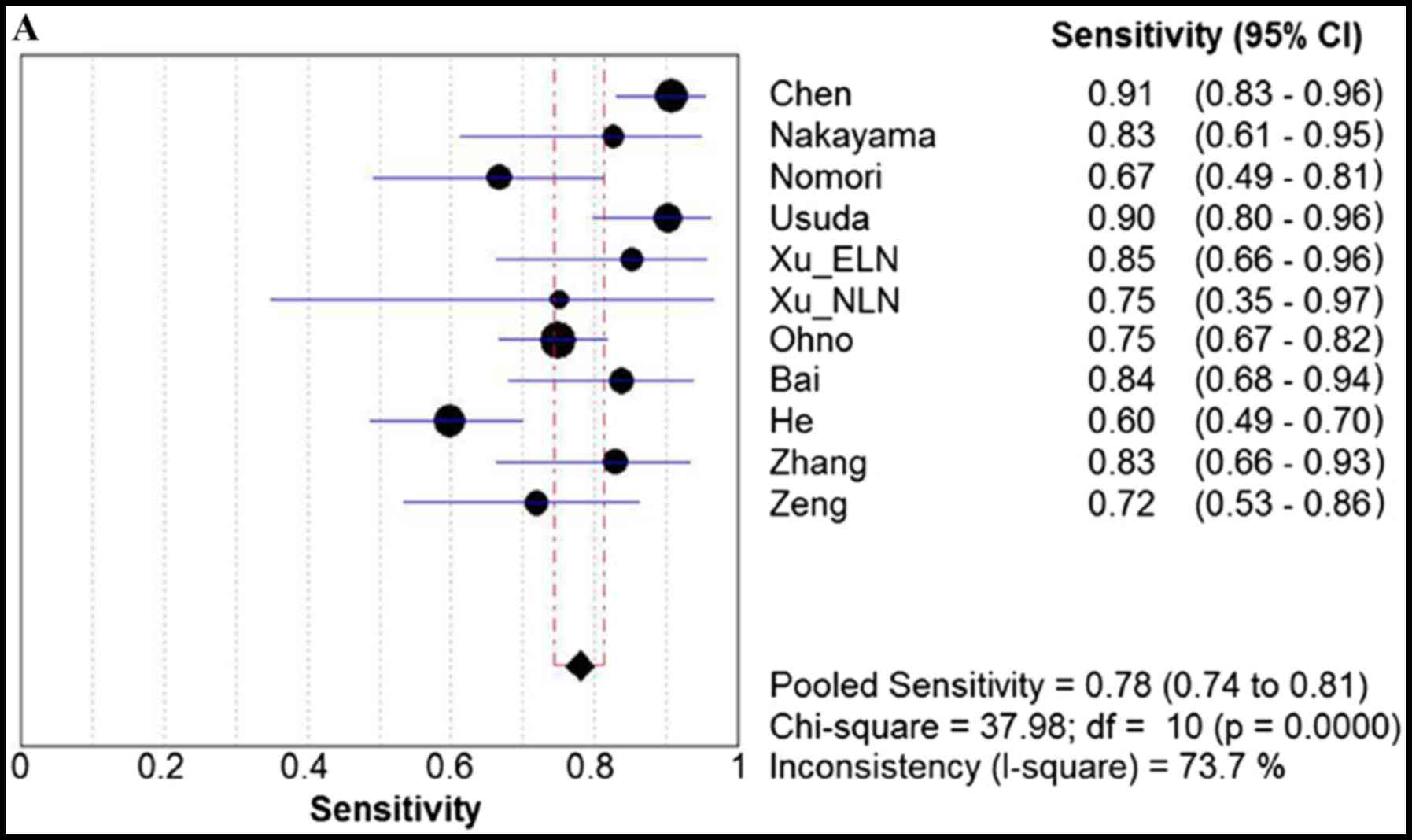
Homogeneity tests and threshold effect
analysis
Homogeneity tests demonstrated significant evidence
of heterogeneity for sensitivity (I2=73.7%,
P<0.0001), specificity (I2=95.2%, P<0.0001), PLR
(I2=86.0%, P<0.0001), NLR (I2=68.6%,
P=0.0004), and DOR (I2=66.1%, P=0.0010). The typical
pattern of a ‘shoulder-arm’ shape in the ROC plane was not
identified. Furthermore, Spearman's correlation coefficient, a
further test for the threshold effect, was calculated to be 0.209
(P=0.537), which indicated that no threshold effect existed.
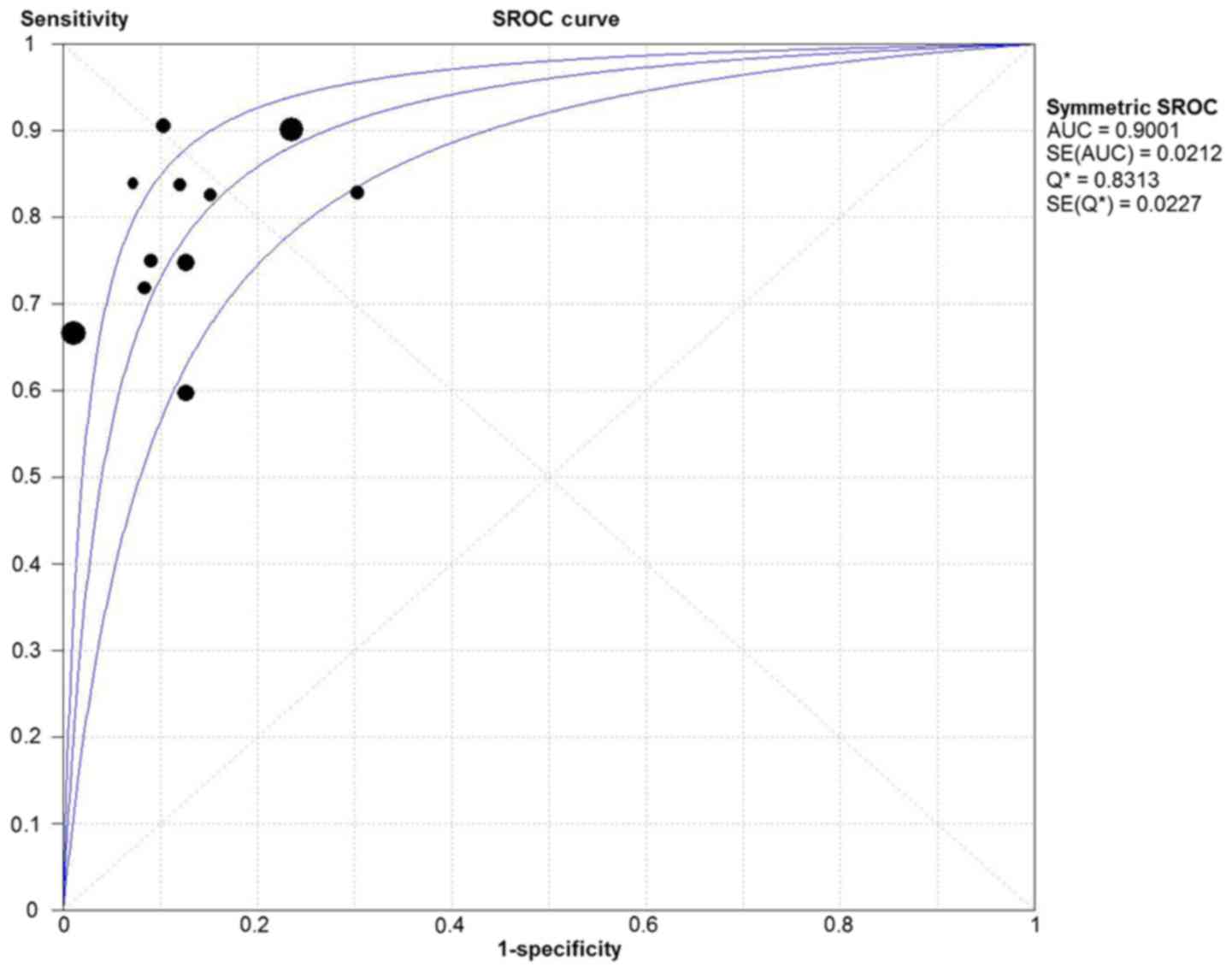
Diagnostic accuracy of DWI
Due to the notable heterogeneity among the included
studies, pooled values were determined using a random-effects model
analysis. The pooled diagnostic sensitivity was 0.78 (95% CI:
0.74–0.81), and the pooled diagnostic specificity was 0.88 (95% CI:
0.86–0.89). The PLR, NLR, and DOR were 7.11 (95% CI: 4.39–11.52),
0.24 (95% CI: 0.18–0.33), and 31.14 (95% CI: 17.32–55.98),
respectively. The forest plots for the included studies are shown
in Fig. 3. The SROC curve showed
that the Q value was 0.83, while the AUC was 0.90, suggesting good
diagnostic performance. The SROC curve is shown in Fig. 4.
Meta-regression and subgroup
analysis
Meta-regression analysis was subsequently performed
to explore other sources (except for threshold effect) of
heterogeneity. The results revealed that patient selection, type of
lung cancer, number of enrolled lymph nodes, reference standard,
B-value and type of scanner were the sources of heterogeneity
(P<0.05). Study design, blinding to all items of information
concerning the other test results, and field strength did not
statistically contribute to the heterogeneity. Table II shows the detailed results of the
meta-regression analysis. The subgroup analysis was performed for
the above-identified variables whose sample size was not <5
datasets. As the sample sizes of consecutive patient selection
(only 4 datasets), the type including small cell lung cancer and
reference standard of pathology and follow-up (only 2 datasets)
were too small to conduct subgroup analysis, only subgroup analysis
of NSCLC and the reference standard of pathology were performed
among the three variables. The results of subgroup analysis of
NSCLC and B-value equal to 1,000 demonstrated the highest
diagnostic performance for pooled sensitivity, specificity and DOR.
The results of the subgroup analysis are shown in Table III.
 | Table II.Results of meta-regression
analysis. |
Table II.
Results of meta-regression
analysis.
| Variable | Coefficient | Standard error | P-value | RDOR | 95% CI |
|---|
| Design | −0.629 | 0.5875 | 0.3630 | 0.53 | 0.08–3.46 |
| Patient
selection | −1.824 | 0.5447 | 0.0154 | 0.16 | 0.04–0.61 |
| Blind | −1.455 | 1.0608 | 0.2420 | 0.23 | 0.01–4.44 |
| Reference
standard | −1.752 | 0.5831 | 0.0239 | 0.17 | 0.04–0.72 |
| Type of lung
cancer | 1.270 | 0.4376 | 0.0198 | 3.56 | 1.30–9.76 |
| Study
sizea | 0.003 | 0.0008 | 0.0138 | 1.00 | 1.00–1.00 |
| B-value | 0.007 | 0.0016 | 0.0050 | 1.01 | 1.00–1.01 |
| DT of ADC | −4.786 | 2.0793 | 0.0828 | 0.01 | 0.00–2.68 |
| Type of
scanner | 0.970 | 0.3630 | 0.0442 | 2.64 | 1.04–6.71 |
| Field strength | −0.853 | 0.4270 | 0.0926 | 0.43 | 0.15–1.21 |
 | Table III.Results of subgroup analysis for DWI
in detecting lymph node metastasis. |
Table III.
Results of subgroup analysis for DWI
in detecting lymph node metastasis.
|
|
| Pooled
sensitivity | Pooled
specificity | DOR |
|---|
|
|
|
|
|
|
|---|
|
| No. of studies | Value (95% CI) | I2 | Value (95% CI) | I2 | Value (95% CI) | I2 |
|---|
| Totala | 11 | 0.78
(0.74–0.81) | 73.0 | 0.88
(0.86–0.89) | 95.2 | 31.14
(17.32–55.98) | 66.1 |
| Type of lung
cancer |
|
|
|
|
|
|
|
|
NSCLC | 9 | 0.80b (0.76–0.85) | 50.5c | 0.95b (0.93–0.96) | 90.7c | 37.71b (19.03–74.78) | 61.6c |
| Study
sized |
|
|
|
|
|
|
|
|
≥100 | 5 | 0.77
(0.73–0.81) | 88.4 | 0.88
(0.87–0.90) | 97.9 | 37.66b (14.17–100.07) | 85.0 |
|
<100 | 6 | 0.81b (0.74–0.87) | 0.0c | 0.86
(0.81–0.90) | 59.5c | 22.96
(12.49–42.23) | 0.0c |
| Reference
standard |
|
|
|
|
|
|
|
|
Pathology | 9 | 0.75
(0.71–0.79) | 66.5c | 0.88
(0.86–0.89) | 96.1 | 27.46
(14.30–52.71) | 68.7 |
| B-value |
|
|
|
|
|
|
|
|
1,000 | 6 | 0.80b (0.75–0.84) | 65.3c | 0.96b (0.95–0.97) | 90.6c | 50.73b (19.91–129.26) | 68.9 |
|
<1,000 | 5 | 0.75
(0.70–0.81) | 81.7 | 0.79
(0.76–0.81) | 74.3c | 18.04
(10.31–31.55) | 32.1c |
| Type of
scanner |
|
|
|
|
|
|
|
|
Phillips | 5 | 0.76
(0.70–0.81) | 9.7c | 0.96b (0.95–0.98) | 91.4c | 48.84b (15.90–149.98) | 72.5 |
| Siemens
and GE | 6 | 0.79b (0.75–0.84) | 84.7 | 0.79
(0.76–0.82) | 72.5c | 22.54
(11.80–43.06) | 54.8c |
Discussion
The presence of lymph node metastasis in patients
with lung cancer has been demonstrated to be a pivotal prognostic
factor for cancer staging and the outcome in these patients
(31–33). A number of studies have indicated
that DWI is a promising technique to distinguish metastatic from
non-metastatic lymph nodes (11,14,15,20). In
the present study, the diagnostic performance of DWI in detecting
metastatic lymph nodes of lung cancer was investigated. The results
revealed that, for lymph node metastasis detection, DWI had
relatively low sensitivity (78%) and high specificity (88%). The
SROC curve presents a global summary of test performance, and
displays the trade-off between sensitivity and specificity
(34–36). The AUC was revealed to be 0.90, which
indicated a good diagnostic ability. The DOR derived from different
combinations of sensitivity and specificity is the ratio of the
odds of positivity in the diseased state relative to the odds of
positivity in the non-diseased state, and may be used as a single
summary measure. The value of a DOR ranges from 0 to infinity, and
the greater it is, the better it is able to distinguish test
performance (23,37). In the present study, it was
identified that the DOR for DWI in detecting metastatic lymph nodes
of lung cancer was 31.14 (95% CI: 17.32–55.98), which also
indicated high overall diagnostic accuracy.
In clinical practice, it is necessary to know how a
diagnostic test result predicts the risk of abnormality. The
likelihood ratio (LR) is generally considered to be one of the best
measures of diagnostic accuracy, and is even more helpful for
decision-making in clinical practice compared with measures of
sensitivity, specificity or the AUC (24). An LR >1 is indicative of the fact
that the test result is associated with the presence of the
disease, whereas, by contrast, an LR <1 indicates that the test
result is associated with the absence of disease. The more that the
LR deviates from a value of 1, the stronger is the proof for either
the presence or absence of disease (38). A higher PLR lends itself to a ruling
in favor of a disease, whereas a lower NLR would lend itself to
ruling out the possibility of disease. In order to be moderately
useful, a diagnostic test should have a higher PLR value (>5)
and a lower NLR value (<0.2) (39). In the present study, the pooled PLR
and NLR were 7.11 and 0.24, respectively, which demonstrated that
DWI had a moderately good diagnostic performance for ruling in
cases of lymph node metastasis in patients with lung cancer, but a
relatively inferior diagnostic ability for ruling out
non-metastatic lymph nodes. Therefore, a lung cancer patient with
lymph node metastasis was 7.11 times more likely to have a positive
DWI manifestation compared with a patient without lymph node
metastasis. Analogously, the probability of having a negative DWI
manifestation for lymph node metastasis in patients with lung
cancer was 0.24 times (or approximately one-fourth) that of those
without lymph node metastasis. In other words, non-metastatic lymph
nodes were approximately 4 times more likely to have a negative DWI
manifestation compared with metastatic lymph nodes in patients with
lung cancer. Owing to the larger number of the included studies in
the present meta-analysis, these results were not entirely
consistent with previous studies (23,24).
However, the results in the present study do circumvent several of
the limitations that were acknowledged in previous studies, and
provide objective and practical suggestions for DWI in the
evaluation of lymph node status in patients with lung cancer.
Significant heterogeneity between the included
studies was identified in the present meta-analysis. Exploring the
sources of heterogeneity, which is useful in order to understand
the potential factors that influence accuracy assessments of the
pooled diagnostic performance, is an important aim of meta-analysis
(40,41). In the present study, the threshold
effect was assessed using the ROC plane and Spearman's correlation
coefficient. As indicated by the results of threshold effect
analysis, there was no threshold effect, and therefore the
heterogeneity may have been caused by other factors, for example,
the study characteristics. Thus, meta-regression analysis was
performed to further explore the sources of heterogeneity. The
results demonstrated that patient selection, the type of lung
cancer, the number of enrolled lymph nodes, the reference standard,
B-value and type of scanner were strongly associated with
diagnostic accuracy. In the subgroup analysis based on the type of
lung cancer and the B-value, the results of the subgroup analysis
of NSCLC and the B-value equal to 1,000 demonstrated the highest
diagnostic performance for pooled sensitivity, specificity and DOR.
The results further verified that the type of lung cancer involved
and the B-value are able to affect the diagnostic accuracy of DWI,
and therefore, the heterogeneity in these studies was increased. In
the present study, the two studies did not distinguish the type of
lung cancer, i.e. they did not differentiate NSCLC from small-cell
lung carcinoma. Previous studies have revealed that the mean ADC
value of small-cell carcinoma is significantly different from that
of NSCLC (42,43). In addition, the selection of the
B-value is particularly important for DWI. At lower B-values, with
<600 sec/mm2, signals are prominently influenced by
perfusion effects. Thus, their ADC values may not reflect diffusion
phenomena alone. To prevent perfusion effects, it is necessary to
use higher B-values. However, the higher the B-value, the greater
is the chance of distortion and susceptibility artifacts occurring
(44,45). The present study revealed that
different B-values contributed to adding to the heterogeneity, and
studies of the B-value equal to 1,000 had the best diagnostic
performance. These findings are helpful for the clinical
application of DWI in detecting lymph node metastasis of lung
cancer.
Although the present meta-analysis has produced a
more robust assessment of the true effect-size, with less random
error compared with individual studies, it should be recognized
that our study had several limitations. First, although no
publication bias was found in our meta-analysis, publication bias
may potentially still exist. The present meta-analysis was based
exclusively on published studies, and a grey literature search
analysis was not performed, which may have led to an overestimation
of the true effect. Additionally, the present study only included
previously published studies that were written in English or
Chinese, which may also have introduced unavoidable inclusion bias.
However, this bias would have been likely to have been small, since
the majority of studies of high quality were published in English.
Secondly, there was a notable heterogeneity among the included
studies. Although meta-regression analysis was adopted to explore
the sources of heterogeneity, the analysis of heterogeneity may
still have been insufficient. The optimal acquisition protocol of
DWI has not been defined, and differences attributable to the
different manufacturer of the MRI scanner, magnetic field strengths
and parameters used in DWI series are capable of affecting the
quality of DWI. In the present study, meta-regression analysis and
subgroup analysis were utilized to identify variables that may be
responsible for the heterogeneity. However, it is impossible to
perform meta-regression and subgroup analyses for all variables,
due to the excessive number of factors that are involved in the
processes of DWI. Therefore, it is necessary to further develop a
standard acquisition protocol of DWI as a routine clinical
application. Thirdly, among the included studies, there were
numerous non-prospective studies, and certain of the studies were
designed without a declaration of DWI reviewer-blinding to all
items of information concerning the results of other examinations.
Furthermore, the reference standards used in two included studies
were pathology and/or clinical follow-up, and these studies did not
report the exact number of metastatic lymph nodes that had been
diagnosed by pathology or follow-up. A reference standard based on
clinical follow-up can lead to inaccuracies in the sensitivities or
specificities provided by that study, and therefore the credibility
of the results is reduced.
In conclusion, our meta-analysis has demonstrated
that DWI is a valuable MRI modality, with good diagnostic
performance for distinguishing metastatic from non-metastatic lymph
nodes in patients with lung cancer. Therefore, DWI has been shown
to be a useful supplement to conventional MRI techniques. In the
future, larger-scale prospective studies with respect to DWI for
the diagnosis of lymph node metastasis will be required to evaluate
and confirm its clinical value. Furthermore, optimization of the
DWI acquisition protocol, standard image processing and analysis
are crucial for the routine clinical application of DWI in
detecting lymph node metastasis in patients with lung cancer.
Acknowledgements
The present study was supported by the National
Natural Science Foundation of China (grant no. 81541090) and the
Joined Foundation of Luzhou Municipal Government and Southwest
Medical University [2015LZCYD-S04 (9/15)].
References
|
1
|
Jemal A, Bray F, Center MM, Ferlay J, Ward
E and Forman D: Global cancer statistics. CA Cancer J Clin.
61:69–90. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Jemal A, Siegel R, Xu J and Ward E: Cancer
statistics, 2010. CA Cancer J Clin. 60:277–300. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Kligerman S and Digumarthy S: Staging of
non-small cell lung cancer using integrated PET/CT. AJR Am J
Roentgenol. 193:1203–1211. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
De Wever W: Role of integrated PET/CT in
the staging of non-small cell lung cancer. JBR-BTR. 92:124–126.
2009.PubMed/NCBI
|
|
5
|
Pauls S, Schmidt SA, Juchems MS, Klass O,
Luster M, Reske SN, Brambs HJ and Feuerlein S: Diffusion-weighted
MR imaging in comparison to integrated [18F]-FDG PET/CT
for N-staging in patients with lung cancer. Eur J Radiol.
81:178–182. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Kim YN, Yi CA, Lee KS, Kwon OJ, Lee HY,
Kim BT, Choi JY, Kim SW, Chung MP, Han J, et al: A proposal for
combined MRI and PET/CT interpretation criteria for preoperative
nodal staging in non-small-cell lung cancer. Eur Radiol.
22:1537–1546. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Cheran SK, Nielsen ND and Patz EF Jr:
False-negative findings for primary lung tumors on FDG positron
emission tomography: Staging and prognostic implications. AJR Am J
Roentgenol. 182:1129–1132. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Shim SS, Lee KS, Kim BT, Choi JY, Chung MJ
and Lee EJ: Focal parenchymal lung lesions showing a potential of
false-positive and false-negative interpretations on integrated
PET/CT. AJR Am J Roentgenol. 186:639–648. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Usuda K, Zhao XT, Sagawa M, Aikawa H, Ueno
M, Tanaka M, Machida Y, Matoba M, Ueda Y and Sakuma T:
Diffusion-weighted imaging (DWI) signal intensity and distribution
represent the amount of cancer cells and their distribution in
primary lung cancer. Clin Imaging. 37:265–272. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Ohba Y, Nomori H, Mori T, Ikeda K, Shibata
H, Kobayashi H, Shiraishi S and Katahira K: Is diffusion-weighted
magnetic resonance imaging superior to positron emission tomography
with fludeoxyglucose F 18 in imaging non-small cell lung cancer? J
Thorac Cardiovasc Surg. 138:439–445. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Nomori H, Mori T, Ikeda K, Kawanaka K,
Shiraishi S, Katahira K and Yamashita Y: Diffusion-weighted
magnetic resonance imaging can be used in place of positron
emission tomography for N staging of non-small cell lung cancer
with fewer false-positive results. J Thorac Cardiovasc Surg.
135:816–822. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Nomori H, Cong Y, Abe M, Sugimura H and
Kato Y: Diffusion-weighted magnetic resonance imaging in
preoperative assessment of non-small cell lung cancer. J Thorac
Cardiovasc Surg. 149:991–996. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Koyama H, Ohno Y, Nishio M, Takenaka D,
Yoshikawa T, Matsumoto S, Seki S, Maniwa Y, Ito T, Nishimura Y and
Sugimura K: Diffusion-weighted imaging vs STIR turbo SE imaging:
Capability for quantitative differentiation of small-cell lung
cancer from non-small-cell lung cancer. Br J Radiol.
87:201303072014. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Chen W, Jian W, Li HT, Li C, Zhang YK, Xie
B, Zhou DQ, Dai YM, Lin Y, Lu M, et al: Whole-body
diffusion-weighted imaging vs. FDG-PET for the detection of
non-small-cell lung cancer. How do they measure up? Magn Reson
Imaging. 28:613–620. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Xu L, Tian J, Liu Y and Li C: Accuracy of
diffusion-weighted (DW) MRI with background signal suppression
(MR-DWIBS) in diagnosis of mediastinal lymph node metastasis of
nonsmall-cell lung cancer (NSCLC). J Magn Reson Imaging.
40:200–205. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
He W, Xu JP, Zhou XH, et al: Comparison of
CT and DWI in preoperative evaluation of chest lymph node status in
lung cancer. Journal of Clinical Radiology. 32:802–806. 2013.(In
Chinese).
|
|
17
|
Zhang X, Xing W and Chen J: Application of
DWI in differential diagnosis of lymph nodes in patients with lung
cancer. Chin Comput Med Imag. 19:213–216. 2013.(In Chinese).
|
|
18
|
Usuda K, Sagawa M, Motono N, Ueno M,
Tanaka M, Machida Y, Matoba M, Kuginuki Y, Taniguchi M, Ueda Y and
Sakuma T: Advantages of diffusion-weighted imaging over positron
emission tomography-computed tomography in assessment of hilar and
mediastinal lymph node in lung cancer. Ann Surg Oncol.
20:1676–1683. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Ohno Y, Koyama H, Yoshikawa T, Nishio M,
Aoyama N, Onishi Y, Takenaka D, Matsumoto S, Maniwa Y and Nishio W:
N stage disease in patients with non-small cell lung cancer:
Efficacy of quantitative and qualitative assessment with STIR turbo
spin-echo imaging, diffusion-weighted MR imaging, and
fluorodeoxyglucose PET/CT. Radiology. 261:605–615. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Nakayama J, Miyasaka K, Omatsu T, Onodera
Y, Terae S, Matsuno Y, Cho Y, Hida Y, Kaga K and Shirato H:
Metastases in mediastinal and hilar lymph nodes in patients with
non-small cell lung cancer: Quantitative assessment with
diffusion-weighted magnetic resonance imaging and apparent
diffusion coefficient. J Comput Assist Tomogr. 34:1–8. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Bai CG, Zhang XM and Qiao W: Application
of apparent diffusion coefficient in evaluating lymphatic
metastasis of non-small cell lung cancer. Jiangsu Med J.
39:2977–2979. 2013.(In Chinese).
|
|
22
|
Zeng Z, Liao Q, Cai J and Liu A:
Diffusion-weighted imaging and apparent diffusion coefficient
values in the differential diagnosis of hilar and mediastinal lymph
nodes of non-small cell lung cancer. Chinese Journal of Clinical
Oncology. 39:706–710. 2012.(In Chinese).
|
|
23
|
Wu LM, Xu JR, Gu HY, Hua J, Chen J, Zhang
W, Haacke EM and Hu J: Preoperative mediastinal and hilar nodal
staging with diffusion-weighted magnetic resonance imaging and
fluorodeoxyglucose positron emission tomography/computed tomography
in patients with non-small-cell lung cancer: Which is better? J
Surg Res. 178:304–314. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Zhou M, Lu B, Lv G, Tang Q, Zhu J, Li J
and Shi K: Differential diagnosis between metastatic and
non-metastatic lymph nodes using DW-MRI: A meta-analysis of
diagnostic accuracy studies. J Cancer Res Clin Oncol.
141:1119–1130. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Whiting PF, Rutjes AW, Westwood ME,
Mallett S, Deeks JJ, Reitsma JB, Leeflang MM, Sterne JA and Bossuyt
PM: QUADAS-2 Group: QUADAS-2: A revised tool for the quality
assessment of diagnostic accuracy studies. Ann Intern Med.
155:529–536. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Higgins JP and Thompson SG: Quantifying
heterogeneity in a meta-analysis. Stat Med. 21:1539–1558. 2002.
View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Chen LH, Zhang J, Bao J, Zhang L, Hu X,
Xia Y and Wang J: Meta-analysis of diffusion-weighted MRI in the
differential diagnosis of lung lesions. J Magn Reson Imaging.
37:1351–1358. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Arends LR, Hamza TH, van Houwelingen JC,
Heijenbrok-Kal MH, Hunink MG and Stijnen T: Bivariate random
effects meta-analysis of ROC curves. Med Decis Making. 28:621–638.
2008. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Zamora J, Abraira V, Muriel A, Khan K and
Coomarasamy A: Meta-DiSc: A software for meta-analysis of test
accuracy data. BMC Med Res Methodol. 6:312006. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Song F, Khan KS, Dinnes J and Sutton AJ:
Asymmetric funnel plots and publication bias in meta-analyses of
diagnostic accuracy. Int J Epidemiol. 31:88–95. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Herneth AM, Mayerhoefer M, Schernthaner R,
Ba-Ssalamah A, Czerny Ch and Fruehwald-Pallamar J: Diffusion
weighted imaging: Lymph nodes. Eur J Radiol. 76:398–406. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Harders SW, Madsen HH, Hjorthaug K,
Arveschoug AK, Rasmussen TR, Meldgaard P, Hoejbjerg JA, Pilegaard
HK, Hager H, Rehling M and Rasmussen F: Mediastinal staging in
non-small-cell lung carcinoma: Computed tomography versus
F-18-fluorodeoxyglucose positron-emission tomography and computed
tomography. Cancer Imaging. 14:232014.PubMed/NCBI
|
|
33
|
Al-Sarraf N, Gately K, Lucey J, Wilson L,
McGovern E and Young V: Lymph node staging by means of positron
emission tomography is less accurate in non-small cell lung cancer
patients with enlarged lymph nodes: Analysis of 1,145 lymph nodes.
Lung Cancer. 60:62–68. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Wu LM, Xu JR, Hua J, Gu HY, Chen J, Haacke
EM and Hu J: Can diffusion-weighted imaging be used as a reliable
sequence in the detection of malignant pulmonary nodules and
masses? Magn Reson Imaging. 31:235–246. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Harbord RM, Deeks JJ, Egger M, Whiting P
and Sterne JA: A unification of models for meta-analysis of
diagnostic accuracy studies. Biostatistics. 8:239–251. 2007.
View Article : Google Scholar : PubMed/NCBI
|
|
36
|
Rutter CM and Gatsonis CA: A hierarchical
regression approach to meta-analysis of diagnostic test accuracy
evaluations. Stat Med. 20:2865–2884. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
37
|
Glas AS, Lijmer JG, Prins MH, Bonsel GJ
and Bossuyt PM: The diagnostic odds ratio: A single indicator of
test performance. J Clin Epidemiol. 56:1129–1135. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
38
|
Deeks JJ and Altman DG: Diagnostic tests
4: Likelihood ratios. BMJ. 329:168–169. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
39
|
Cronin P, Dwamena BA, Kelly AM, Bernstein
SJ and Carlos RC: Solitary pulmonary nodules and masses: A
meta-analysis of the diagnostic utility of alternative imaging
tests. Eur Radiol. 18:1840–1856. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
40
|
Naaktgeboren CA, van Enst WA, Ochodo EA,
de Groot JA, Hooft L, Leeflang MM, Bossuyt PM, Moons KG and Reitsma
JB: Systematic overview finds variation in approaches to
investigating and reporting on sources of heterogeneity in
systematic reviews of diagnostic studies. J Clin Epidemiol.
67:1200–1209. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
41
|
Lijmer JG, Bossuyt PM and Heisterkamp SH:
Exploring sources of heterogeneity in systematic reviews of
diagnostic tests. Stat Med. 21:1525–1537. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
42
|
Matoba M, Tonami H, Kondou T, Yokota H,
Higashi K, Toga H and Sakuma T: Lung carcinoma: Diffusion-weighted
MR imaging-preliminary evaluation with apparent diffusion
coefficient. Radiology. 243:570–577. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
43
|
Liu HD, Liu Y, Yu TL and Ye N: Usefulness
of diffusion-weighted MR imaging in the evaluation of pulmonary
lesions. Eur Radiol. 20:807–815. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
44
|
Jezzard P, Barnett AS and Pierpaoli C:
Characterization of and correction for eddy current artifacts in
echo planar diffusion imaging. Magn Reson Med. 39:801–812. 1998.
View Article : Google Scholar : PubMed/NCBI
|
|
45
|
Bastin ME: Correction of eddy
current-induced artefacts in diffusion tensor imaging using
iterative cross-correlation. Magn Reson Imaging. 17:1011–1024.
1999. View Article : Google Scholar : PubMed/NCBI
|