|
1
|
Sato H, Maeda K and Maruta M: Prognostic
significance of lateral lymph node dissection in node positive low
rectal carcinoma. Int J Colorectal Dis. 26:881–889. 2011.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Ishihara S, Kawai K, Tanaka T, Kiyomatsu
T, Hata K, Nozawa H, Morikawa T and Watanabe T: Oncological
outcomes of lateral pelvic lymph node metastasis in rectal cancer
treated with preoperative chemoradiotherapy. Dis Colon Rectum.
60:469–476. 2017.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Nagasaki T, Akiyoshi T, Fujimoto Y,
Konishi T, Nagayama S, Fukunaga Y and Ueno M: Preoperative
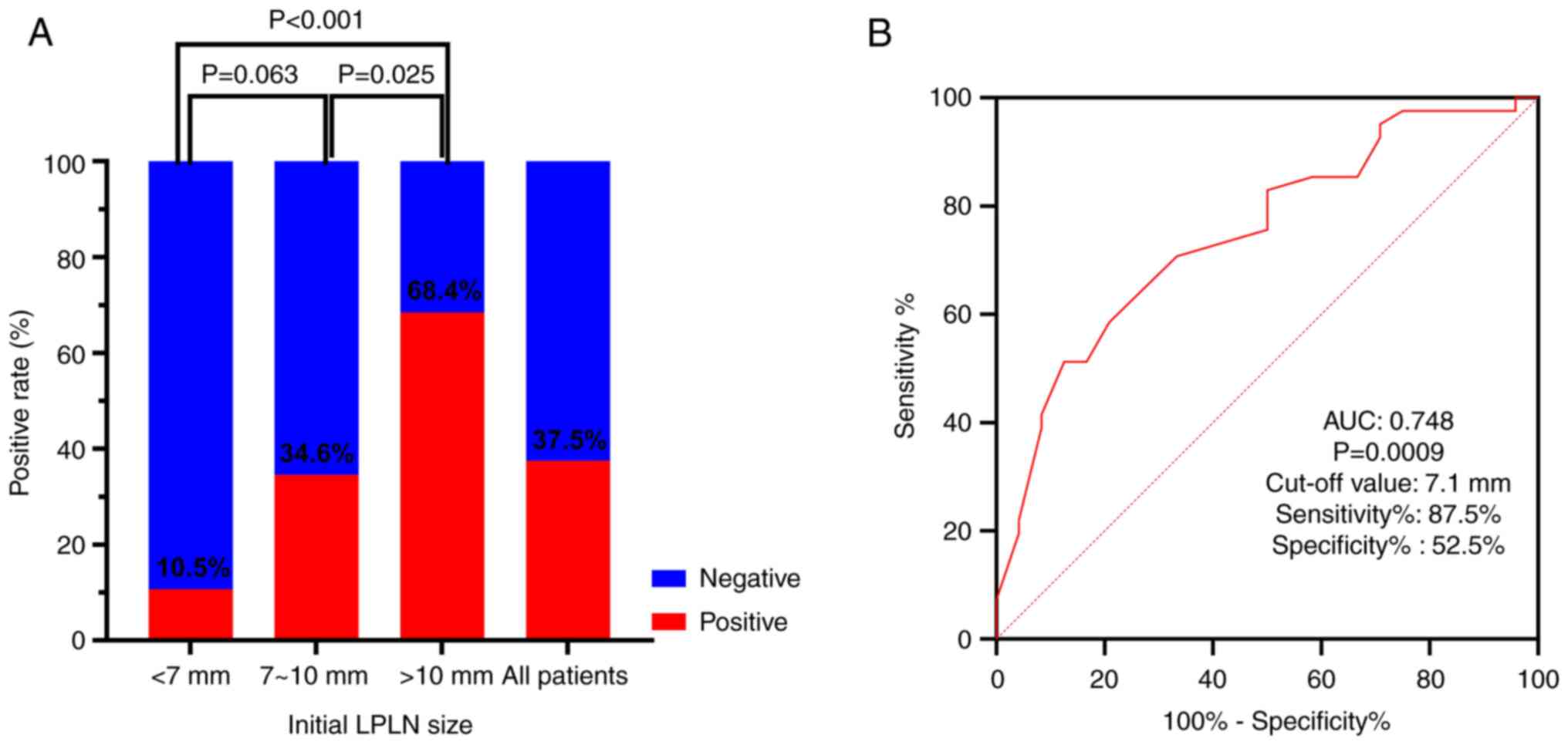
chemoradiotherapy might improve the prognosis of patients with
locally advanced low rectal cancer and lateral pelvic lymph node
metastases. World J Surg. 41:876–883. 2017.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Sugihara K, Kobayashi H, Kato T, Mori T,
Mochizuki H, Kameoka S, Shirouzu K and Muto T: Indication and
benefit of pelvic sidewall dissection for rectal cancer. Dis Colon
Rectum. 49:1663–1672. 2006.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Georgiou P, Tan E, Gouvas N, Antoniou A,
Brown G, Nicholls RJ and Tekkis P: Extended lymphadenectomy versus
conventional surgery for rectal cancer: A meta-analysis. Lancet
Oncol. 10:1053–1062. 2009.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Moriya Y: Treatment of lateral pelvic
nodes metastases from rectal cancer: The future prospective. G
Chir. 34:245–248. 2013.PubMed/NCBI
|
|
7
|
Yano H and Moran BJ: The incidence of
lateral pelvic side-wall nodal involvement in low rectal cancer may
be similar in Japan and the West. Br J Surg. 95:33–49.
2008.PubMed/NCBI View
Article : Google Scholar
|
|
8
|
Kobayashi H, Mochizuki H, Kato T, Mori T,
Kameoka S, Shirouzu K and Sugihara K: Outcomes of surgery alone for
lower rectal cancer with and without pelvic sidewall dissection.
Dis Colon Rectum. 52:567–576. 2009.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Kim HJ, Choi GS, Park JS, Park SY, Lee HJ,
Woo IT and Park IK: Selective lateral pelvic lymph node dissection:
A comparative study of the robotic versus laparoscopic approach.
Surg Endosc. 32:2466–2473. 2018.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Fujita S, Mizusawa J, Kanemitsu Y, Ito M,
Kinugasa Y, Komori K, Ohue M, Ota M, Akazai Y, Shiozawa M, et al:
Mesorectal excision with or without lateral lymph node dissection
for clinical stage II/III lower rectal cancer (JCOG0212): A
multicenter, randomized controlled, noninferiority trial. Ann Surg.
266:201–207. 2017.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Kim MJ, Chang GJ, Lim HK, Song MK, Park
SC, Sohn DK, Chang HJ, Kim DY, Park JW, Jeong SY and Oh JH:
Oncological impact of lateral lymph node dissection after
preoperative chemoradiotherapy in patients with rectal cancer. Ann
Surg Oncol. 27:3525–3533. 2020.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Amin MB, Edge SB, Greene FL and Brierley
JD: AJCC cancer staging manual, 8th edition. New York: Springer,
2017.
|
|
13
|
Ogura A, Konishi T, Cunningham C,
Garcia-Aguilar J, Iversen H, Toda S, Lee IK, Lee HX, Uehara K, Lee
P, et al: Neoadjuvant (chemo)radiotherapy with total mesorectal
excision only is not sufficient to prevent lateral local recurrence
in enlarged nodes: Results of the multicenter lateral node study of
patients with low cT3/4 rectal cancer. J Clin Oncol. 37:33–43.
2019.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Kroon HM, Malakorn S, Dudi-Venkata NN,
Bedrikovetski S, Liu J, Kenyon-Smith T, Bednarski BK, Ogura A, van
de Velde CJH, Rutten HJT, et al: Local recurrences in western low
rectal cancer patients treated with or without lateral lymph node
dissection after neoadjuvant (chemo)radiotherapy: An international
multi-centre comparative study. Eur J Surg Oncol. 47:2441–2449.
2021.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Kroon HM, Hoogervorst LA, Hanna-Rivero N,
Traeger L, Dudi-Venkata NN, Bedrikovetski S, Kusters M, Chang GJ,
Thomas ML and Sammour T: Systematic review and meta-analysis of
long-term oncological outcomes of lateral lymph node dissection for
metastatic nodes after neoadjuvant chemoradiotherapy in rectal
cancer. Eur J Surg Oncol. 48:1475–1482. 2022.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Yang X, Yang S, Hu T, Gu C, Wei M, Deng X,
Wang Z and Zhou Z: What is the role of lateral lymph node
dissection in rectal cancer patients with clinically suspected
lateral lymph node metastasis after preoperative chemoradiotherapy?
A meta-analysis and systematic review. Cancer Med. 9:4477–4489.
2020.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Oh HK, Kang SB, Lee SM, Lee SY, Ihn MH,
Kim DW, Park JH, Kim YH, Lee KH, Kim JS, et al: Neoadjuvant
chemoradiotherapy affects the indications for lateral pelvic node
dissection in mid/low rectal cancer with clinically suspected
lateral node involvement: A multicenter retrospective cohort study.
Ann Surg Oncol. 21:2280–2287. 2014.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Kawai K, Shiratori H, Hata K, Nozawa H,
Tanaka T, Nishikawa T, Murono K and Ishihara S: Optimal size
criteria for lateral lymph node dissection after neoadjuvant
chemoradiotherapy for rectal cancer. Dis Colon Rectum. 64:274–283.
2021.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Komori K, Fujita S, Mizusawa J, Kanemitsu
Y, Ito M, Shiomi A, Ohue M, Ota M, Akazai Y, Shiozawa M, et al:
Predictive factors of pathological lateral pelvic lymph node
metastasis in patients without clinical lateral pelvic lymph node
metastasis (clinical stage II/III): The analysis of data from the
clinical trial (JCOG0212). Eur J Surg Oncol. 45:336–340.
2019.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Wang P, Zhou S, Zhou H, Liang J and Zhou
Z: Evaluating predictive factors for determining the presence of
lateral pelvic node metastasis in rectal cancer patients following
neoadjuvant chemoradiotherapy. Colorectal Dis. 21:791–796.
2019.PubMed/NCBI View Article : Google Scholar
|
|
21
|
Bae JH, Song J, Kim JH, Kye BH, Lee IK,
Cho HM and Lee YS: Lateral lymph node size and tumor distance from
anal verge accurately predict positive lateral pelvic lymph nodes
in rectal cancer: A multi-institutional retrospective cohort study.
Dis Colon Rectum. 66:785–795. 2023.PubMed/NCBI View Article : Google Scholar
|
|
22
|
Ogura A, Konishi T, Beets GL, Cunningham
C, Garcia-Aguilar J, Iversen H, Toda S, Lee IK, Lee HX, Uehara K,
et al: Lateral nodal features on restaging magnetic resonance
imaging associated with lateral local recurrence in low rectal
cancer after neoadjuvant chemoradiotherapy or radiotherapy. JAMA
Surg. 154(e192172)2019.PubMed/NCBI View Article : Google Scholar
|
|
23
|
Schaap DP, Boogerd LSF, Konishi T,
Cunningham C, Ogura A, Garcia-Aguilar J, Beets GL, Suzuki C, Toda
S, Lee IK, et al: Rectal cancer lateral lymph nodes: Multicentre
study of the impact of obturator and internal iliac nodes on
oncological outcomes. Br J Surg. 108:205–213. 2021.PubMed/NCBI View Article : Google Scholar
|
|
24
|
Chen JN, Liu Z, Wang ZJ, Mei SW, Shen HY,
Li J, Pei W, Wang Z, Wang XS, Yu J and Liu Q: Selective lateral
lymph node dissection after neoadjuvant chemoradiotherapy in rectal
cancer. World J Gastroenterol. 26:2877–2888. 2020.PubMed/NCBI View Article : Google Scholar
|
|
25
|
Zhou S, Zhang H, Liang J, Fu W, Lou Z,
Feng B, Yang Y, Xie Z and Liu Q: Chinese Lateral Node Collaborative
Group. Feasibility, indications, and prognostic significance of
selective lateral pelvic lymph node dissection after preoperative
chemoradiotherapy in middle/low rectal cancer: Results of a
multicenter lateral node study in China. Dis Colon Rectum.
67:228–239. 2024.PubMed/NCBI View Article : Google Scholar
|
|
26
|
Kim MJ, Kim TH, Kim DY, Kim SY, Baek JY,
Chang HJ, Park SC, Park JW and Oh JH: Can chemoradiation allow for
omission of lateral pelvic node dissection for locally advanced
rectal cancer? J Surg Oncol. 111:459–464. 2015.PubMed/NCBI View Article : Google Scholar
|
|
27
|
Rooney S, Meyer J, Afzal Z, Ashcroft J,
Cheow H, De Paepe KN, Powar M, Simillis C, Wheeler J, Davies J and
Joshi H: The role of preoperative imaging in the detection of
lateral lymph node metastases in rectal cancer: A systematic review
and diagnostic test meta-analysis. Dis Colon Rectum. 65:1436–1446.
2022.PubMed/NCBI View Article : Google Scholar
|
|
28
|
Hoshino N, Murakami K, Hida K, Sakamoto T
and Sakai Y: Diagnostic accuracy of magnetic resonance imaging and
computed tomography for lateral lymph node metastasis in rectal
cancer: A systematic review and meta-analysis. Int J Clin Oncol.
24:46–52. 2019.PubMed/NCBI View Article : Google Scholar
|
|
29
|
Mizukami Y, Ueda S, Mizumoto A, Sasada T,
Okumura R, Kohno S and Takabayashi A: Diffusion-weighted magnetic
resonance imaging for detecting lymph node metastasis of rectal
cancer. World J Surg. 35:895–899. 2011.PubMed/NCBI View Article : Google Scholar
|
|
30
|
Laparoscopic Surgery Committee of the
Endoscopist Branch in the Chinese Medical Doctor Association
(CMDA); Laparoscopic Surgery Committee of Colorectal Cancer
Committee of Chinese Medical Doctor Association (CMDA); Colorectal
Surgery Group of the Surgery Branch in the Chinese Medical
Association (CMA); Chinese Anti-Cancer Association Colorectal Tumor
Integrated Rehabilitation Committee; China International Exchange
and Promotive Association for Medical and Health Care Colorectal
Disease Branch. Chinese expert consensus on the diagnosis and
treatment for lateral lymph node metastasis of rectal cancer (2024
edition). Zhonghua Wei Chang Wai Ke Za Zhi. 27:1–14.
2024.PubMed/NCBI View Article : Google Scholar : (In Chinese).
|