Introduction
Diabetic nephropathy (DN) is the main cause of end
stage renal disease (ESRD), accounting for ~44% of all ESRD cases,
and seriously affects patients' quality of life (1). Pathologically, early DN is
characterized by glomerular hyperfiltration, glomerular and renal
hypertrophy, increased urinary albumin excretion, and increased
basement membrane thickening and mesangial expansion with the
accumulation of extracellular matrix and podocyte injury (2). Currently, the pathogenesis of DN is
attributed to abnormal cell signal transduction, an immune
response, and metabolic disorders, renin-angiotensin system (RAS)
and other associated disorders. Previous studies have demonstrated
that Wnt/β-catenin signaling is able to downregulate nephrin
expression in podocytes and impair the glomerular filtration
barrier, resulting in proteinuria; however, it has been
demonstrated that inhibiting this pathway reduces podocyte damage
(3,4). Furthermore, aberrant activation of
Wnt/β-catenin signaling may induce extracellular matrix
accumulation and glomerulosclerosis by raising TGF-β1 expression,
thus affecting the development of DN (5). Certain therapeutic strategies are able
to effectively inhibit the progression of DN and recent studies
have confirmed that treatment with angiotensin II receptor blockers
reduces proteinuria and delays DN progression (6,7).
However, the identification of novel therapeutic reagents,
particularly those able to potently inhibit Wnt/β-catenin
signaling, may provide an improved treatment option.
Tripterygium wilfordii (TW) is a type of
traditional Chinese medicine that has been used to treat a variety
of primary and secondary glomerular diseases due to its
effectiveness in attenuating proteinuria (8). Previous studies have demonstrated that
TW has potent anti-inflammatory and regulatory properties, as well
as the ability to promote mesangial cell apoptosis and protect
podocytes from inflammatory injury (9,10). TW
has been extensively used in China for the treatment of autoimmune
diseases, including rheumatoid arthritis, systemic lupus
erythematosus (SLE), nephrotic syndrome (11), and has been used to treat patients
with DN (12); however, it has not
yet been determined whether TW is able to modulate Wnt/β-catenin
signaling in kidney tissue. Furthermore, the association between
the downregulation of Wnt/β-catenin signaling and improvement in
kidney function in individuals with DN is currently unclear.
In the present study, a rat model of DN was induced
by streptozotocin. Diabetic rats were then randomly treated with
vehicle (sodium carboxymethyl cellulose; SCC), TW combined with SCC
(8 or 16 mg/kg) or irbesartan (50 mg/kg) daily for 8 weeks.
Metabolic parameter levels and renal pathological changes were
examined. mRNA and protein expression levels of Wnt-1, glycogen
synthase kinase (GSK)-3β, β-catenin, nuclear factor (NF)-κB and
transforming growth factor (TGF)-β1 in the kidneys of rats from all
groups were measured. The aim of the present study was to observe
the association between renal injury and Wnt/β-catenin expression
by establishing a DN rat model, and investigate the possible
mechanisms of repairing renal injury in DN with TW.
Materials and methods
Animals
A total of 60 male Sprague-Dawley (SD) rats (8 weeks
old, weighing 180–200 g) were obtained from the Laboratory Animal
Center of the Bengbu Medical College (license no. SYXK, Anhui
2012–002; Bengbu, China). SD rats were housed in a specific
pathogen free facility at 24±1°C and 60% humidity, and exposed to a
12-h dark-light cycle. During the experiment, the rats accessed
food and water freely, and were not administered with insulin. The
present study was approved by the Animal Ethics Committee of Bengbu
Medical College (Bengbu, China).
Diabetes induction and treatment
SD rats were randomly divided into two groups: A
control group (n=10) and a diabetes mellitus (DM) group (n=50). All
rats were fasted overnight. The control group was injected
intraperitoneally (i.p.) with vehicle (0.1 mol/l citrate buffer, pH
4.5) and the DM group received an i.p. injection of 55 mg/kg
streptozotocin (STZ; Sigma-Aldrich; Merck KGaA, Darmstadt, Germany)
to induce diabetes. After 3 days, the blood glucose (BG) levels of
rats were measured using a glucose analyzer (One Touch SureStep;
Johnson & Johnson, New Brunswick, NJ, USA) and individual rats
with three consecutive BG readings >16.7 mmol/l were considered
diabetic (n=48). The BG of two mice were <16.7 mmol/l, therefore
they were not considered diabetic and were excluded from the rest
of the study. In the DM group (n=12), diabetic rats were randomly
fed with 0.5% sodium carboxymethyl cellulose (CMC-Na, 5 ml/kg) once
daily by gavage. Rats in the Control group (n=10) received the same
amount of CMC-Na (5 ml/kg) once daily by gavage. Diabetic rats in
the TW8 groups (n=12) received 8 mg/kg and TW16 groups (n=12)
received 16 mg/kg TW (Shanghai Fudan Fuhua Pharmaceutical Co.,
Ltd., Shanghai, China) combined with 5 ml/kg CMC-Na by once daily
by gavage. Diabetic rats in the Irbesartan group received 50 mg/kg
irbesartan [Sanofi-Aventis Minsheng (Hangzhou) Co., Ltd., Hangzhou,
China] combined with 5 ml/kg CMC-Na once daily by gavage. All rats
received treatment for 8 consecutive weeks. The body weights of
individual rats were measured weekly to allow adjustment of
dosages. During the experiment, rats were fed a standard diet, had
free access to food and drinking water and did not receive
insulin.
Blood sample and tissue
collection
One day prior to the end of the experiment, 24-h
urine samples were collected from all rats. The concentration of
urinary protein in the 24-h urine samples (24 h U-PRO; normal
reference range, 0–30 mg daily) was determined using urine protein
determination kit (cat. no. 59400370314; Shaoxing Medical Biotech,
Inc., Zhejiang, China), according to manufacturer's protocol. At
the end of the experiment, the body weights of rats from each group
were measured. Individual rats were injected i.p. with 50 mg/kg
pentobarbital (Sigma-Aldrich; Merck KGaA) to induce anesthesia and
their blood samples were collected. BG (normal reference range,
4.3–7.3 mmol/l), blood urea nitrogen (BUN; normal reference range,
4.3–9.8 mmol/l) and serum creatinine (Scr; normal reference range,
35–63 µmol/l) levels were analyzed using an OLYMPUS automatic
biochemical analyzer (Olympus Corporation, Tokyo, Japan). The rats
were sacrificed and the kidneys were perfused in vivo via
the right carotid artery with 100 ml of normal saline at 4°C, while
the renal vein was punctured to permit the perfusate to drain, then
the kidneys were removed immediately. The left kidneys of
individual rats were weighed to calculate the ratio of kidney
weight/body weight (KW/BW). Kidney tissues (8-mm thick) were fixed
in 10% formalin solution at room temperature for 48 h and
paraffin-embedded. Kidney sections were cut (3-µm thick) and
subjected to histological and immunohistochemistry examinations.
Remaining kidney tissues were cut into small pieces (1-mm thick)
and immersed in 4°C ethyl alcohol for 4 h prior to transmission
electron microscopy. The right kidneys were stored at −70°C until
they were assayed.
Renal pathology and
immunohistochemistry examination
The 3-µm thick formalin-fixed kidney sections were
stained with Periodic Acid-Schiff (PAS) or Masson's reagent. The
digital images of glomeruli and interstitial areas of individual
kidney samples were captured under a light microscope
(magnification, ×400). The mean glomerular area (AG) and
area of extracellular matrix (AECM) in six glomeruli of
individual kidney samples was calculated using Image-Pro Plus 6.0
analysis software (Media Cybernetics, Inc., Rockville, MD, USA).
The mean glomerular volume (VG) of individual kidney
samples was calculated using the formula
VG=β/K[AG] 3/2 [as described previously
(13)], where β=1.38 is the size
distribution coefficient and K=1.1 is the shape coefficient for
glomeruli idealized as a sphere. The mean Masson-positive stained
areas in six glomeruli and interstitial areas of individual kidney
samples were analyzed.
The impact of treatment on Wnt-1 and β-catenin
expression in the kidney tissues of rats from the different groups
was determined using immunohistochemistry. Kidney sections (3-µm
thick) were rehydrated, treated with 3% H2O2
for 10 min at room temperature and subjected to antigen retrieval.
The sections were blocked with 5% fat-free dry milk for 60 min at
room temperature and probed with rabbit anti-rat Wnt-1 polyclonal
antibodies (1:200; cat. no. sc-514531; Santa Cruz Biotechnology,
Inc., Dallas, TX, USA) and mouse anti-rat β-catenin monoclonal
antibodies (1:200; cat. no. sc-221398A; Santa Cruz Biotechnology,
Inc.) overnight at 4°C. Following washing, bound antibodies were
detected with horseradish peroxidase (HRP)-conjugated goat
anti-mouse IgG antibodies (1:1,000) and visualized with
3,3′-Diaminobenzidine, the antibodies and reagent were supplied by
the Ultra-Sensitive Streptavidin-Peroxidase (mouse) IHC kit (cat.
no. 9701; Fuzhou Maixin Biotech. Co., Ltd., Fuzhou, China)
according to the manufacturer's protocol. The immunostained
sections were viewed under a light microscope. A total of 10
glomerular and interstitial regions were randomly selected and
imaged (magnification, ×400). The immunostaining intensity (optical
density) of six glomerular and interstitial areas in individual
kidney samples was analyzed by Image-Pro Plus 6.0 analysis software
(Media Cybernetics, Inc.) in a blinded manner.
Electronic microscopy
Tissue specimens were cut into small pieces, washed
in pH 7.6 phosphate buffer and fixed with 2.5% glutaraldehyde for 4
h at 4°C. The fixed tissues were dehydrated with graded
concentrations of acetone, embedded in Araldite and cut into
ultrathin sections (50 nm). Following staining with uranyl acetate
and lead citrate, the kidney sections were examined under a Hitachi
Hu-12A transmission electron microscope (Hitachi, Ltd., Tokyo,
Japan; magnification, ×7,000).
Isolation of total mRNA and reverse
transcription-quantitative polymerase chain reaction (RT-qPCR)
Total RNA was extracted from individual right kidney
samples using TRIzol reagent. Following the determination of RNA
concentration and purity by an ultraviolet spectrophotometer
(NanoDrop™ 2000; Thermo Fisher Scientific Inc., Waltham, MA, USA),
RNA samples (5 µg/sample) were reverse transcribed into cDNA using
a PrimeScript™ RT reagent kit (cat. no. RR047A; Takara
Biotechnology Co., Ltd., Dalian, China). qPCR was performed using
the SYBR-Green kit (cat. no. RR820A; Takara Biotechnology Co.,
Ltd.) and specific primers (Sangon Biotech Co., Ltd., Shanghai,
China) in an Applied Biosystems StepOne Real-Time PCR machine
(Applied Biosystems; Thermo Fisher Scientific Inc.). The sequences
of primers and product lengths are presented in Table I. qPCR was performed using
SYBR® Premix Ex Taq™ II in a 20 µl reaction volume. Each
reaction was comprised of 2 µl of the cDNA solution, 10 µl of SYBR
Premix Ex Taq (2X), 1.6 µl of primers, 0.4 µl of ROX Reference Dye
and 6 µl of nuclease-free water. The thermocycling protocol was as
follows: 95°C for 30 sec for initial denaturation, 40 cycles of
95°C for 5 sec and 60°C for 30 sec for PCR, and 95°C for 15 sec,
60°C for 30 sec and 95°C for 15 sec for separation. β-actin was
used as a reference gene and primer sequences are provided in
Table I. The relative gene
expression levels of Wnt-1, glycogen synthase kinase (GSK)-3β,
β-catenin, nuclear factor (NF)-κB and transforming growth factor
(TGF)-β1 to control β-actin mRNA transcripts were determined using
the 2−ΔΔCq method (14).
 | Table I.Primer sequences and lengths for
reverse transcription-quantitative polymerase chain reaction. |
Table I.
Primer sequences and lengths for
reverse transcription-quantitative polymerase chain reaction.
| Primer | Sequence (5′-3′) | Product length
(bps) |
|---|
| Wnt-1 | Forward:
GGTGGGGCATCGTGAACATAG | 296 |
|
| Reverse:
GGAGGTGATTGCGAAGATAAACG |
|
| GSK-3β | Forward:
ATGCCTGTCTCCTCTAACGC | 321 |
|
| Reverse:
GGTCTTGGTGGCGGGTTT |
|
| β-catenin | Forward:
GCTGACCAAACTGCTAAATGACGA | 192 |
|
| Reverse:
TGTAGGGTCCCAGCGGTACAA |
|
| NF-κB | Forward:
CTGGAAGCACGAATGACAGA | 297 |
|
| Reverse:
TTTCAAGTTGGATGCATTGG |
|
| TGF-β1 | Forward: CCAACTA
TTGCTTCAGCTCCA | 154 |
|
| Reverse:
GTGTCCAGGCTCCAAATGT |
|
| β-actin | Forward:
CACCCGCGAGTACAACCTTC | 207 |
|
| Reverse:
CCCATACCCACCATCACACC |
|
Western blot analysis
Frozen kidney tissue samples were homogenized in
radioimmunoprecipitation assay lysis solution (cat. no. P0013B;
Beyotime Institute of Biotechnology, Jiangsu, China) and
centrifuged (12,000 × g) for 10 min at 4°C. Following
quantification of protein concentrations using a BCA protein assay
kit (cat. no. P0012; Beyotime Institute of Biotechnology), tissue
lysates (30 µg/lane) were separated by 10% SDS-PAGE and transferred
onto nitrocellulose membranes. The membranes were blocked with 5%
fat-free dry milk for 1 h at room temperature and incubated with
primary antibodies directed against Wnt-1 (cat. no. sc-514531),
GSK-3β (cat. no. sc-81462), p-GSK-3β (cat. no. sc-81495), β-catenin
(cat. no. sc-221398A), NF-κB-p65 (cat. no. sc-71675) and TGF-β1
(cat. no. sc-130348; all 1:500) or anti-β-actin (cat. no. sc-69879;
1:800; all Santa Cruz Biotechnology, Inc.) overnight at 4°C.
Following washing, membranes were incubated with HRP-conjugated
goat anti-mouse IgG (1:2,000; cat. no. BA1051; Wuhan Boster
Biological Technology, Ltd., Wuhan, China) for 1 h at room
temperature. Membranes were incubated with the secondary antibodies
alone as a negative control. Bound antibodies were detected by
enhanced chemiluminescence reagents. The relative levels of target
protein expression to control were determined by densitometric
scanning using an AlphaEase FC 4.0 image analysis system (Alpha
Innotech Corporation, San Leandro, CA, USA).
Statistical analysis
Data are presented as the mean ± standard deviation.
The difference among groups was analyzed by repeated one-way
analysis of variance followed by least significant difference and
the data between two groups were analyzed by t-test with SPSS 13.0
software (SPSS, Inc., Chicago, IL, USA). The potential correlation
between variants was analyzed by the Pearson correlation test.
P<0.05 was considered to indicate a statistically significant
difference.
Results
Treatment with TW significantly
mitigates hyperglycemia-related metabolic parameter values in
rats
To determine the effect of TW on
hyperglycemia-related kidney injury, SD rats were injected with STZ
to induce hyperglycemia and treated by gavage with vehicle,
different doses (8 or 16 mg/kg) of TW, or irbesartan (50 mg/kg)
daily for 8 weeks. During the observation period, two rats from
each of the DM, TW8, and Irbesartan groups and one from the TW16
group succumbed from gavage-related causes and were therefore
excluded from the statistical analyses. Laboratory examinations
indicated that rats in the DM group had significantly higher levels
of BG, Scr, BUN and 24-h urinary protein (24-h U-PRO) than rats in
the control group (all P<0.01), indicating that they developed
hyperglycemia and renal functional impairment (Table II). Although treatment with either
TW (8 or 16 mg/kg) or irbesartan did not significantly alter the
levels of BG, treatment with TW (8 or 16 mg/kg) or irbesartan did
significantly reduce the levels of Scr, BUN and 24-h U-PRO in rats
compared with the DM group (P<0.01; Table II). These results indicate that the
therapeutic effect of TW may be dose-dependent. In the present rat
model, although treatment with irbestartan elicited a similar
biochemical response on rats as treatment with TW, TW treatment
appeared to have an improved effect on reducing
hyperglycemia-related renal functional impairment. The present data
suggest that treatment with TW or irbesartan significantly
mitigated hyperglycemia-related renal functional impairment in
rats.
 | Table II.Metabolic parameters in rats from all
five groups. |
Table II.
Metabolic parameters in rats from all
five groups.
| Group | Dose (mg/kg) | N | BG (mmol/l) | Scr (µmol/l) | BUN (mmol/l) | 24 h U-PRO (mg/24
h) |
|---|
| Control | – | 10 | 5.23±0.45 | 54.62±9.23 | 5.98±0.82 | 9.37±1.66 |
| DM | – | 10 |
27.40±3.37a |
99.46±7.67a |
12.62±2.83a |
76.73±10.27a |
| TW8 | 8 | 10 |
26.31±3.12a |
72.39±7.52a,b |
8.48±1.2a,b |
42.55±4.86a,b |
| TW16 | 16 | 11 |
26.01±3.15a |
66.26±7.46a,b |
7.87±1.06b,c |
36.13±6.07a,b |
| Irbesartan | 50 | 10 |
27.42±3.07a |
74.81±7.23a,b |
9.10±1.91a,b |
43.41±6.35a,b |
Treatment with TW reduces
hyperglycemia-induced kidney injury in diabetic rats
The impact of TW treatment on pathological changes
in the kidney tissues of rats was investigated. The KW/BW ratio of
rats in the DM group was significantly increased compared with the
healthy rats in the Control group (P<0.01; Table III). Treatment with irbesartan or 8
mg/kg TW significantly reduced the ratio of KW/BW in diabetic rats
compared with the DM group (P<0.05). Rats treated with 16 mg/kg
TW exhibited a significantly reduced ratio of KW/BW compared with
rats in the DM group (P<0.01), which was notably decreased
compared with rats treated with 8 mg/kg TW (Table III). PAS staining indicated no
abnormalities in the kidney sections of rats in the Control group.
Conversely, glomerular and renal hypertrophy, thickened basement
membranes and mesangial expansion with the accumulation of
extracellular matrix was detected in the kidney sections of rats in
the DM group. However, reduced pathological changes were observed
in the kidney sections of rats in the TW8, TW16 and Irbesartan
groups, particularly in the TW16 group (Fig. 1). Similarly, potent Masson staining
was detected in the kidney sections of rats in the DM group;
however, significantly reduced Masson staining intensity was
observed in rats from the TW8, TW16 and Irbesartan groups compared
with the DM group (P<0.01; Fig.
1B). Notably, limited Masson staining was observed in the
kidney sections of rats in the TW16 group. The results indicated
that treatment with TW reduced hyperglycemia-induced kidney
fibrosis in rats (Fig. 1). In
addition, hypertrophy and fusion of podocytes, and thickened
basement membranes were detected in the glomeruli of rats in the DM
group using electron microscopy. However, less severe pathological
changes were observed in the kidney sections of rats in the TW and
Irbesartan groups (Fig. 1).
Quantitative analysis of the glomerular size revealed that although
the AG and AECM in rats from the TW8, TW16
and Irbesartan groups were increased significantly compared with
the Control group, these values were significantly decreased
compared with the DM group (P<0.01; Table III). Notably, the lowest values of
AG and AECM were observed in the TW16 group.
A similar pattern was observed regarding the values of
VG in rats from all five groups (Table III). The present results indicated
that treatment with TW effectively reduced hyperglycemia-induced
kidney injury in diabetic rats.
 | Table III.Morphological parameters in
glomerular and KW/BW in rats from all five groups. |
Table III.
Morphological parameters in
glomerular and KW/BW in rats from all five groups.
| Group | Dose (mg/kg) | N | KW/BW (g/100
g) | AG
(×103 µm2) | VG
(×105 µm3) | AECM
(×102 µm2) |
AECM/AG (%) |
|---|
| Control | – | 10 | 0.34±0.03 | 5.45±0.29 | 5.03±0.41 | 8.20±0.40 | 15.09±1.01 |
| DM | – | 10 |
0.63±0.10a |
8.03±0.64a |
9.02±1.07a |
22.54±1.33a |
28.23±2.74a |
| TW8 | 8 | 10 |
0.54±0.07a,b |
7.15±0.51a,c |
7.57±0.82a,c |
16.38±0.64a,c |
23.02±1.85a,c |
| TW16 | 16 | 11 |
0.46±0.06a,c |
6.49±0.42a,c |
6.54±0.62a,c |
12.98±0.53a,c |
20.11±1.85a,c |
| Irbesartan | 50 | 10 |
0.55±0.07a,b |
7.35±0.47a,c |
7.89±0.75a,c |
15.47±0.66a,c |
21.13±1.51a,c |
Treatment with TW impairs
hyperglycemia-induced upregulated Wnt-1, p-GSK-3β, β-catenin, NF-κB
and TGF-β1 expression in the kidneys of diabetic rats
To understand the molecular mechanisms underlying
the action of TW, the impact of TW treatment on Wnt-1, GSK-3β,
β-catenin, NF-κB and TGF-β1 expression in the kidney tissues of
rats was assessed. Compared with the DM group, the relative
expression of Wnt-1, β-catenin, NF-κB and TGF-β1 mRNA transcripts
in the kidneys of rats in the TW8, TW16 and Irbesartan groups were
significantly reduced (P<0.01), particularly in the TW16 group,
although levels of gene expression in all treatment groups remained
significantly higher compared with the Control group (all
P<0.01; Fig. 2). No significant
differences in the expression of GSK-3β mRNA were observed in any
of the groups (Fig. 2). Treatment
with 16 mg/kg TW provided an increased inhibitory effect compared
with 8 mg/kg TW or 50 mg/kg irbesartan in the present study
(Fig. 2).
 | Figure 2.Relative gene expression of (A) Wnt-1,
(B) GSK-3β, (C) β-catenin, (D) NF-κB and (E) TGF-β1 in the kidney
tissues of rats from the 5 groups. The relative gene expression
levels of Wnt-1, GSK-3β, β-catenin, NF-κB and TGF-β1 mRNA
transcripts to control β-actin in individual rats in the Control
(n=10), DM (n=10), TW8 (n=10), TW16 (n=11) and Irbesartan (n=10)
groups were determined by reverse transcription-quantitative
polymerase chain reaction. Data are expressed as the mean ±
standard deviation. ##P<0.01 vs. Control group;
**P<0.01 vs. DM group. GSK, glycogen synthase kinase; NF,
nuclear factor; TGF, transforming growth factor; DM, diabetes
mellitus; TW8, 8 mg/kg Tripterygium wilfordii; TW16, 16
mg/kg Tripterygium wilfordii. |
A similar pattern was detected in the levels of
Wnt-1, GSK-3β, p-GSK-3β, β-catenin, NF-κB-p65 and TGF-β1 protein
expression in the kidneys of rats in all groups (Fig. 3), further supporting that treatment
with TW mitigated hyperglycemia-induced Wnt-1, p-GSK-3β, β-catenin,
NF-κB p65 and TGF-β1 overactivation in the kidney of rats. Again,
no significant differences in the protein expression of GSK-3β were
detected in any of the groups (Fig.
3).
 | Figure 3.Expression of Wnt-1, GSK-3β, p-GSK-3β,
β-catenin, NF-κB and TGF-β1 protein relative to control β-actin in
the kidney tissues of individual rats from the Control (n=10), DM
(n=10), TW8 (n=10), TW16 (n=11) and Irbesartan (n=10) groups were
determined by western blotting. Data are representative images of
each group of rats. ##P<0.01 vs. Control group;
**P<0.01 vs. DM group. GSK, glycogen synthase kinase; p-,
phosphorylated; NF, nuclear factor; TGF, transforming growth
factor; DM, diabetes mellitus; TW8, 8 mg/kg Tripterygium
wilfordii; TW16, 16 mg/kg Tripterygium wilfordii. |
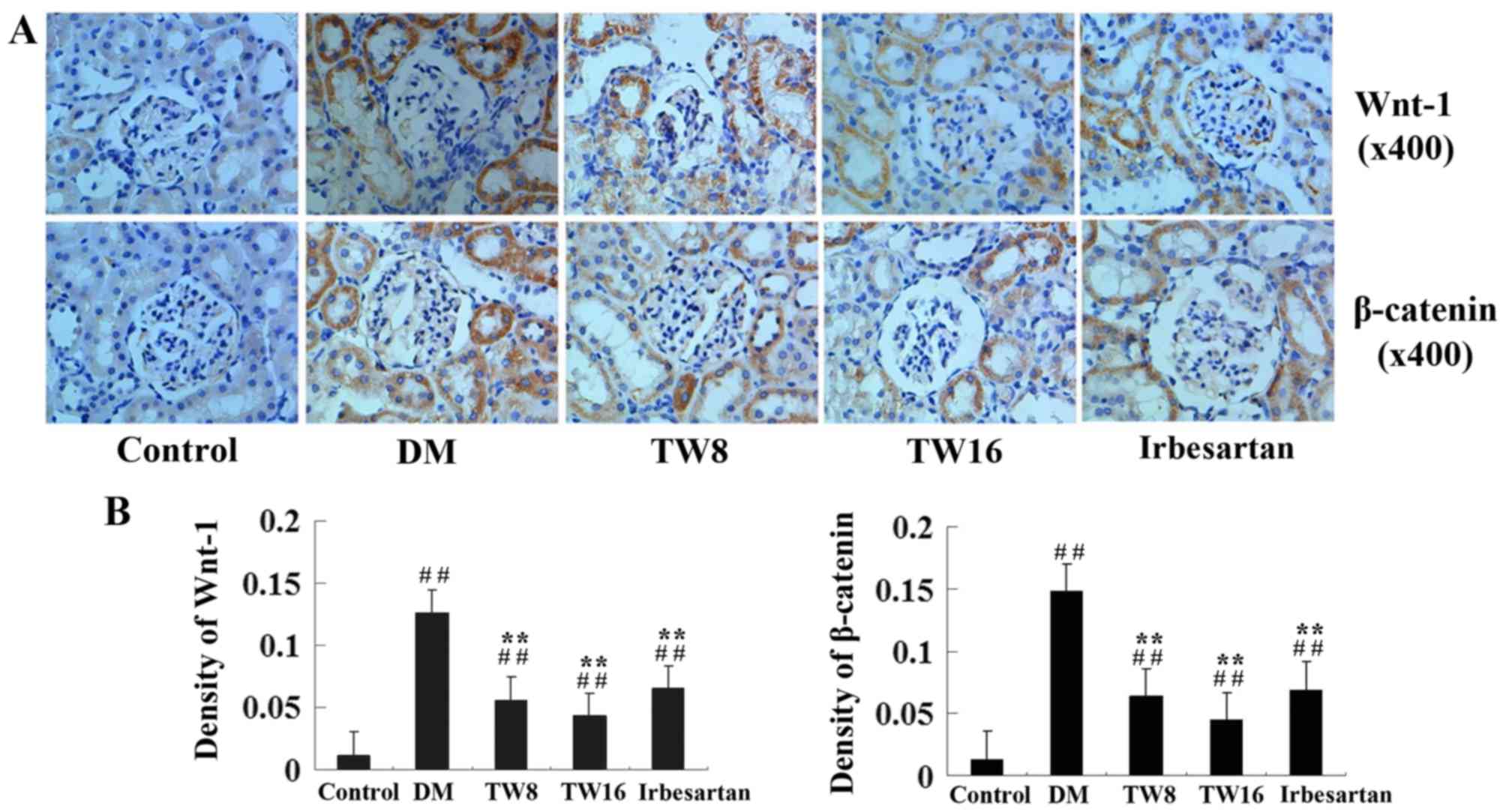
Furthermore, immunohistochemistry analysis revealed
that significantly increased anti-Wnt-1 and anti-β-catenin staining
occurred in the glomeruli and tubulointerstitial areas in the
kidneys of rats in the DM group compared with the Control group
(P<0.01; Fig. 4). However,
compared with the DM group, the kidney sections of rats in the TW8,
TW16 and Irbesartan groups exhibited significantly reduced
intensities of anti-Wnt-1 and anti-β-catenin staining (Fig. 4). Quantitative analysis indicated
that treatment with TW significantly mitigated the
hyperglycemia-induced Wnt and β-catenin over-expression in the
kidney of diabetic rats (P<0.01; Fig.
4). Therefore, these data demonstrate that treatment with TW
impairs hyperglycemia-upregulated Wnt-1 and β-catenin expression in
the kidney of diabetic rats.
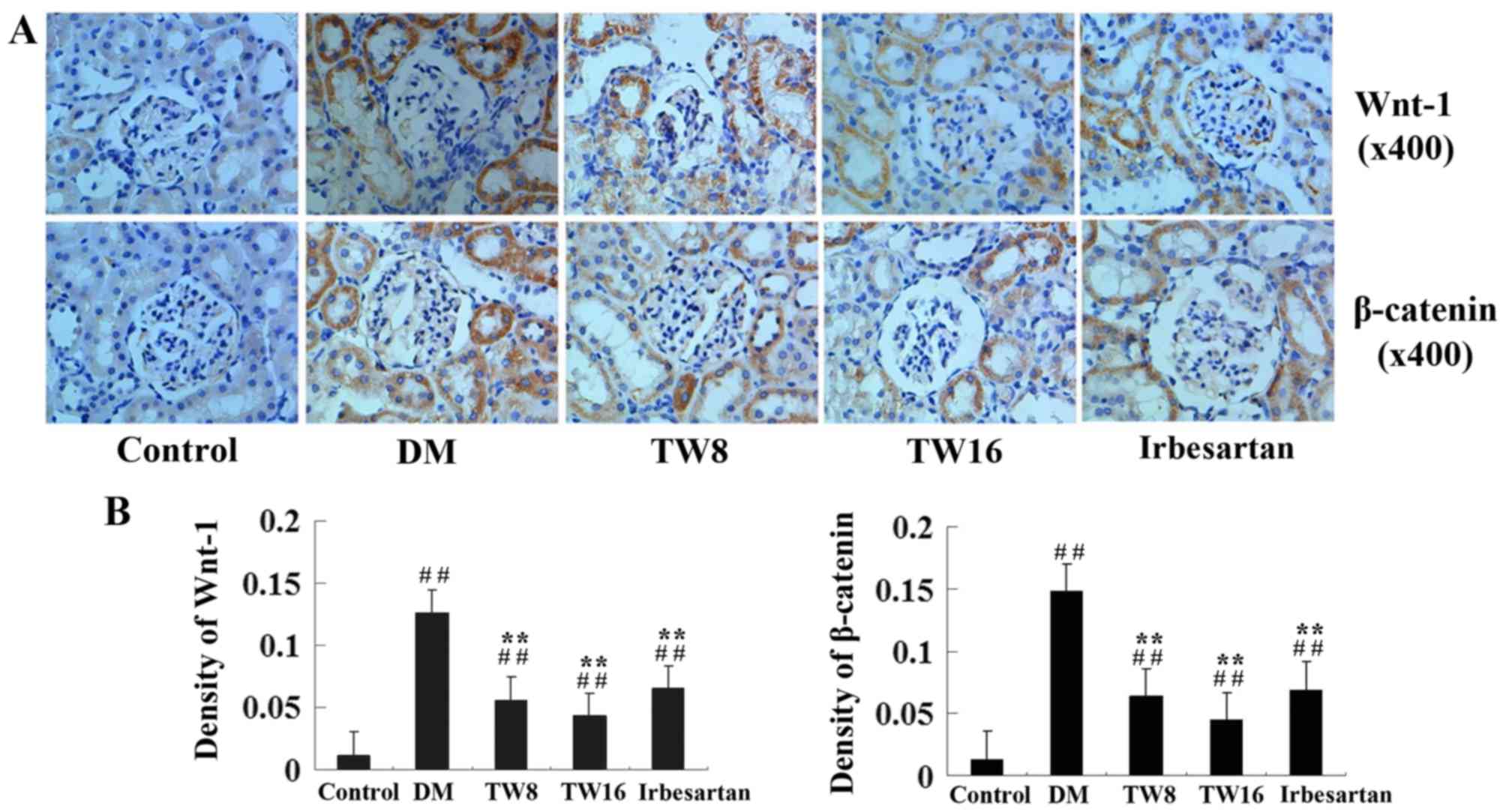 | Figure 4.Immunohistochemical analysis of Wnt-1
and β-catenin expression in the kidney tissues of rats from the
Control (n=10), DM (n=10), TW8 (n=10), TW16 (n=11) and Irbesartan
(n=10) groups. The expression of Wnt-1 and β-catenin in the kidney
tissues of individual rats were determined by (A)
immunohistochemistry and (B) quantitatively analyzed. Data are
representative images of the kidney tissues of each group of rats
(magnification, ×400). ##P<0.01 vs. Control group;
**P<0.01 vs. DM group. GSK, glycogen synthase kinase; NF,
nuclear factor; TGF, transforming growth factor; DM, diabetes
mellitus; TW8, 8 mg/kg Tripterygium wilfordii; TW16, 16
mg/kg Tripterygium wilfordii. |
Correlation analysis
Correlation analysis of data from all five groups
indicated a significant positive linear correlation between Wnt-1
mRNA and protein expression, and β-catenin mRNA and protein
expression (P<0.01). Notably, the levels of Wnt-1 and β-catenin
expression were significantly positively correlated with the ratios
of KW/BW and the levels of 24U-PRO, AG, VG,
AECM/AG and GBMT in all five groups of rats
(P<0.01; Table IV).
 | Table IV.Correlation analysis. |
Table IV.
Correlation analysis.
| Index | Wnt-1 protein | β-catenin
protein |
|---|
| 24-h U-PRO | r=0.953,
P<0.001 | r=0.919,
P<0.001 |
| KW/BW | r=0.592,
P=0.006 | r=0.580,
P=0.007 |
| AG | r=0.882,
P<0.001 | r=0.824,
P<0.001 |
| VG | r=0.882,
P<0.001 | r=0.825,
P<0.001 |
|
AECM/AG | r=0.857,
P<0.001 | r=0.889,
P<0.001 |
| GBMT | r=0.932,
P<0.001 | r=0.945,
P<0.001 |
| Wnt-1 mRNA | r=0.972,
P<0.001 | – |
| β-catenin mRNA | – | r=0.943,
P<0.001 |
Discussion
Previous studies have demonstrated that treatment
with TW benefits patients with DN (12). However, the mechanisms underlying the
action of TW have not been clarified. The Wnt/β-catenin signaling
pathway is crucial for the pathogenesis of DN, particularly in the
early process of DN (15);
therefore, the current study investigated the effect of treatment
with TW on Wnt/β-catenin expression in the kidney tissues of rats
in the early stage of DN. The present results indicated that
treatment with TW did not significantly alter BG levels; however,
TW treatment did significantly reduce the levels of BUN, Scr and
24-h U-PRO, particularly when a higher dose of TW (16 mg/kg) was
used in rats. Administration of 16 mg/kg TW provoked an improved
therapeutic effect compared with the positive control, irbesartan,
in the present experimental system. Treatment with TW also
significantly reduced the ratios of KW/BW and the values of
AG, VG, AECM/AG and
GBMT compared with those in the DM group. In addition, treatment
with TW dramatically reduced hyperglycemia-induced fibrosis and
kidney injury and the relative levels of Wnt-1 and β-catenin
expression in the kidney tissues of rats. Furthermore, Wnt-1 and
β-catenin expression was positively correlated with the ratios of
KW/BW, as well as levels of 24-h U-PRO, AG,
VG, AECM/AG and GBMT in rats from
all five groups. The present data supports the notion that
Wnt/β-catenin signaling is crucial in the pathogenesis of DN.
Various factors may contribute to the early
development of DN, including aberrant action of cell signaling,
abnormal immune and inflammatory responses, and increased levels of
the cytokines, TGF-β1 and NF-κB (16,17). In
the present study glomerular and renal hypertrophy, thickened
basement membranes and mesangial expansion with the accumulation of
extracellular matrix in the kidney sections of rats in the DM group
were observed. Furthermore, potent Masson staining was identified
in the kidney sections of rats in the DM group and increased
basement membrane thickness and podocyte hypertrophy and fusion
were detected in the glomeruli of the kidney sections of rats in
the DM group. Moreover, the values of AG, VG,
AECM/AG and GBMT were significantly increased
in rats from the DM group. Notably, upregulated Wnt-1, p-GSK-3β,
β-catenin, NF-κB and TGF-β1 expression levels were detected in the
kidney tissues of rats in the DM group. These data indicate that
during the early process of DM, aberrant activation of
Wnt/β-catenin signaling contributes to NF-κB and TGF-β1
over-expression, as well as hyperglycemia-induced functional
impairment and structural damage in the kidneys of rats. The
present findings were in agreement with those from a previous
study, which suggested that activation of Wnt/β-catenin signaling
was associated with hyperglycemia-induced podocyte apoptosis and
glomerular injury (18). In
addition, the present results extended on previous findings
demonstrating that the aberrant activation of the Wnt/β-catenin
signaling contributes to the development of multiple chronic kidney
disease (19). Therefore, the
Wnt/β-catenin signaling pathway may be a potential target for the
development of novel therapies for DN.
TW is a type of traditional Chinese medicine that
has potent anti-inflammatory activity and provides protection from
hyperglycemia-induced kidney injury. It is associated with the
downregulation of NF-κB, osteopontin and TGF-β1 expression
(20,21). The present study indicated that
treatment with TW significantly reduced the ratios of KW/BW and the
levels of 24-h U-PRO, indicating a reduction of kidney injury in
rats. The present findings are consistent with those from a
previous study, which used a DN model (10). The present results indicated that TW
is able to protect hyperglycemia-induced kidney injury in animals
and notably, that treatment with a higher dose of TW (16 mg/kg)
provided an improved protective effect compared with irbesartan
treatment. This is similar to the results of a previous study
(22). Furthermore, the present
study indicated that treatment with TW significantly attenuated
hyperglycemia-upregulated Wnt-1 and β-catenin expression in the
kidney tissues of rats. Given that Wnt/β-catenin signaling
positively regulates pro-inflammatory responses, it is possible
that TW may inhibit activation of the Wnt/β-catenin signaling
pathway and in turn, mitigate hyperglycemia-induced inflammation,
such as NF-κB and TGF-β1, to protect the kidney from
hyperglycemia-induced injury (20).
Notably, the current study observed that treatment with irbesartan
alone significantly mitigated hyperglycemia-induced upregulated
Wnt-1 and β-catenin expression in the kidney tissues of diabetic
rats. These findings may explain why the combination of TW and
irbesartan synergistically protect against hyperglycemia-induced
podocyte injury in patients with DN (23).
In conclusion, the present study demonstrated that
treatment with TW mitigated hyperglycemia-induced functional
impairment and structural injury of the kidney in a rat model of
DM. Furthermore, treatment with TW significantly mitigated
hyperglycemia-induced upregulated Wnt-1 and β-catenin expression in
the kidney of diabetic rats, suggesting that the aberrant
activation of Wnt/β-catenin signaling may contribute to the early
development of DN. The present findings may provide new insights
into the pathogenesis of DN and molecular mechanisms underlying the
action of TW in treatment of DN.
Acknowledgements
Not applicable.
Funding
The present study was supported by the Key Program
of Natural Science Foundation of Higher Education of Anhui Province
(grant nos. KJ2013A191 and KJ2015B008by) and Natural Science
Foundation of Bengbu Medical College (grant no. BYKY1457).
Availability of data and materials
The datasets used and/or analyzed during the current
study are available from the corresponding author on reasonable
request.
Authors' contributions
All authors contributed significantly to the
conception and implementation of the study. BC initiated the study,
was responsible for the experiment implementation, statistical
analysis and wrote the first draft and subsequent drafts. WC
initiated the study, was responsible for the experiment
implementation, and critically revised the first and subsequent
drafts for important intellectual content. PY was responsible for
the detection of biochemical indexes. YZ and LL assisted animal
feeding, gavage and collection of samples. All authors read and
approved the final draft.
Ethics approval and consent to
participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Doi T, Mima A, Matsubara T, Tominaga T,
Arai H and Abe H: The current clinical problems for early phase of
diabetic nephropathy and approach for pathogenesis of diabetic
nephropathy. Diabetes Res Clin Pract. 82 Suppl 1:S21–S24. 2008.
View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Zhu B, Wang Y, Jardine M, Jun M, Lv JC,
Cass A, Liyanage T, Chen HY, Wang YJ and Perkovic V:
Tripterygium preparations for the treatment of CKD: A
systematic review and meta-analysis. Am J Kidney Dis. 62:515–530.
2013. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Wang D, Dai C, Li Y and Liu Y: Canonical
Wnt/β-catenin signaling mediates transforming growth
factor-β1-driven podocyte injury and proteinuria. Kidney Int.
80:1159–1169. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Dai C, Stolz DB, Kiss LP, Monga SP,
Holzman LB and Liu Y: Wnt/beta-catenin signaling promotes podocyte
dysfunction and albuminuria. J Am Soc Nephrol. 20:1997–2008. 2009.
View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Ho C, Lee PH, Hsu YC, Wang FS, Huang YT
and Lin CL: Sustained Wnt/β-catenin signaling rescues high glucose
induction of transforming growth factor-β1-mediated renal fibrosis.
Am J Med Sci. 344:374–382. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Zain M and Awan FR: Renin angiotensin
aldosterone system (RAAS): Its biology and drug targets for
treating diabetic nephropathy. Pak J Pharm Sci. 27:1379–1391.
2014.PubMed/NCBI
|
|
7
|
Ren F, Tang L, Cai Y, Yuan X, Huang W, Luo
L, Zhou J and Zheng Y: Meta-analysis: The efficacy and safety of
combined treatment with ARB and ACEI on diabetic nephropathy. Ren
Fail. 37:548–561. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Wu Y, Ren K, Liang C, Yuan L, Qi X, Dong
J, Shen J and Lin S: Renoprotective effect of total glucosides of
paeony (TGP) and its mechanism in experimental diabetes. J
Pharmacol Sci. 109:78–87. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
He Y, Shi S, Zhang R, Shen W, Tu J, Ding Z
and Fan Y: In vitro immunosuppressive and cytotoxic activities of
Tripterygium wilfordii extract. Drug Chem Toxicol.
38:145–151. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Hao L, Pan MS, Zheng Y and Wang RF: Effect
of Cordyceps sinensis Tripterygium wilfordii polyglycosidium
on podocytes in rats with diabetic nephropathy. Exp Ther Med.
7:1465–1470. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Liu S, Li X, Li H, Liang Q and Chen J and
Chen J: Comparison of Tripterygium wilfordii multiglycosides
and tacrolimus in the treatment of idiopathic membranous
nephropathy: A prospective cohort study. BMC Nephrol. 16:2002015.
View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Ge Y, Xie H, Li S, Jin B, Hou J, Zhang H,
Shi M and Liu Z: Treatment of diabetic nephropathy with
Tripterygium wilfordii Hook F extract: A prospective,
randomized, controlled clinical trial. J Transl Med. 11:1342013.
View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Ota T, Takamura T, Ando H, Nohara E,
Yamashita H and Kobayashi K: Preventive effect of cerivastatin on
diabetic nephropathy through suppression of glomerular macrophage
recruitment in a rat model. Diabetologia. 46:843–851. 2003.
View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Livak KJ and Schmittgen TD: Analysis of
relative gene expression data using real-time quantitative PCR and
the 2(-Delta Delta C(T)) method. Methods. 25:402–408. 2001.
View Article : Google Scholar : PubMed/NCBI
|
|
15
|
He W, Kang YS, Dai C and Liu Y: Blockade
of Wnt/β-catenin signaling by paricalcitol ameliorates proteinuria
and kidney injury. J Am Soc Nephrol. 22:90–103. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Fernández Fernández B, Elewa U,
Sánchez-Niño MD, Rojas-Rivera JE, Martin-Cleary C, Eqido J and
Ortiz A: 2012 update on diabetic kidney disease: The expanding
spectrum, novel pathogenic insights and recent clinical trials.
Minerva Med. 103:219–234. 2012.PubMed/NCBI
|
|
17
|
Zhang W, Zhao L, Su SQ, Xu XX and Wu YG:
Total glucosides of paeony attenuate renal tubulointerstitial
injury in STZ-induced diabetic rats: Role of Toll-like receptor 2.
J Pharmacol Sci. 125:59–67. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Li Z, Xu J, Xu P, Liu S and Yang Z:
Wnt/β-catenin signalling pathway mediates high glucose induced cell
injury through activation of TRPC6 in podocytes. Cell Prolif.
46:76–85. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
He W, Dai C, Li Y, Zeng G, Monga SP and
Liu Y: Wnt/beta-catenin signaling promotes renal interstitial
fibrosis. J Am Soc Nephrol. 20:765–776. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Ma R, Liu L, Liu X, Wang Y, Jiang W and Xu
L: Triptolide markedly attenuates albuminuria and podocyte injury
in an animal model of diabetic nephropathy. Exp Ther Med.
6:649–656. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Ma ZJ, Zhang XN, Li L, Yang W, Wang SS,
Guo X, Sun P and Chen LM: Tripterygium glycosides tablet
ameliorates renal tubulointerstitial fibrosis via the toll-like
receptor 4/nuclear factor kappa B signaling pathway in high-fat
diet fed and streptozotocin-induced diabetic rats. J Diabetes Res.
2015:3904282015. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Gao Q, Shen W, Qin W, Zheng C, Zhang M,
Zeng C, Wang S, Wang J, Zhu X and Liu Z: Treatment of db/db
diabetic mice with triptolide: a novel therapy for diabetic
nephropathy. Nephrol Dial Transplant. 25:3539–3547. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Ma RX, Zhao N and Zhang W: The effects and
mechanism of Tripterygium wilfordii Hook F combination with
irbesartan on urinary podocyte excretion in diabetic nephropathy
patients. Zhonghua Nei Ke Za Zhi. 2:469–473. 2013.(In Chinese).
|