|
1
|
Sung H, Ferlay J, Siegel RL, Laversanne M,
Soerjomataram I, Jemal A and Bray F: Global cancer statistics 2020:
GLOBOCAN estimates of incidence and mortality worldwide for 36
cancers in 185 countries. CA Cancer J Clin. 71:209–249. 2021.
View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Pashayan N, Antoniou AC, Ivanus U,
Esserman LJ, Easton DF, French D, Sroczynski G, Hall P, Cuzick J,
Evans DG, et al: Personalized early detection and prevention of
breast cancer: ENVISION consensus statement. Nat Rev Clin Oncol.
17:687–705. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Xia C, Basu P, Kramer BS, Li H, Qu C, Yu
XQ, Canfell K, Qiao Y, Armstrong BK and Chen W: Cancer screening in
China: A steep road from evidence to implementation. Lancet Public
Health. 8:e996–e1005. 2023. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Santen RJ and Yue W: Cause or prevention
of breast cancer with estrogens: Analysis from tumor biologic data,
growth kinetic model and Women's Health Initiative study.
Climacteric. 22:3–12. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Martei YM, Dauda B and Vanderpuye V:
Breast cancer screening in sub-Saharan Africa: A systematic review
and ethical appraisal. BMC Cancer. 22:2032022. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
The Society of Breast Cancer China
Anti-Cancer Association, Breast Oncology Group of the Oncology
Branch of the Chinese Medical Association, . Guidelines for breast
cancer diagnosis and treatment by China Anti-cancer Association
(2024 edition). China Oncol. 33:1092–1187. 2023.(In Chinese).
|
|
7
|
Ahmed M and Kabel: Tumor markers of breast
cancer: New prospectives. J Oncol Sci. 3:5–11. 2017. View Article : Google Scholar
|
|
8
|
Guo W, Lu X, Liu Q, Zhang T, Li P, Qiao W
and Deng M: Prognostic value of neutrophil-to-lymphocyte ratio and
platelet-to-lymphocyte ratio for breast cancer patients: An updated
meta-analysis of 17079 individuals. Cancer Med. 8:4135–4148. 2019.
View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Oktay K, Santaliz-Casiano A, Patel M,
Marino N, Storniolo AMV, Torun H, Acar B and Madak Erdogan Z: A
Computational statistics approach to evaluate blood biomarkers for
breast cancer risk stratification. Horm Cancer. 11:17–33. 2020.
View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Jørgensen N, Lænkholm AV, Sækmose SG,
Hansen LB and Hviid TVF: Peripheral blood immune markers in breast
cancer: Differences in regulatory T cell abundance are related to
clinical parameters. Clin Immunol. 232:1088472021. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Fang Q, Tong YW, Wang G, Zhang N, Chen WG,
Li YF, Shen KW, Wu BW and Chen XS: Neutrophil-to-lymphocyte ratio,
obesity, and breast cancer risk in Chinese population. Medicine
(Baltimore). 97:e116922018. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Said NM: Three gold indicators for breast
cancer prognosis: A case-control study with ROC analysis for novel
ratios related to CBC with (ALP and LDH). Mol Biol Rep.
46:2013–2027. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Zhou Q, Dong J, Sun Q, Lu N, Pan Y and Han
X: Role of neutrophil-to-lymphocyte ratio as a prognostic biomarker
in patients with breast cancer receiving neoadjuvant chemotherapy:
A meta-analysis. BMJ Open. 11:e0479572021. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Liu Y, He M, Wang C, Zhang X and Cai S:
Prognostic value of neutrophil-to-lymphocyte ratio for patients
with triple-negative breast cancer: A meta-analysis. Medicine
(Baltimore). 101:e298872022. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Cullinane C, Creavin B, O'Leary DP,
O'Sullivan MJ, Kelly L, Redmond HP and Corrigan MA: Can the
neutrophil to lymphocyte ratio predict complete pathologic response
to neoadjuvant breast cancer treatment? A Systematic Review and
Meta-analysis. Clin Breast Cancer. 20:e675–e681. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Alizamir A, Dehghan Azad S, Pirdehghan A
and Moradi A: Preoperative neutrophil: Lymphocyte ratio, platelet:
Lymphocyte ratio, and C-reactive protein levels predictive value in
determining the severity of breast mass. Iran J Pathol. 17:413–418.
2022. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Sun H, Yin CQ, Liu Q, Wang F and Yuan CH:
Clinical significance of routine blood test-associated inflammatory
index in breast cancer patients. Med Sci Monit. 23:5090–5095. 2017.
View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Nøst TH, Alcala K, Urbarova I, Byrne KS,
Guida F, Sandanger TM and Johansson M: Systemic inflammation
markers and cancer incidence in the UK Biobank. Eur J Epidemiol.
36:841–848. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Dal F, Ökmen H, Ulusan K, Havare SB, Orhan
B, Çolak Ş, Ferlengez E and Sari S: Hemogram index parameters in
the evaluation of male breast cancer and inflammatory response: A
case-control study. Rev Assoc Med Bras. 68:94–99. 2022. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Velidedeoglu M, Kundaktepe BP, Aksan H and
Uzun H: Preoperative fibrinogen and hematological indexes in the
differential diagnosis of idiopathic granulomatous mastitis and
breast cancer. Medicina (Kaunas). 57:6982021. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Seretis C, Seretis F, Lagoudianakis E,
Politou M, Gemenetzis G and Salemis NS: Enhancing the accuracy of
platelet to lymphocyte ratio after adjustment for large platelet
count: A pilot study in breast cancer patients. Int J Surg Oncol.
2012:6536082012.PubMed/NCBI
|
|
22
|
Li N, Cao L, Zhao K and Feng Y:
Development and validation of a nomogram to predict Chinese breast
cancer risk based on clinical serum biomarkers. Biomark Med.
17:273–286. 2023. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
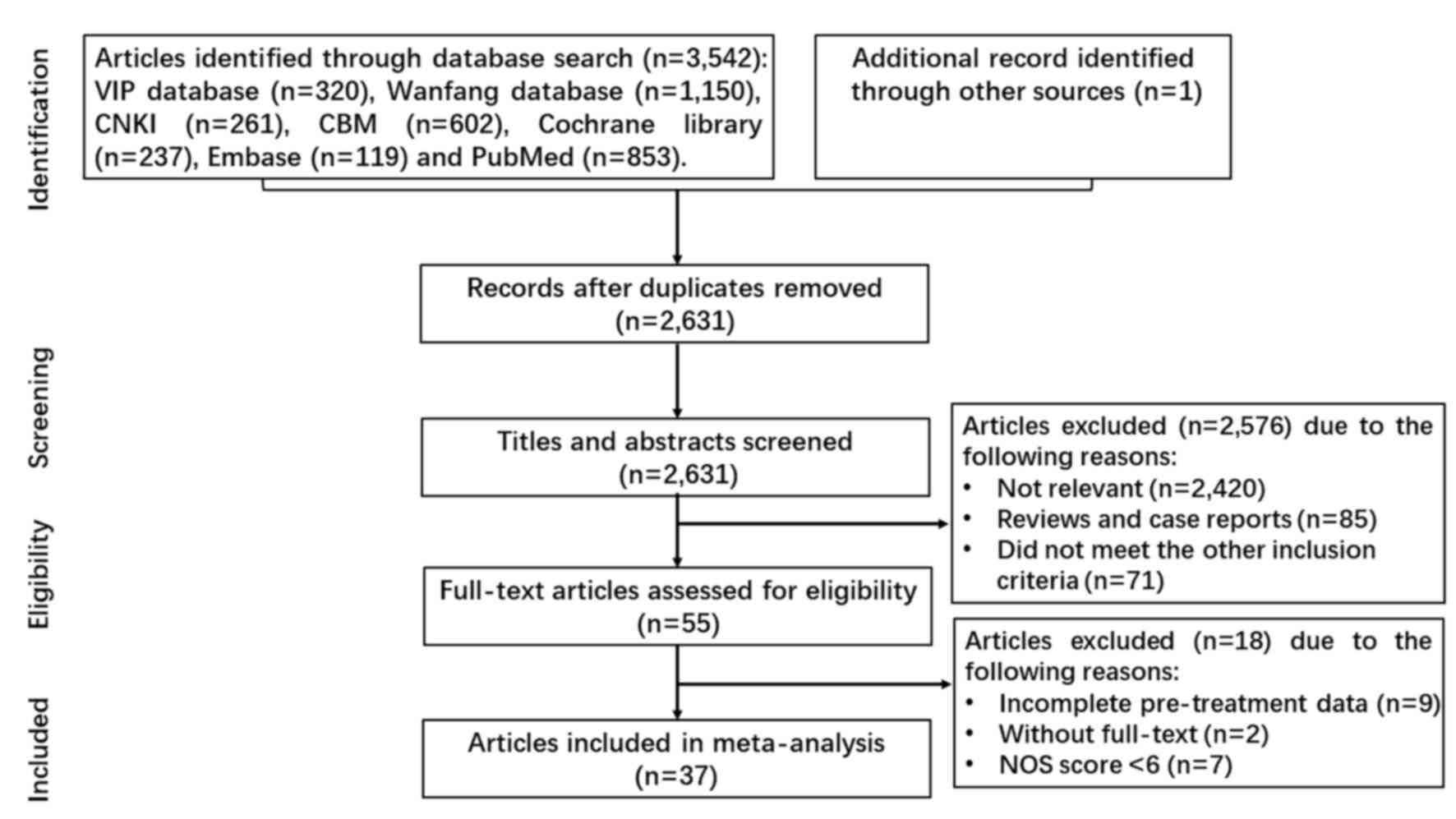
Page MJ, McKenzie JE, Bossuyt PM, Boutron
I, Hoffmann TC, Mulrow CD, Shamseer L, Tetzlaff JM, Akl EA, Brennan
SE, et al: The PRISMA 2020 statement: An updated guideline for
reporting systematic reviews. BMJ. 372:n712021. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Jiang Y, Xu D, Song H, Qiu B, Tian D, Li
Z, Ji Y and Wang J: Inflammation and nutrition-based biomarkers in
the prognosis of oesophageal cancer: A systematic review and
meta-analysis. BMJ Open. 11:e0483242021. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Bhadauria US, Purohit B, Nilima N and
Priya H: Oral health in individuals with bleeding disorders: A
systematic review and meta-analysis. Haemophilia. 30:658–670. 2024.
View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Deeks JJ and Higgins JPT; Altman DG
(eds.); on behalf of the Cochrane Statistical Methods Group, :
Chapter 10: Analysing data and undertaking meta-analyses In:
Cochrane Handbook for Systematic Reviews of Interventions.
https://training.cochrane.org/handbook/current/chapter-10#section-10-10-4-1August
22–2023
|
|
27
|
Rimini M, Casadei-Gardini A, Ravaioli A,
Rovesti G, Conti F, Borghi A, Dall'Aglio AC, Bedogni G, Domenicali
M, Giacomoni P, et al: Could inflammatory indices and metabolic
syndrome predict the risk of cancer development? Analysis from the
bagnacavallo population study. J Clin Med. 9:11772020. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Ozyalvacli G, Yesil C, Kargi E, Kizildag
B, Kilitci A and Yilmaz F: Diagnostic and prognostic importance of
the neutrophil lymphocyte ratio in breast cancer. Asian Pac J
Cancer Prev. 15:10363–10366. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Okuturlar Y, Gunaldi M, Tiken EE, Oztosun
B, Inan YO, Ercan T, Tuna S, Kaya AO, Harmankaya O and Kumbasar A:
Utility of peripheral blood parameters in predicting breast cancer
risk. Asian Pac J Cancer Prev. 16:2409–2412. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Qian P, Yun HZ, Zhu L and Zhang YY: The
value of inflammatory markers in preoperative diagnosis and
prognostic evaluation of breast cancer. Lab Med Clin. 12:3765–3767.
2015.
|
|
31
|
Weiwei Z, Linlin X, Xiufen L, You P, Huang
dingding, Yuping W and Jing F: Preoperative peripheral blood
neutrophil-to-lymphocyte ratio in the diagnosis of breast cancer.
Lab Med. 33:209–212. 2018.(In Chinese).
|
|
32
|
Yan X, Zhang HZ, Yan J, Peng HW and Wu X:
The value of preoperative peripheral blood NLR in the differential
diagnosis of benign and malignant breast masses. Jiangsu Med J.
45:638–641. 2019.(In Chinese).
|
|
33
|
Tao C, Mingming Y and Zhiqi H: Application
value of preoperative peripheral blood multi-index combined
detection and analysis in the diagnosis of breast cancer. Chin J
Cancer Prev Treat. 27:730–734. 2020.(In Chinese).
|
|
34
|
Peng F, Luo P and Li L: Correlation
analysis of preoperative inflammatory indicators and
clinicopathological features in breast cancer patients. J Bengbu
Med Coll. 46:1208-1211-1215. 2021.(In Chinese).
|
|
35
|
Divsalar B, Heydari P, Habibollah G and
Tamaddon G: Hematological parameters changes in patients with
breast Cancer. Clin Lab. 672021.PubMed/NCBI
|
|
36
|
Wang K, Zhang P, Su B, Wang H, Dong X and
Yang Q: Analysis of blood routine test and PLR, NLR, LMR in breast
cancer patients. Lab Med Clin. 19:84–89. 2022.(In Chinese).
|
|
37
|
Zou H, Liu SH, Yang R, Wu XJ, Cao YP and
Huang HF: Combination of Neutrophil-to-Lymphocyte ratio and red
cell distribution width with serum tumor markers for the
differential diagnosis of breast cancer and its association with
pathological features and molecular types. Clin Breast Cancer.
22:e526–e535. 2022. View Article : Google Scholar : PubMed/NCBI
|
|
38
|
Guo M, Bai Y and Zhang J: Application of
peripheral blood NLR expression level in the adjuvant diagnosis of
breast cancer. Systems Medi. 7:14–17+22. 2022.
|
|
39
|
Tang CL, Li Y and Zhang XF: Diagnostic
value of preoperative neutrophil lymphocyte count ratio combined
with carbohydrate antigen 153 in breast cancer. Lab Med Clin.
38:237–240. 2023.(In Chinese).
|
|
40
|
Schober P, Mascha EJ and Vetter TR:
Statistics from A (Agreement) to Z (z Score): A Guide to
interpreting common measures of association, agreement, diagnostic
accuracy, effect size, heterogeneity, and reliability in medical
research. Anesth Analg. 133:1633–1641. 2021.PubMed/NCBI
|
|
41
|
Youssry S, Hussein A, Ramadan R,
Alkarmouty A and Elsheredy A: The association of human
cytomegalovirus with biomarkers of inflammation and immune
activation in breast cancer. Breast Dis. 41:229–239. 2022.
View Article : Google Scholar : PubMed/NCBI
|
|
42
|
Velizarova M, Yacheva T, Genova M and
Svinarov D: Evaluation of automated hematology analyzer DYMIND DH76
compared to SYSMEX XN 1000 system. J Med Biochem. 40:367–377. 2021.
View Article : Google Scholar : PubMed/NCBI
|
|
43
|
Zhang H, Zhao R, Gu G, Wu L, Li X, Huang B
and Peng Q: Change and significance of partial peripheral blood
biochemical indicators in breast cancer patients. Lab Med Clin.
13:2153–2155. 2016.(In Chinese).
|
|
44
|
Wei W, Wen T, Xin M, Shaoping S, Yongliang
Z and Yanjun Z: Diagnostic value of neutrophil lymphocyte ratio for
intraductal papillary neoplasms of breast. Acad J Chin PLA Med Sch.
38:628–630+661. 2017.
|
|
45
|
Yu H, Xushan C, Jiajun J and Chunli Z: The
Predictive value of preoperative neutrophil-to lymphocyte ratio for
breast cancer and its relationship with Beclin1. Lab Med Clin.
15:3667–3669+3673. 2018.
|
|
46
|
Zhenzhen P, Minmin Y, Yingge C, Jiuling D,
Meiqiu Y and Jianli G: Abnormal granulocyte differentiation and the
paradoxical switch of transforming growth factor-β1 in breast
cancer patients. J South Med Univ. 38:856–860. 2018.
|
|
47
|
Cao L, Peng X, Jin L and Su Z: Clinical
significance of peripheral blood related indexes in patients with
breast cancer. Medicine and Health 4. 192018.(In Chinese).
|
|
48
|
Lulu Z, Yun L, Wenbing D, Wen T, Xiaoying
L, Wanhui Z and Bingchang Z: Diagnostic values of peripheral blood
indexes and tumor markers for breast cancer. China Med. 13:421–425.
2018.
|
|
49
|
Tianhua Z, Wenqiang W, Zhenhui C and
Xiaoping M: Clinical significance of preoperative platelet to
lymphocyte ratio and red cell distribution width in patients with
breast cancer. Hainan Med J. 29:2284–2287. 2018.
|
|
50
|
Pei Y and Qian YQ: Analysis of the
relationship between body mass index, neutrophil-to-lymphocyte
ratio and the risk of breast cancer. Baojianwenhui. 9:226–227.
2019.(In Chinese).
|
|
51
|
Alsaadi JHH and Younus BM: Study of some
biochemical and blood parameters as screening markers for breast
cancer patients before adjuvant therapy in Thi Qar
Government-southern Iraq. J Global Pharma Technol. 11:236–244.
2009.
|
|
52
|
Xiaolin X, Xiaoqun Y, Menglu L and Bing L:
Analysis of hematological indexes and clinical features i breast
cancer patients. Hainan Med J. 30:186–188, (In Chinese).
|
|
53
|
Gao X, Yin J, Wang X, Petersen F and Yu X:
A comprehensive comparison of hematological parameters among 39
common diseases. Scand J Clin Lab Invest. 79:251–259. 2019.
View Article : Google Scholar : PubMed/NCBI
|
|
54
|
Congfang L, Baoxiang W, Yuhui W, Zhi X,
Wei Z and Sufang W: Relationship between NLR, PLR and breast
cancer. J Clin Res. 37:1184–1187. 2020.(In Chinese).
|
|
55
|
Baselice S, Castaldo R, Giannatiempo R,
Casaretta G, Franzese M, Salvatore M and Mirabelli P: Impact of
breast tumor onset on blood count, Carcinoembryonic antigen, cancer
antigen 15-3 and lymphoid subpopulations supported by automatic
classification approach: A pilot study. Cancer Control.
28:107327482110486122021. View Article : Google Scholar : PubMed/NCBI
|
|
56
|
Meng X, Bo S and Hongquan C: Changes of
some peripheral blood indexes and diagnostic value of serum CA125,
CA153 and CEA in patients with breast cancer. Chinese Foreign Med
Res. 20:66–70. 2022.(In Chinese).
|
|
57
|
Ding H, Xu J, Wang F, Zhang Q, Pan H, Mu
Y, Gu CR, Miao SX, Li XN, Ju HY, et al: Differential diagnosis
model of benign and malignant breast BI-RADS category 4 nodules
based on serum SP70 and conventional laboratory indicators. Chin J
Prev Med. 56:1774–1783. 2022.(In Chinese).
|