Introduction
Clear cell sarcoma of soft tissues (CCSST) was first
described by Enzinger in 1965 (1).
CCSST is a very rare, malignant soft tissue tumor and is often
referred to as ‘malignant melanoma of soft tissues’ due to the
histologic similarities and lack of observable pigmentation often
seen in cutaneous melanoma. Clinically, the majority of cases
present as a slowly progressive mass with a predilection for young
females (2). Patients with CCSST
have a variable unpredictable prognosis (3). The condition presents as a soft tissue
mass common to the tendons, and aponeurosis is observed in the
lower extremities and rarely presents in the trunk (2). The present study reports an unusual
case of CCSST in the right lumbar region. To the best of our
knowledge, this is the first case report that has been documented
in the English literature worldwide regarding CCSST in the right
lumbar region. Written informed consent was obtained from the
patient.
Case report
A 45-year-old male presented to our department with
a painless mass in the right lumbar region of one year. The patient
related that the mass had remained stable for 11 months, with no
pain or increase in size. One month prior to presenting at the
hospital, the patient reported that the mass had started to
enlarge, elicit pain and affect the general wellbeing of the
patient. The patient did not have personal or familiar history of
cutaneous malignancy. Magnetic resonance imaging identified a
3.6×3.2×1.5-cm soft tissue mass of the right lumbar region.
Physical examination revealed a subcutaneous
irregular firm mass in the right lumbar region region measuring
3.5×3.0 cm. There were no signs of superficial skin inflammation
and clinical examination did not reveal other relevant cutaneous
lesions.
An open biopsy was performed and the gross specimen
measured 3.5×3×1.2 cm. The gross specimen was described as a
gray-white, homogenous, rubbery tissue with no attachment to the
skin. Tumoral cells were arranged in sheets or small nests, and
were separated by connective tissue septa (Fig. 1). The cells had pleomorphic nuclei
and large amounts of clear cytoplasm, whereas the spindle-shaped
cells had palely stained eosinophilic cytoplasm. Patchy melanin
expression was observed (Fig. 2).
Mitoses were moderately numerous and there was no evidence of
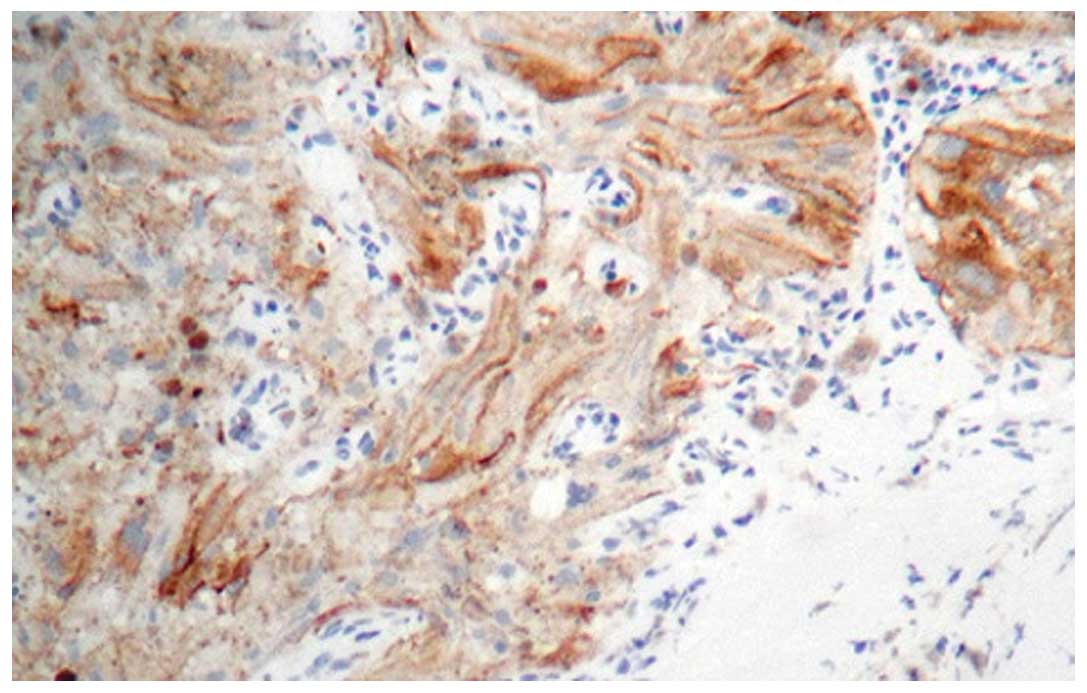
necrosis or hemorrhage. Immunohistochemical analysis indicated
positive staining for tumor markers S-100 (Fig. 3), MITF (Fig. 4) and HMB-45, and negative staining
for CD10, CD68, actin, desmin and AE1/AE3 antigens (data not
shown). The pathological findings were compatible with CCSST.
The patient was started on a postoperative
chemotherapy protocol. Radiotherapy was not administered, as
requested by the patient. The patient had no local recurrences at
the one year post-surgery follow-up and there were no complications
from the chemotherapy treatment.
Discussion
CCSST is currently a distinct entity classified, by
the World Health Organization, as soft tissue and bone tumors
(4). CCSST is a rare tumor
accounting for only a small percentage of soft tissue tumors. CCSST
is an aggressive soft tissue tumor with a long period from the
first symptom to diagnosis. The median age of patients at diagnosis
is 33 years (5). Clinically, CCSST
is most often present in young adults, with a slight female
bias.
Pain above the tumor site may be experienced in
33–50% of all the patients that suffer from CCSST. Primary CCSST
usually arises in deeper soft tissues, bound to an adjacent tendon
or aponeurosis (6). Frequently, it
arises in the extremities with a predilection for the lower limbs
(78–97%). The foot and ankle are the most common sites of tumor
appearance, accounting for 33–65% of all cases. The next most
common sites are the knee, thigh, hand, forearm, elbow and
shoulder, in descending order of frequency; tumors rarely arise in
the head, neck or trunk (7–10). Primary CCSST overlying the right
lumbar region, as in the present case, are uncommon.
Histologically, CCSST is composed of round and/or
fusiform cells that are arranged in nests and separated by
fibrocollagenous tissue. The cells have pleomorphic nuclei and
large amounts of clear cytoplasm, while the spindle-shaped cells
exhibit palely stained eosinophilic cytoplasm (5).
A small number of giant cells, with >12–15
nuclei, may be observed (11), but
there were no wreath-like giant cells in the presented case.
Melanosomes may be present, as detected at the ultrastructural
level (11). In the present case,
some cells were detected that contained melanin.
There are no specific immunoreactive markers used to
delineate clear cell sarcoma. S-100 and HMB-45 are often used to
differentiate clear cell sarcoma from epithelial tumors and
synovial sarcoma, and faint keratin immunoreactivity has been
observed in clear cell sarcoma (5).
More recently, molecular genetic characterization of clear cell
sarcoma has been shown to be specific for t(12;22) chromosomal
translocation, which is typically not present in cutaneous
malignant melanoma (MM) (12,13).
This translocation has not been observed in either cutaneous or
uveal MM or malignant peripheral nerve sheath tumors (MPNSTs+)
(14,15). A chromosomal study was not performed
in the present case due to practical constraints.
An important differential diagnosis is metastatic
MM. A possible source of a primary lesion must first be excluded
before making a diagnosis of CCSST (12). In contrast to MM, CCSST is situated
in deep tissues and is generally located in non-pigmented
areas.
Surgical resection, adjuvant radio- or chemotherapy
or a combination of these three treatments has no reported
significant advantage of one therapy over another (16), although a report has suggested that
metastatic tumors exhibit almost no response to systemic
chemotherapy (17). The described
patient underwent a surgical excision and chemotherapy, and was
healthy at the one-year follow-up.
Patients with CCSST have a variable unpredictable
course of the disease. Lymph node metastasis has been reported in a
high number of cases (12). The
other sites of metastases often include the lungs, skin, bones,
liver, heart and brain. Lymph node metastasis has a worse survival
rate (12) and it has been
hypothesized that the size of the tumor can define a better or
worse prognosis (16). Other
clinical and pathological factors have no significant association
to survival or distant metastasis when the tumor size is >5 cm.
In a study by Deenik et al (12), patients with a tumor size <2 cm
had an improved survival. Preoperative duration of symptoms,
mitotic index or vascular invasion may not predict survival in
these patients.
References
|
1
|
Enzinger FM: Clear-cell sarcoma of tendons
and aponeuroses: an analysis of 21 cases. Cancer. 18:1163–1174.
1965.
|
|
2
|
Weiss SW and Goldblum JR: Malignant nerve
sheath tumors. Enzinger and Weiss’s Soft Tissue Tumors. 5th
edition. Mosby; Maryland Heights, MO: pp. 926–934. 2008
|
|
3
|
Ferrari A, Casanova M, Bisogno G, et al:
Clear cell sarcoma of tendons and aponeuroses in pediatric
patients: a report from the Italian and German Soft Tissue Sarcoma
Cooperative Group. Cancer. 15:3269–3276. 2002.
|
|
4
|
Sciot R and Speleman F: Clear cell sarcoma
of soft tissue. In: Pathology and Genetics of Tumours of Soft
Tissue and Bone. WHO Classification of Tumours. Fletcher CDM, Unni
KK and Mertens F: IARC Press; Lyon: pp. 211–212. 2002
|
|
5
|
Hocar O, Le Cesne A, Berissi S, Terrier P,
et al: Clear cell sarcoma (malignant melanoma) of soft parts: a
clinicopathologic study of 52 cases. Dermatol Res Pract.
2012:9840962012.
|
|
6
|
Mentzel T: Uncommon variants of malignant
melanocytic neoplasms. Pathologe. 28:445–452. 2007.(In German).
|
|
7
|
Charhi H, Malihy A, Lamalmi N, Alhamany Z
and Cherradi N: Clear cell sarcoma of soft tissues: a case report.
Arch Pediatr Sep. 17:1304–1307. 2010.(In French).
|
|
8
|
Pavlidis NA, Fisher C and Wiltshaw E:
Clear-cell sarcoma of tendons and aponeuroses: a clinicopathologic
study. Presentation of six additional cases with review of the
literature. Cancer. 54:1412–1417. 1984.
|
|
9
|
Marquès B, Terrier P, Voigt JJ, Mihura J
and Coindre JM: Clear cell soft tissue sarcoma. Clinical,
histopathological and prognostic study of 36 cases. Ann Pathol.
20:298–303. 2000.(In French).
|
|
10
|
Kazakos CJ, Galanis VG, Giatromanolaki A,
Verettas DA and Sivridis E: Clear cell sarcoma of the scapula. A
case report and review of the literature. World J Surg Oncol.
4:482006.
|
|
11
|
Graadt van Roggen JF, Mooi WJ and
Hogendoorn PC: Clear cell sarcoma of tendon and aponeuroses
(malignant melanoma of soft parts) and cutaneous melanoma:
exploring the histogenetic relationship between these two
clinicopathological entities. J Pathol. 186:3–7. 1998.
|
|
12
|
Deenik W, Mooi WJ, Rutgers EJ, et al:
Clear cell sarcoma (malignant melanoma) of soft parts: A
clinicopathologic study of 30 cases. Cancer. 86:969–975. 1999.
|
|
13
|
Straessler KM, Jones KB, Hu H, et al:
Modeling clear cell sarcomagenesis in the mouse: cell of origin
differentiation state impacts tumor characteristics. Cancer Cell.
23:215–227. 2013.
|
|
14
|
Kawai A, Hosono A, Nakayama R, et al:
Clear cell sarcoma of tendons and aponeuroses: a study of 75
patients. Cancer. 109:109–116. 2007.
|
|
15
|
Hisaoka M, Ishida T, Kuo TT, et al: Clear
cell sarcoma of soft tissue: A clinicopathologic,
immunohistochemical, and molecular analysis of 33 cases. Am J Surg
Pathol. 32:452–460. 2008.
|
|
16
|
Sara AS, Evans HL and Benjamin RS:
Malignant melanoma of soft parts (clear cell sarcoma): A study of
17 cases with emphasis on prognostic factors. Cancer. 65:367–374.
1990.
|
|
17
|
Xu GG, Chong YL and Cheong MO: Clear cell
sarcoma of the rectus sheath. Singapore Med J. 48:e203–e205.
2007.
|