Introduction
Schwannoma (neurinoma or neurilemmoma) is a rare,
benign tumor, composed exclusively of Schwann cells, that arises
from the nerve sheath, as opposed to neurofibrome consisting of
different cell types that constitute the nerve. Schwannoma is the
most common tumor of the nerves and the incidence in adults is ~5%
(1). It is common in neurocutaneous
diseases as neurofibromatosis I; in neurofibromatosis II,
schwannoma involves typically eighth nerves. It is an encapsulated
lesion without an infiltrative behaviour; the lesion pushes the
nerve laterally, assuming an eccentric shape, usually <3 cm in
diameter. In this sense, malignant transformation is rare and
growth is slow. In some locations, schwannoma can reach a
considerable size, with degenerative features such as cyst,
fibrosis and calcification (2). In
the majority of cases, the tumor is identified incidentally and
involves the limbs, trunk, head and neck. Infrequently, it can
arise in any part of the body. Surgical excision is the treatment
of choice. The decision whether to operate depends on the degree of
the symptomatology and the location of the lesion. The balance
between the relief of pain and the potential neurological deficit
is a key point in the decision-making. Due to the low risk of
relapse and the exceptional malignant transformation, enucleation
is a surgical option (3). Partial
excision can be considered in order to avoid neurological
sequelae.
To the best of our knowledge, the present study is
the third reported case of a schwannoma located in the abdominal
wall, and the first symptomatic case (4,5).
Written informed consent was obtained from the patient.
Case Report
A 57-year-old woman presented to the surgical
outpatient department due to well-localized parietal pain in the
left lower quadrant. The onset of pain occurred three years prior
to presentation, without apparent cause and in the absence of other
symptoms. The pain was extremely localized, 6–7 cm inferiorly and
laterally to the umbilicus, and was not associated with movement,
position or particular events such as oral feeding and stress.
Overall, the symptomatology increased over time, in terms of
frequency and intensity of the abdominal pain. On physical
examination, the abdomen was not painful and no mass was identified
or suspected. All routine laboratory tests were normal. During the
first year of symptoms, a gastroenterological outpatient
consultation was performed and a colonoscopy procedure did not
reveal any lesions or abnormalities. During the same consultation,
an ultrasound examination was performed, notably revealing a
well-defined cystic lesion, 1.6 cm in diameter, located in the
muscular layer of the left-lower quadrant of the parietal wall. The
nodule was not painful upon the administration of pressure. Due to
the persistence of the symptoms, one year later an abdominal
computed tomography (CT) scan was performed. In a preliminary
analysis, no lesions were identified in the peritoneal cavity or
abdominal wall, and no parietal defects were found. Three years
subsequent to the onset of the symptoms, a novel analysis and
review of the radiological images revealed the presence of a small
parietal nodule. In order to confirm and verify the possible
alteration in the tumor, a novel CT scan was performed.
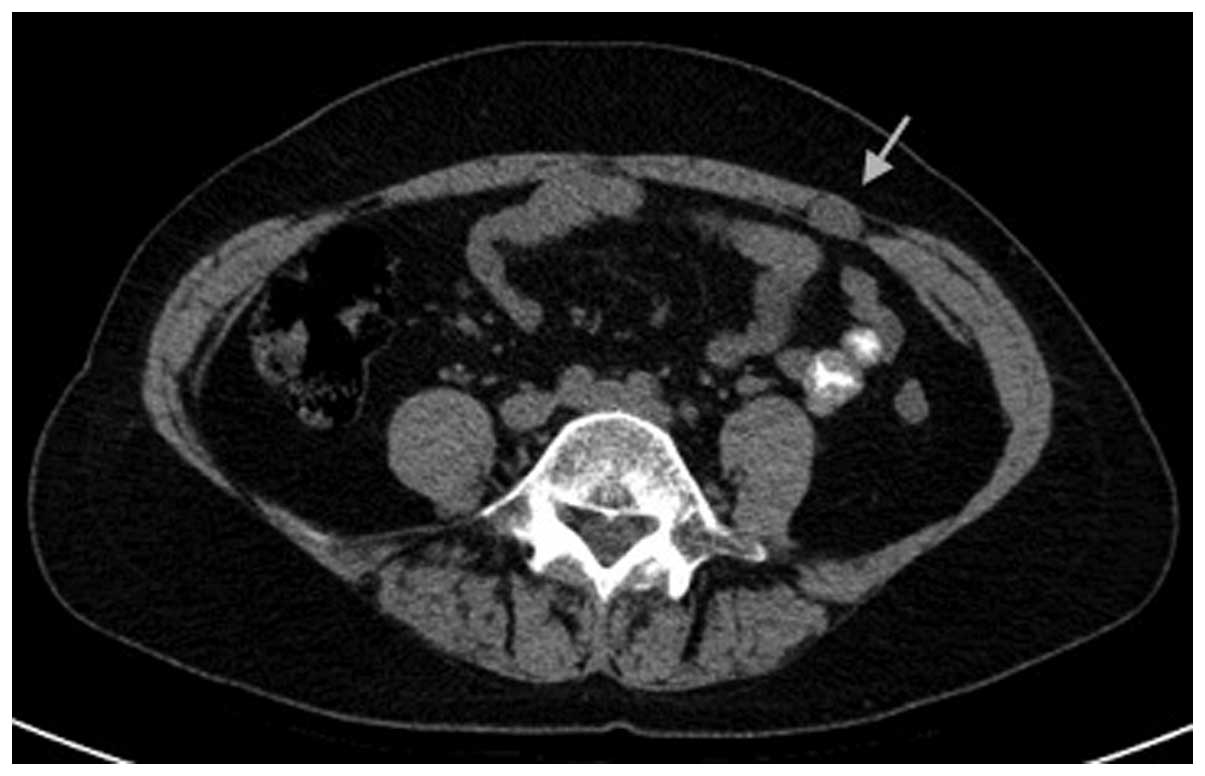
The CT scans were performed on a 16-channel
multislice unit (Brilliance 16p; Philips, Amsterdam, Netherlands)
and on a 256-channel multislice unit (iCT256; Philips) prior to and
following the administration of intravenous (IV) contrast media
with a two-year interval between the two examinations. A 17×11 mm
mass was identified in the abdominal wall, on the left edge of the
left rectus anterior muscle (Fig.
1). The mass exhibited a homogeneous soft mass density on basal
CT, with a regular oval shape. The IV administration of contrast
media for dynamic CT revealed a modest, homogeneous enhancement of
the lesion (Fig. 2). No difference
was identified between the first and second examinations.
The suspected diagnosis was of a benign schwannoma
of the anterior abdominal wall. The most notable indication of the
cause-effect association between the lesion and the parietal
abdominal pain was the considerable topographic coincidence.
Presented with this clear association, an indication for surgical
removal was discussed with the patient and decided by mutual
agreement.
A pre-operative ultrasound examination (Logiq E9
Ultrasound System; GE Healthcare Life Sciences, Chalfont, UK)
confirmed the size and shape of the mass, which was hypoechoic with
certain internal linear hyperechoic structures (Fig. 3).
The patient underwent surgery under general
anesthesia, which was performed using a direct anterior approach.
By making an incision into the anterior fascia of the left rectus
abdominis muscle, the lesion was immediately identified at the
lateral edge of the muscle (Fig.
4). Notably, a small parietal nerve entered and exited the
nodule in an eccentric manner. The tumor was completely
resected.
Macroscopically, the nodule was 2 cm in diameter,
rounded and of tense-elastic consistency, exhibiting a white color
in the center of the lesion and possessing a peripheral region of
myxoid appearance (Fig. 5).
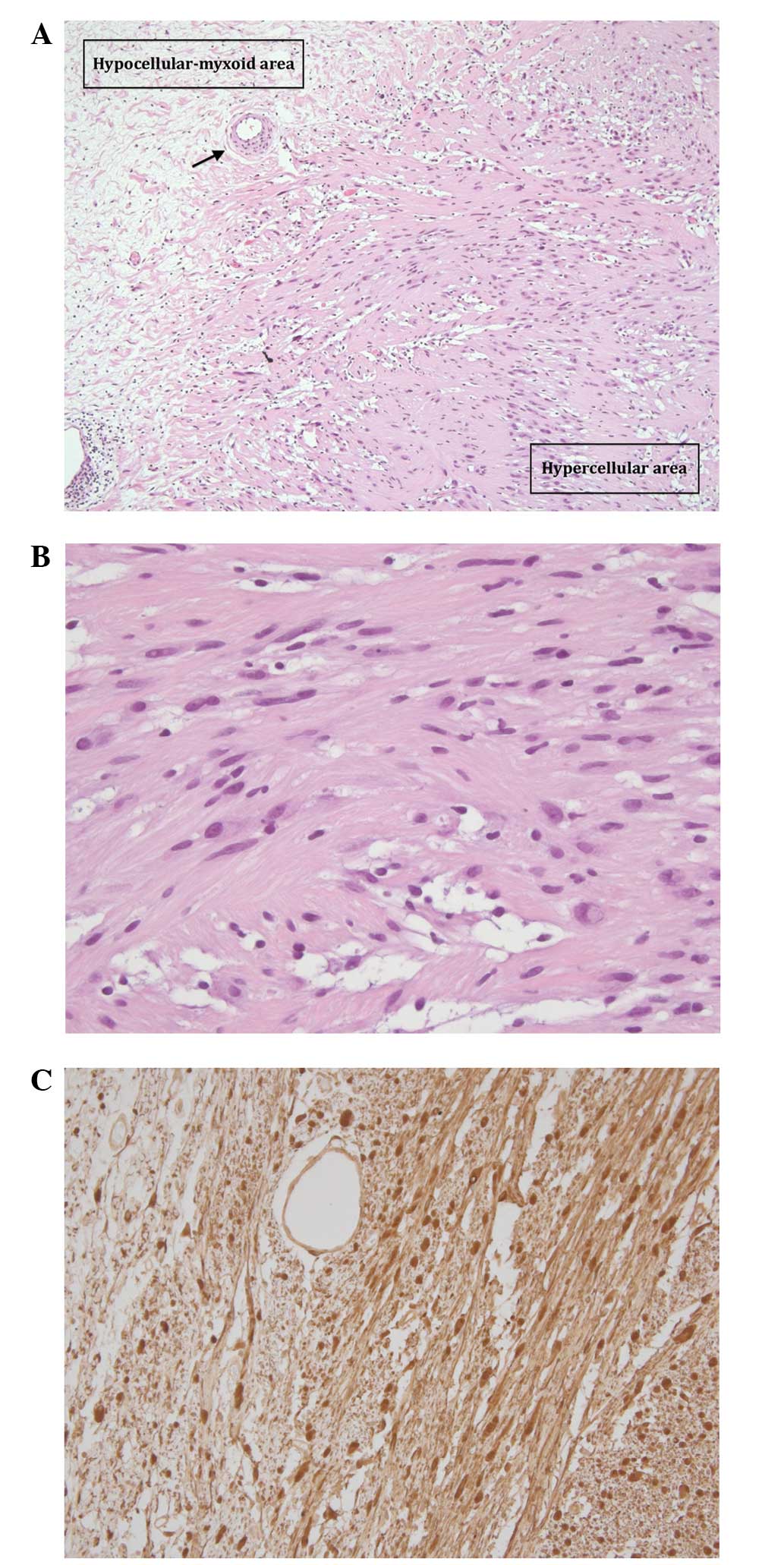
Microscopically, the lesion demonstrated an
alternation of hypercellular and hypocellular areas, each
comprising spindle cells without significant atypia. In the
hypocellular area, foci of myxoid differentiation were also
present. The tumor cells were revealed to strongly and diffusely
express the S-100 protein by immunohistochemistry (Fig. 6), confirming the diagnosis of benign
schwannoma. The post-operative course was uneventful and the
symptoms ceased completely. A one-year follow-up appointment did
not reveal any relapse of the symptoms.
Discussion
Schwannomas are benign tumors of the Schwann cells
in the neural sheath of cranial and peripheral nerves. The lesions
usually involve the extremities, but can also be found in the head
and neck, trunk, pelvis, retroperitoneum, mediastinum and
gastrointestinal tract. However, the tumors are extremely uncommon
in parenchymatous organs, such as the liver and pancreas (6). There is a female predominance and
schwannoma typically occurs between the ages of 20–50 years old
(7,8).
In numerous cases the schwannoma is asymptomatic and
is identified incidentally upon physical examination or imaging.
Occasionally, the tumors are symptomatic due to the compression of
surrounding large nerves (9).
To the best of our knowledge, only two cases of
benign schwannoma located in the abdominal wall have been reported
in the medical literature at present. In the first case (4), a healthy 64-year-old female underwent
a whole body CT scan, which revealed an incidental mass of 6 cm in
the right iliac fossa. The second study (5) reported the case of a 29-year-old
female who presented with a painless lump in the left-upper
abdomen, which had been gradually increasing in size over 10
months. The tumor was 6 cm in diameter and, notably, the tumor was
located between the rectus abdominis muscle and the lateral
abdominal muscle, which is identical to the tumor location in the
present patient. In the two cases, a histopathological diagnosis of
benign ancient schwannoma was made.
Ancient schwannoma is a sub-type of schwannoma
characterized by degenerative changes that are observed under
microscopy (10). These changes are
the result of long-term progression (11). In the present case, the symptomatic
behavior of the lesion, which was characterized by persistent pain
of the abdominal wall, may explain the early diagnosis of a
schwannoma that was small in size and, accordingly, lacked
degenerative changes.
As in the present patient, the identification of a
nerve entering and exiting a mass is pathognomonic for a peripheral
nerve sheath tumor and the eccentric association with the nerve is
considered to be pathognomonic for a schwannoma rather then a
neurofibroma (12,13).
To conclude, the definitive treatment for benign
schwannoma is surgical removal. The prognosis of these lesions is
good (14), recurrence is unusual
and malignant transformation is extremely rare (15). To the best of our knowledge, the
present study reports the first case of symptomatic schwannoma of
the abdominal wall. A lesion located in the abdominal wall should
be considered among the rare causes of unexplained abdominal
pain.
References
|
1
|
Forthman CL and Blazar PE: Nerve tumors of
the hand and upper extremity. Hand Clin. 20:233–242. 2004.
View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Abernathey CD, Onofrio BM, Scheithauer B,
et al: Surgical management of giant sacral schwannomas. J
Neurosurg. 65:286–295. 1986. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Li Q, Gao C, Juzi JT and Hao X: Analysis
of 82 cases of retroperitoneal schwannoma. ANZ J Surg. 77:237–240.
2007. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Bhatia RK, Banerjea A, Ram M and Lovett
BE: Benign ancient schwannoma of the abdominal wall: an unwanted
birthday present. BMC Surg. 10:12010. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Mishra A, Hamadto M, Azzabi M and Elfagieh
M: Abdominal wall schwannoma: case report and review of the
literature. Case Rep Radiol. 2013:4568632013.PubMed/NCBI
|
|
6
|
Hayashi M, Takeshita A, Yamamoto K and
Tanigawa N: Primary hepatic benign schwannoma. World J Gastrointest
Surg. 4:73–78. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
White W, Shiu MH, Rosenblum MK, Erlandson
RA and Woodruff JM: Cellular schwannoma. A clinicopathologic study
of 57 patients and 58 tumors. Cancer. 66:1266–1275. 1990.
View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Theodosopoulos T, Stafyla VK, Tsiantoula
P, et al: Special problems encountering surgical management of
large retroperitoneal schwannomas. World J Surg Oncol. 6:1072008.
View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Hide IG, Baudouin CJ, Murray SA and
Malcolm AJ: Giant ancient schwannoma of the pelvis. Skeletal
Radiol. 29:538–542. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Dodd LG, Marom EM, Dash RC, Matthews MR
and McLendon RE: Fine-needle aspiration cytology of “ancient”
schwannoma. Diagn Cytopathol. 20:307–311. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Argenyi ZB, Balogh K and Abraham AA:
Degenerative (“ancient”) changes in benign cutaneous schwannoma. A
light microscopic, histochemical and immunohistochemical study. J
Cutan Pathol. 20:148–153. 1993. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Beaman FD, Kransdorf MJ and Menke DM:
Schwannoma: radiologic-pathologic correlation. Radiographics.
24:1477–1481. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Tsai WC, Chiou HJ, Chou YH, et al:
Differentiation between schwannomas and neurofibromas in the
extremities and superficial body: the role of high-resolution and
color Doppler ultrasonography. J Ultrasound Med. 27:161–166.
2008.PubMed/NCBI
|
|
14
|
Eizinger FM and Weiss SW: Benign tumors of
peripheral nerves. Soft Tissue Tumors. Third edition. Mosby; St.
Louis, MO: pp. 829–842. 1995
|
|
15
|
Akin M, Bozkirli B, Leventoglu S, et al:
Liver schwannoma incidentally discovered in a patient with breast
cancer. Bratisl Lek Listy. 110:298–300. 2009.PubMed/NCBI
|